RESPIRATORY FAILURE-EVALUATION AND MANAGEMENT
advertisement
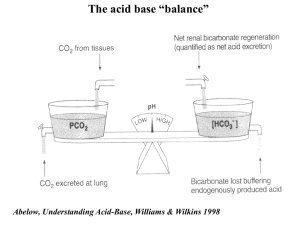
RESPIRATORY FAILURE-EVALUATION AND MANAGEMENT Dr Binila Chacko Associate Professor Medical ICU, CMC Vellore DR THOMAS COGAN DR WILLIAM HOWES RESPIRATION CELLULAR RESPIRATION TRANSPORT OF GASES VENTILATION DEFINITION Failure of the lung to maintain adequate gas exchange Abnormalities of arterial blood gas tensions. PaO2 < 60 mmHg with or without hypercarbia PaCO2 > 46 mmHg Onset usually acute or sub-acute WHY IS THIS TOPIC IMPORTANT • • Common problem 360,000 cases per year United States • 36% die during hospitalization • Estimated that respiratory failure will become more common as the population ages, increasing by as much as 80 percent in the next 20 years PHYSIOLOGY PACEAMAKER PUMP Increased airway resistance Decreased lung compliance Resistance REDUCECompliance PUMP EFFICIENCY INCREASE WORK OF BREATHING GAS EXCHANGER FACTORS AFFECTING EFFICIENCY OF GAS TRANSFER Alveolar capillary interface Transit time of blood in the pulmonary capillaries 0.7seconds PaO2 PAO2 Alveolar partial pressure of oxygen Diffusing capacity Ventilation-perfusion matching PAO2 determinants Alveolar pressure Alveolar gas equation Alveolar PAO2=(FiO2 x713)-PACO2/R pressure=PAO2+PACO2+PA(H20)+PA N2 FiO2 PACO2 PaO2 PAO2 Diffusing capacity Transit time in the pulmonary capillaries-0.7seconds Alveolar capillary interface Increase in thickness Since CO2 diffusion 20 times that of oxygen usually hypoxemia unless there is ventilatory failure PaO2 PAO2 Diffusing capacity Ventilation-perfusion matching Normal alveolar ventilation (V) about 4 to 6 L, Perfusion (cardiac output, Q) about 5 L Normal V/Q=0.8-1.2 V/Q matching Intracardiac/intr apulmonary Anatomical/ physiological Predominant hypoxemia Predominant hypercarbia PaO2 quick recap PAO2 Alveolar pressure, FiO2 and the PaCO2 Diffusing capacity Alveolar capillary membrane and time across pulmonary capillaries Ventilation-perfusion matching Dead space and shunt effect Carbon dioxide outflow Dependent on alveolar ventilation Resp rate x (VT-VD) Respiratory rate Tidal volume Ventilation-perfusion matching VT=Tidal volume VD=Dead space Again shows the importance of V/Q matching in carbon dioxide regulation TYPES Physiological approach Type 1 and 2 Pathophysiological approach Types 1 to 4 TYPES SHUNT Hypoxemic/type I respiratory failure Hypercapnic/typ e II respiratory failure IN AN UNWELL PATIENT CLINICAL EXAMINATION HAPPEN IN PARALLEL MANAGEMENT Clinical assessment TO ASSESS SEVERITY TO DETERMINE THE CAUSE Clinical assessment RESPIRATORY COMPENSATION RESPIRATORY COMPENSATION SYMPATHETIC STIMULATION RESPIRATORY COMPENSATION RESPIRATORY SYMPATHETIC TACHYPNEA WORRY COMPENSATION STIMULATION IF TACHYCARDIA SYMPATHETIC STIMULATION USE SYMPATHETIC OFTISSUE ACCESSORY RR >30/MIN HYPOXIA STIMULATION MUSCLES HYPERTENSION TISSUE HYPOXIA CAN’T SYMPATHETIC ALTERED SPEAK TISSUE MENTAL IN HYPOXIA FULL STIMULATION STATUS SENTENCES SWEATING HEMOGLOBIN DESATURATION SHOCK-DECREASED HEMOGLOBIN AGITATED/CONFUSED TISSUE DESATURATION HYPOXIA ORGAN PERFUSION TISSUE HYPOXIA DETERIORATING HEMOGLOBIN CYANOSIS DESATURATION DESPITE THERAPY HEMOGLOBIN DESATURATION To determine the cause… APPLYING PHYSIOLOGY TO PATHOLOGY Approach to Type I respiratory failure Hypoxemia reduction in oxygen in the blood-low PaO2 Hypoxia reduction in oxygen in the tissues LOW PaO2 =HYPOXEMIA Low PAO2 Overdistended alveoli(Intrinsic/extrinsic-PEEP) Decreased blood supply-Pulmonary Alveolar capillary embolism/Shock Alveolar disease (fluid/pus/protein/bloo d) Intra-pulmonary shunting collapsed lung (atelectasis) MUST REMEMBER More