Envisioning Collaborative Relationships
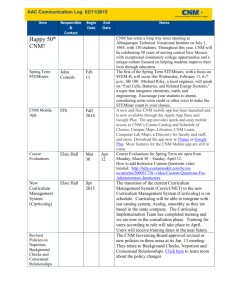
advertisement

Envisioning Collaborative Relationships Among Midwives and Physicians, Institutions Seneca Falls October 11, 2013 Objectives After attending this lecture the participant should have increased knowledge and enhanced competence to • Identify current interdisciplinary collaborative models between Midwives and Physicians • Discuss the regulatory and socially ingrained barriers to successful collaboration for midwives in different practice settings such as academic, hospital-based, private practice and home • Use evidenced-based research to focus policies on outcomes • Identify practical steps to forging professional, functional and mutually satisfying relationships with physicians and other medical providers • Understand the opportunities for transformation of birth practices present today Ellen Biggers, MD, FACOG Disclosures • No potential conflict of interest • Mistaken for a midwife on several occasions Birth Carving 980 AD Angkor Wat, Cambodia Definition of Collaboration • American College of Nurse-Midwives, 2011. Collaboration is the process whereby a CNM/CM and physician jointly manage the care of a woman or newborn who has become medically, gynecologically or obstetrically complicated. • Webster’s – To work jointly with others or together especially in an intellectual endeavor Historical Perspective on Midwifery in the US • Midwives in colonial America were the dominant attendants at birth • Late 19th century: Obstetrics created as a medical specialty, physicians attended half of the nation’s births. Medical science advances • Early 20th century: hospitalization for birth increases, maternal and neonatal mortality begin to increase in and out of hospital History Continued • __ ________ ______ _________ – – – – _______ ___ ________ ________ _____ ________ __________ _______ ___ ______ ______ ___ __________ _____ ________ _______ __ _______ ____ – ________ ______ __________ __ ___________ ___________ ___ __ _________ ______ ________ _______ _____ __ ________ History continued • Mary Breckinridge founds Frontier Nursing Service in Kentucky in 1925 • 1931 The Lobenstein Clinic initiated a nursemidwifery education program to serve disadvantaged women in New York City • Nurse-midwifery grew slowly in poor communities both urban and rural and in home deliveries. (Tom) History Continued • 1960’s and 1970’s: California studies reveal improved outcomes with midwives in rural underserved areas. (Montgomery 1969 and Levy 1971) • 1971 ACNM, ACOG, and NAACOG approved a “Joint Statement on Maternity Care”. The first recognition of nurse-midwives by a medical organization (Rooks, 1997) • 1975 Revision of “Joint Statement” to clarify that an obstetrician’s presence is not required when care is rendered by a nurse-midwife History Continued • 1978 ACNM redefines nurse midwifery practice as “independent management of the antepartal, intrapartal, postpartal, and gynecological care of essentially normal women and their normal newborns” (Dawley & Varney, Burst 2005) • 2000 ACNM and ACOG define collaboration between CNMs and Ob/Gyns as one of “consultation, collaboration and referral” Collaboration • American College of Nurse-Midwives, 2011. Collaboration is the process whereby a CNM/CM and physician jointly manage the care of a woman or newborn who has become medically, gynecologically or obstetrically complicated. -Joint Committee definition: “The provision of healthcare by an interdisciplinary team of professionals who collaborate to accomplish a common goal, and is associated with increased efficiency, improved clinical outcomes, and enhanced provider satisfaction. Current Collaborative Models • Home Birth – In 1940 US, the percentage of out-of hospital births was 44% – In 2006, National Vital Statistics Report states there were 24,970 home births in the US or 0.59% – Prenatal consultation via phone or prenatal visit; external version for breech, borderline hypertension – Intrapartum or postpartum transfer to hospital CM or FP or OB Current Collaborative Models • Birthing Center – In 2006 there were 10,781 births in a freestanding birth center – Above collaboration – Multidisciplinary Team: Midwife, Obstetrician, Family Practitioner, Pediatrician, Nurses, Doulas – Policy and Protocol Development – Quality Assurance – Regulatory oversight at state and national level Current Collaborative Models • Community Hospital – National Vital Statistics Report: 4.3 million live births in US in 2006 – Above – Hospitalists/Laborists – Nurses, anesthesiologists, administrators – Hospital