24th April 2012 - General Practice Income
advertisement
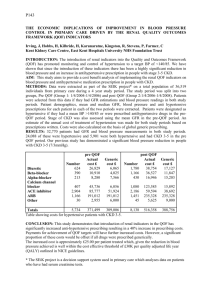
GP VTS Training Session 24th April 2012 General Practice Income Joanne Wales-Smith Aims Understand sources of GP income Understand structures that govern NHS income Practical look at maximising income in general practice Objectives Participants will be able to Identify sources of GP practice income Describe operating / contractual framework for NHS income Apply a service specification to a Practice situation Why important? GP Partner – personal income Efficiency of NHS income Effectiveness patients of resources for benefit of PRACTICE INCOME PRACTICE INCOME N H S I N C O M E Contract Global Sum Reports & Certificates Minimum Practice Income Guarantee (MPIG) QOF (Aspiration & Reward) £ Private Rental Income Teaching Income Seniority Private Services Enhanced Services Notional Rent & Service Charge Training Income N O N N H S …………. I N C O M E Contents Structure of NHS (& changes) GMS Contract PMS QOF Premises Income Training Income Enhanced Services * Structure of NHS Structure of NHS DoH 10 SHAs 152 Primary Care Trusts Primary Care Services Community Health Services Acute hospital trusts Mental health trusts Ambulance trusts Commercial providers & Voluntary organisations NHS Foundation Trusts GMS – the last version Red Book Item of service approach Per Doctor funding National framework only Contract between individual GP & DoH PMS? PMS Brought in as an alternative to the Red Book & old inflexible system Focused on special areas or needs Additional funding for additional work / responsibilities Contract between Practice & PCT Separate contractual & monitoring arrangements GMS – the new contract Set contractual framework nationally & ability to commission outside the framework for local needs NHS budget – weighted population basis Re-distribute Carr-Hill formula Factors involved: patient age and gender (used to reflect frequency of home and surgery visits) additional needs: Standardised Mortality Ratio and Standardised Long-Standing Illness for patients under the age of 65 years number of newly registered patients (generate 40% of work in 1st year) rurality costs of living in some area (ie South East - higher staff costs) patient age/gender for nursing/residential consultations. GMS – the new contract Set contractual framework nationally & ability to commission outside the framework for local needs Re-distribute NHS budget – weighted population basis Quality drive Out of Hours / GP recruitment Failed hospital contract Contract Structure Enhanced Services GMS Main Contract – global sum Enhanced Services Essential Services Additional Services* Enhanced Services QOF Enhanced Services Enhanced Services *Vacc & Imms 3% Key Aspects of nGMS Contract Contract between the Practice & the PCT The global sum allocation covers the payments PCTs will make to GMS practices as a contribution towards the contractors’ costs in delivering essential and additional services. The Minimum Practice Income Guarantee (MPIG) covers the payments PCTs will make to GMS practices to protect income levels in relation to some previous fees and allowances and is delivered through the correction factor. (no Practice worse off) “Global Sum Allocation Formula” QOF Enhanced Services local flavour & flexibility nGMS – income statement * * QOF QOF Quiz – how much do you know about the QOF? The Quality and Outcomes Framework (QOF) is the annual reward and incentive programme detailing GP practice achievement results. is a voluntary process for all surgeries in England and was introduced as part of the GP contract in 2004. awards surgeries achievement points for: managing some of the most common chronic diseases e.g. asthma, diabetes how well the practice is organised how patients view their experience at the surgery the amount of extra services offered such as child health and maternity services http://www.dh.gov.uk/en/Policyandguidance/Organisationpolicy/Primaryc are/Primarycarecontracting/QOF/index.htm * Example of a Clinical Indicator CHD Indicator 6 Example of an Organisational Indicator * GP Registrar Involvement Changes to the QOF 2012/13 the retirement of seven indicators (CHD13, AF4, QP1, QP2, QP3, QP4, QP5) releasing 45 points to fund new and replacement indicators the replacement of seven indicators with eight NICE recommended replacement indicators, focusing on six clinical areas namely Diabetes, Mental Health, Asthma, Depression, Atrial Fibrillation and Smoking the introduction of nine new NICE recommended clinical indicators, including two new clinical areas (Atrial Fibrillation, Smoking, PAD and Osteoporosis) the introduction of three new organisational indicators for improving Quality and Productivity which focus on accident and emergency attendances amendments to indicator wording for CHD9, CHD10, CHD14, STROKE12, DM26, DM27, DM28 and DEM3 inclusion of telephone reviews for Epilepsy 6. Premises Income Cost rent Notional rent Cost Rent The Cost Rent Scheme is no longer used. It previously existed for new extended or refurbished surgeries. The Cost Rent Scheme, as its name implies, is more closely associated to the costs involved, as opposed to the associated rental levels. Its purpose was to reimburse the cost of finance from providing new or considerably modified buildings. Notional Rent Re-imburse Doctors who own their surgery. The Notional Rent remuneration based on the Current Market Rental (CMR) value for the property i.e. what it would let for on the open market. District Valuer assesses for PCT. GPs can involve professional advisors. A primary factor affecting value is location. Training Income GP Registrars Training grant for Practice Educational grant for Trainers - £750 Salary & costs re-imbursed Medical Students Different payment structure for different years Groups of 4 students over 4 years – differing payments Enhanced Services Directed National Local • Enhanced services are services not provided through essential or additional services, • or essential and additional services delivered to a higher specified standard. • Key tool to help PCTs reduce demand on secondary care. Their main purposes are to expand the range of local services to meet local need, improve convenience and choice, and ensure value for money. They were designed to provide a major opportunity to expand and develop primary care, and give practices greater flexibility and the ability to control their workload. Directed Enhanced Services PCT has to commission these services for its population: Access (have to offer to GPs) IM&T (have to offer to GPs) Violent Patients Choose & Book Childhood Imms National Enhanced Services PCTs don’t have to commission Services commissioned to meet local need to national specifications and benchmark pricing. Other examples of NES are enhanced care of the homeless, more specialised services for multiple sclerosis and specialised care of patients with depression E.g. IUCD, Minor Injuries, NPT, Amber Drugs * Local Enhanced Services Up to the PCT what they commission, how much & how locally developed services designed to meet local health needs e.g. Wound Care North Yorkshire Enhanced Service Directory Examples of service specifications - Extended access - Minor surgery Any questions? Objectives Participants will be able to Identify sources of GP practice income Describe operating / contractual framework for NHS income Apply a service specification to a Practice situation