than one pathophysiological process may co-exist. Pure diffusion abnormalities are uncommon. WHAT’S THE NEXT STEP? Find out where the abnormalty is Pa CO2 A-a gradient A-a gradient Low PaO2 Is the CO2 increased ? Yes No A-a gradient Is the A-a gradient increased ? No Yes Response to oxygen therapy Yes V/Q mismatch Alveolar disease Interstitial disease Diffusion problems Pulmonary embolism Low inspired FiO2 No Shunt Increased Normal - pure hypoventilation Approach to hypercapnic respiratory failure Increased CO2 production Increased CO2 production Increased muscle activity (spasms, convulsions) Reduced CO2 elimination Hyper metabolicCO states (fever, sepsis) Increased production 2 CONTROLLER-BRAIN/SPINAL CORD/NMJ Carbohydrate rich feeds. Reduced CO2 elimination HYPERCAPNIA OCCURS ONLY IF CO2 ELIMINATION CANNOT KEEP PACE WITH PUMP PRODUCTION ALVEOLOCAPILLARY UNIT Reduced CO2 elimination Reduced elimination High CO2 Increased production Is the A-a gradient increased? No Yes Pure hypoventilation Response to oxygen therapy PI Max Yes V/Q mismatch Alveolar disease Interstitial disease Diffusion problems Pulmonary embolism No Shunt Low Neuromuscular problem Normal Central hypoventilation syndrome Don’t forget to look at the pH • PaCO2 must always be considered in relation to the pH. • Acute hypercapnic respiratory failure • Shift in the pH, • Compensatory mechanisms take time • Chronic hypercapnic respiratory failure • pH is usually close to normal, Management of hypoxemic respiratory failure • treatment of the underlying cause (specific • • • treatment) improving oxygen delivery to the tissues limiting potentially damaging therapies reducing tissue oxygen demand. Management of hypoxemic respiratory failure treatment of the underlying cause (specific treatment) improving oxygen delivery to the tissues DO2 = [1.39 x Hb x SaO + (0.003 x PaO )] x Q Hb SaO2 Increase FiO2 PaO2 PEEP Cardiac index 2 2 Improving oxygen delivery • • Target is to maintain cerebral oxygenation Increase FiO2 • FiO2 start with 100% (unless COPD) and reduce FiO2 based on ABG (P/F ratios) • Apply extrinsic PEEP - “Open lung ventilation” (can be done by invasive MV or NIV) • Physiological goal of preventing alveolar collapse Oxygen delivery devices Performance Variable Flow Flow Low the flowoxygen concentration of the air-oxygen mix reaching the alveoli is not constant deliver oxygen less than PIFR Performance Fixed High flow not influenced by respiratory rate, deliver oxygen at flow rates size of the reservoir or oxygen flow higher than PIFR rate Oxygen delivery devices Management of hypoxemic respiratory failure treatment of the underlying cause (specific treatment) improving oxygen delivery to the tissues limiting potentially damaging therapies Lung protective ventilatory strategies reducing tissue oxygen demand. control of fever, sepsis or seizures ventilatory support offloads the respiratory muscles Alveolar recruitment Increase tidal volumes (increase distending pressures) - keep alveoli open Increase inspiratory time Increase PEEP How much tidal volume? Landmark NIH NHLBI ARDS network Prospective, randomized, multi-center trial of 12 ml/kg vs 6 ml/kg tidal volume positive pressure ventilation for treatment of acute lung injury and acute respiratory distress syndrome 861 patients The Acute Respiratory Distress Syndrome Network: Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 2000, 342:1301– 1308 OPTIMAL PEEP SETTING Staircase recruitment manouvre Defined as the lowest PEEP attainable without causing a significant drop (>10%) in PaO2 ARDSNet protocol No agreed upon method of determination Thoracic tomography • Higher