department level reporting – Education programs – Private practice CM, OB, or combined – Hospital-based practices – Financial arrangements – State agency oversight Current Collaborative Models • Tertiary Care Hospital – Maternal Fetal Medicine – Residents in OB, FP, ED – Various departments (Imaging, ED), Programscancer screening, Women’s Health Institute – Community of Hospitals Reporting, Education – Policy Making Committees Characteristics of Successful Models • Joint Committee Call for Papers (Waldman and Kennedy 2011) – Northwest Family Beginnings (Darlington, McBroom, Warwick, 2011) – Reasons for success • Legal framework of independent practice in Washington State – Limits vicarious liability for consulting Ob/Gyn • Clearly delineated scope of practice for each provider type Northwest Model • Institutional culture that supports collaboration – – – – In-house Ob/Gyn Regularly scheduled meetings between CNM and Ob/Gyn Family Practice and Licensed Midwife consultation Eventual Midwifery Dept: Institutional status, protection to practice independently and appropriate consultations » Shared-care model » On-call team » Patients attend prenatal visits in their own neighborhood » Guidelines developed jointly Licensed Midwives in Northwest Model • 1978 Marge Mansfield and Suzy Myers co-founded the Seattle Midwifery School, became dept of Midwifery at Bastyr University. Direct-entry 3 year Masters • Favorable provider insurance environment -1996 Malpractice available to LM with “every category of provider” legislation in Washington. Insurance contract availability – LM to CM transfer with ability to give doula support, resumes care upon discharge Northwest Definition of Collaboration • Consultation: CNM seeks the advice or opinion of Ob/Gyn. CNM maintains management responsibility for the client. MD does not typically meet patient • Comanagement: CNM and Ob/Gyn jointly manage care with CNM primary and MD has direct patient contact • Referral: the management of all or a very specific part of a client’s care is transferred to an Ob/Gyn who then assumes “hands-on” care and responsibility • Written care plan and roles* San Francisco General Hospital Hutchison, 2011 • “Great Minds Don’t Think Alike” -Shared commitment to excellence in both providing care to the underserved and training the next generation of physicians and nursemidwives • Mutual respect for differences in practice to capitalize on the expertise of each [type of provider] San Francisco General Hospital Hutchison, 2011 • Independent clinical caseloads, with patient choice in CNM or obstetric care • Shared commitment to improving care delivery systems • Clear lines of communication that include guidelines for consultation and collaboration • Faculty appointments for both obstetricians and CNMs • Interdependent responsibility for generating and managing finances San Francisco General Hospital Hutchison, 2011 • Interdisciplinary development of policy – Uniform use of evidenced-based practice – Serve on a variety of hospital committees – Quality assurance initiatives – Seat at the table • Interprofessional continuing education – Obstetric emergency simulation model – Philosophies of care and benefits of collaboration SFGH- Effects of Collaboration • Selective use of Episiotomy • Intermittent Auscultation • Centering Pregnancy: group-based model of prenatal care with Ob resident participation, model used for breast cancer, chronic pelvic pain and Mother-baby dyad groups • VBAC guidelines evidence-based candidate selection • Postpartum Hemorrhage prevention checklist • Consultation skill assessment for residents and CNM students SFGH- Challenges • • • • Safety, Autonomy and Power Ob not comfortable with CNM independence PROM management differences State required supervision of nurse-midwives by physicians in California Baystate Successful Collaborative Practice, (Dejoy, 2011) • Tertiary care, 4,000 births/year • CNMs have “broad, immediate, and responsive access to consultation and high-risk care” 3rd and 4th year residents are used for in-patients and attending Ob/Gyn for out-patients • Clear communication, written definitions of “philosophy, scope of practice, functions and organizational structure. Details of diagnostic tests and therapeutic agents that may be independently ordered by CNMs, conditions requiring consultation, collaboration, and referral. Baystate Successful Collaborative Practice • Midwifery practice serves a hospital-based office, four neighborhood health centers, and a correctional facility • Midwives provide triage for arriving patients with obstetric and gynecologic problems. CNM learned limited U/S, BPP, preterm labor evaluation • Midwives have primary responsibility for teaching normal obstetrics and triage to first-year residents and medical students. Ob Team CNM Baystate Successful Collaborative Practice • CNM primary C/S 9% • VBAC rate 69%, overall dept rate 13.1 % and Massachusetts State 8.1% • Reduced episiotomy and laceration rates Baystate Successful Collaborative Practice • Detailed practice agreement • Open lines of communication • Understanding and accepting different philosophies • Trust Obstetrician and Nurse-Midwife Collaboration: Successful Public Health and Private Practice Partnership, Shaw-Battista, 2011 • Outcomes of collaborative maternity care for diverse population in a California community hospital • 74% of women received intrapartum CNM care • Few differences were seen in management or outcomes despite significant variation in demographic and clinical characteristics of public health clinic patients vs private practice Shaw-Battista 2011 • Private practice patients: older, less likely obese, more likely English speaking; more hydrotherapy, epidurals, and severe lacerations • Overall 12.5% Cesarean, less than a quarter used narcotics, epidural or hydrotherapy. Shaw-Battista, 2011 • Philosophy of extensive prenatal education, shared decision-making, and judicious use of obstetric interventions: – Optimal labor begins spontaneously – Labor is permitted to progress without intervention – Prenatal education about pharmacologic and nonpharmacologic pain relief methods – Obstetricians who firmly believe in collaborative practice model Shaw-Battista, 2011 – Evidenced based guidelines developed collaboratively – Ample hands-on support from nurses, CNM, and doulas Shaw-Battista, 2011 • Challenges: – CNM view childbirth as a physiologic process requiring supportive care – Ob view childbirth as process to be managed to avoid illness and pathology – Inter-professional consensus on guidelines is timeintensive and therefore expensive – Patient-centered model respects woman’s right to decline recommended care Barriers to Collaboration • Educational differences – Level of degree • Institutionalized discrimination – Hierarchical system – Focus on problem cases not overall outcomes – Legal definitions of relationships between providers – Insurance companies – Hospital departments Barriers to Collaboration • • • • • Professional competition Ineffective communication Gender issues Social class Medical malpractice – Vicarious liability – Mandates practice composition – Limits to scope of practice Barriers to Collaboration • International Collaboration – Australia in an attempt to mandate practice agreements met with complete opposition by obstetricians and lessened midwife autonomy – Canada RM are publicly funded, autonomous primary care providers, required to offer home and hospital birth. Limited acceptance especially in rural areas where the patient volume is smaller, doctors bill feefor-service, physician-staffed Medical Advisory Committees deny privileges to midwives (Munro, 2012) Peru Surgical Mission Characteristics of Successful Models • • • • • • • • Joint policy development Joint responsibility and accountability Joint education and team drills Peer review: interdependent independent practices Focused on patient outcomes Evidenced-based practice Shared work-load and improved outcomes lead to provider satisfaction Institutional recognition of autonomy of MW Normalizing Collaboration • Current opportunities – – – – – – – Affordable Care Act National Maternal Health Initiative Laborists, “Midwifilist” triage Maternal Fetal Medicine Obstetric resident education Consumer demand Information availability- shared guidelines, consents, transport plans, refusal of recommended treatment forms Opportunities • Institute of Medicine (2001,2010) – care provided by nurses safely reduces health care costs – critical to the availability and value of public and private clinical services Federal Health Reform: Implications & Opportunities • Increased ACNM visibility among policymakers, other health professions, White House, federal agencies, and Congress • Multiple new opportunities for ACNM member involvement, need for new taskforces, etc. • Potential for action on multiple issues including reimbursement, recognition as primary care providers, education funding, workforce issues, and issues directly affecting women and families (Avery, ACNM Focus on the Future, 2009) Normalizing Collaboration • Current opportunities – – – – – – – Affordable Care Act National Maternal Health Initiative Laborists, “Midwifilist” triage Maternal Fetal Medicine