than the lower infection point on a pressurevolume loop Oesophageal balloon directed estimation of pleural pressures to calculate transpulmonary pressures and guide PEEP titration How do you set PEEP? • LIP is that point of the curve where the slope of the line changes significantly. • Believed to represent the opening of majority of alveoli How do you set PEEP? Benefits of PEEP Increases transpulmonary distending pressures Displaces edema fluid into interstitium Decreases atelectasis Decrease in right to left shunt Improved compliance Improved oxygenation Whom should I ventilate? Decision to ventilate Complex Multifactorial No simple rules Severity of respiratory failure Cardiopulmonary reserve Adequacy of compensation Ventilatory requirement Underlying disease Treatment already given Risks of mechanical ventilation Always consider .. Different clinical situations Mild hypoxemia (PaO2 60 – 70 mmHg on room air) a nasal cannula or a simple mask may be sufficient. Moderate hypoxemia (PaO2 50-60 mmHg) a partial re-breather mask or venturi device latter preferred for COPD patients. Severe hypoxemia (PaO2 <50 mmHg) not responding to simpler devices non-rebreather systems (e.g. CPAP, non-invasive ventilation, Ambu-bag, Bains) Invasive mechanical ventilation Specific to management of hypercapnic respiratory failure Reduce CO2 production controlling fever and excess motor activity (convulsions) Reducing carbohydrate intake. (R.Q Carbohydrates 1.0 and for fat is 0.7) Particularly important for COPD To enhance CO2 elimination.. Respiratory drive can be increased Reducing the use of sedation Drugs that increase respiratory drive (COPD) acetazolamide, medroxy-progesterone acetate Benefit not proven in randomized trials Ventilation-GOAL TO INCREASE ALVEOLAR VENTILATION HYPERCARBIA DUE TO LOSS OF PROGRESSIVE Improve Lung mechanics P ABCDE HYPOXIA KILLS!! P- propping up A-Analgesics to reduce chest pain B-Bronchodilators C-Compliance-ventilatory/non-ventilatory strategies D-Drugs such as xanthines E-Electrolyte correction IMPROVE LUNG MECHANICS HYPOXIC DRIVE IS RARE Always consider .. NIV COPD The number needed to be treated for benefit N=8 patients to save one life N=5 to avoid one invasive mechanical ventilation N=3 to avoid “a” complication of ventilation Milder exacerbations Evidence not clear Post hoc analysis suggest benefit below pH of 7.37 and PaCO2 of > 55 mm Hg NIV COPD Failure rates in COPD exacerbations about 25% Early failure predictors are lack of improvement in pH no change in the level of consciousness no improvements in CO2 levels worsening respiratory rate NIV APO CPAP appears to be superior to bi-level ventilation in terms of mortality (NNT 10 for CPAP) Similar benefits of both CPAP and bilevel ventilation in reducing need for mechanical ventilation (NNT 6 for CPAP and 7 for bilevel) Failure of NIV When do you say treatment has failed? Complications have occurred PaO2 continues to be low PaCO2 continues to be elevated is the patient on too much oxygen? Is there excessive leakage in the circuit? Are the ventilatory supports adequate (IPAP & EPAP)? Is there patient-ventilator asynchrony? Is re-breathing occurring May need IMV CASE 43 year old man Community acquired pneumonia Day 1 antibiotics PaO2 60mmHg, Pa CO2 30mmHg, pH 7.15 on 15L/min oxygen Respiratory rate 35/min Agitated RECAP Investigations (clinical and lab) and management happen in parallel PaO2 - PAO2, Alveolocapillary diffusion and V/Q abnormalities PaCO2- Alveolar ventilation Hypoxemia PaCO2 A-a gradient Response to increase in FiO2 Decide on therapy-Non invasive versus invasive mechanical ventilation Lung protective ventilation