Obstetric resident education Consumer demand Information availability- shared guidelines, consents, transport plans, refusal of recommended treatment forms Normalizing Collaboration • Consensus to eliminate hierarchy – Clearly defined roles, lines of communication – Acknowledge history: Control, hostility, supervision, suppression, nursing dept, ego • Evidenced-based guidelines: resources • Interdisciplinary teams – Capitalizing on the strengths of each provider – Emergency Scenario Training – Joint Quality Assurance Normalizing Collaboration • Home birth – HBAC increasing – Consents for risks and benefits – Transport plans to hospital – Referral plans to CNM, MD, MFM – Acknowledge hostility: unilateral guidelines if necessary – WHO observation 82% of births world-wide are out-of-hospital. In US 1-2% Normalizing Collaboration Financial support for collaboration Educate obstetric and FP residents and midwives to consult and collaborate Midwife participation at all levels Shared work load Outcomes based assessments The End Legislative History NYSALM • 2003: NYS Legislature passed a bill adding Licensed Midwives to the list of providers who could order lab tests. • A.11649 / S.7658 Ch. 524 of 20042007: Physical Therapy bill added Licensed Midwives to the list of providers who could order physical therapy evaluation and treatment. • A.5515 / S.3490 (05-06)2008: A non-discrimination bill was passed that added Licensed Midwives to the list of providers who could not be denied hospital privileges solely based on class of licensure. We lobbied for this bill for seven years before its successful passage. • A.5505 / A.4019-A2010: The Midwifery Modernization Act amended the midwifery licensing law which had been passed in 1992. The MMA removed the requirement that midwives have a written practice agreement with a physician or hospital, and instead required that midwives advise their patients of what arrangements were in place in case the woman needed care beyond the scope of practice of the midwife. A.8117-B / S.5007-A Bibliography • Shaw-Battista J, Fineberg A, Boehler B, Skubic B, Wooley D, Tilton Z. Obstetrician and Nurse-Midwife Collaboration: Successful Public Health and Private Partnership. Obstet Gynecol 2011;663-72 • Darlington A, McBroom K, Warwick S. A Northwest Collaborative Practice Model. Obstet Gynecol 2011;673-7 • Hutchison MS, Ennis L, Shaw-Battista J, Delgado A, Myers K, Cragin L, Jackson RA. Great Minds Don’t Think Alike: Collaborative Maternity Care at San Francisco General Hospital. Obstet Gynecol 673-7 • DeJoy S, Burkman RT, Graves BW, Grow D, Sankey HZ, Delk C, Feinland J, Kaplan J, Hallisey A. Making It Work : Successful Collaborative Practice • Conry JA, Inaugural Speech, 64th President of ACOG. 2013 Bibliography • Garvey, M. Communication: ACNM and ACOG Issue Joint Statement on Collaboration, 2011 • Brocklehurst P. Perinatal and maternal outcomes by planned place of birth for healthy women with low risk pregnancies: the Birthplace in England national prospective cohort study. BMJ 2011;343/d7400 • Reiger KM, Lane KL. Working together: Collaboration between midwives and doctors in public hospitals. Aust Health Rev 2009; 33(2);315-324 • Miller, King, Lurie, Choitz. Certified nurse-midwife and physician collaborative practice. Piloting a survey on the Internet. J Nurse Midwifery 1997 Jul-Aug;42(4):308-15. • Ament, LA, Hanson, L. A model for the future. Certified nurse-midwives replace residents and house staff in hospitals. Nurs Health Care Perspect. 1998 Jan-Feb;19(1):26-33. • Waldman R, Powell Kennedy H. Collaborative Practice Between Obstetricians and Midwives. Obstet Gynecol 2011;503-4 Bibliography • Baldwin, LM, Hutchinson,H, Rosenblatt, RA. Professional Relationships between Midwives and Physicians: Collaboration or Conflict? Am J Public Health. 1992;82;262-264 • MacDorman, MF, Menaker, F. Trends and Charcteristics of Home and Other out-ofHospital Births in the United States, 19902006. National Vital Statistics Report, 2010;58:1-14 Bibliography • Gee, RE, Corry, MP. Patient Engagement and Shared Decision Making in Maternity Care. Obstet Gynecol 2012;120:995-997 • Munro, S., et al., Models of maternity care in rural environments: Barriers and attributes of interprofessional collaboration with midwives. Midwifery (2012), http://dx.doi.org/10.1016/j.midw.2012.06.00 4 Bibliography • Menasche,KA. Collaborative Practice between Certified Nurse-Midwives and Obstetricians and the Factors in Working Together to Normalize Childbirth: An Integrative Review, 2013 • DiVenere, L. Lay midwives and the ObGyn: Is collaboration risky? OBG Management, 2012;24