Planned GP contract changes 2013/2014 and beyond
advertisement

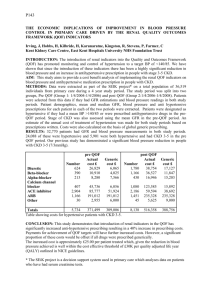
Planned GP contract changes 2013-2014 and beyond (Wales) Cardiff Tuesday 29th January Dr. David Bailey Chairman, GPC Wales Presentation outline Where are we? How did we get here? Outline of the changes Issues to consider – workload, quality and funding Changes to locum superannuation Redistribution of funding What can you do? What are we doing? Also coming our way… Questions and discussion Where are we? GPC Wales has decided to agree the latest offer on Welsh GP contracts Changes are significant and potentially disadvantageous (But significantly less so than England) Includes 1.5% resource uplift Insistence on eroding correction factor dropped GPCW has negotiated robustly to get what we think is the best deal possible Very different arrangements across the UK How did we get here? • June 2012 UK negotiations commence with NHSE • October 17th position reached which negotiators felt was reasonable • Rejected by governments (Scotland indicated still willing to negotiate) • October 2012 initial letter from WG • December 2012 - revised offer following discussions rejected – due to MPIG concerns • January 2013 new revised offer agreed Proposed contract changes Initial insistence on phasing out correction factor dropped Open discussions next year on reducing funding variability Implement most changes to QOF recommended by NICE, taking account of GPC concerns on some Reducing the time period for achieving most indicators from 15 to 12 months will not be introduced in Wales Proposed contract changes (2) Increase upper thresholds for some QOF indicators to match median achievement Remove some of the organisational domain = 969 point QOF Introduce new risk profiling QP domain Reform the QOF Contractor Population Index (CPI) New immunisations rotavirus added to childhood immunisations shingles for patients aged 70 Re-invest A&E QP points in GSE Why we should all be concerned: workload More box ticking - under-priced new work in QOF Shifting the goal posts - chasing points at QOF margins - However new training requirements and reduced timeframes NOT introduced in Wales Impact on access Impact on secondary care Why we should all be concerned: quality QOF Clinical problems with clinical QOF changes: Unworkable new indicators, unavailable services Changed blood pressure targets + higher thresholds polypharmacy Repetitive or inappropriate questioning Rise in exception reporting Less time for holistic patient care Risk profiling QP domain • Identify 5% of highest risk patients • Select 10% of those (0.5% of practice list) for multidisciplinary discussion and care plans • 47.5 points • 4 meetings • 1 page plan – medications, OOH summaries, carer contacts, allergies, preferred place of care • May well actually improve care Why we should all be concerned: funding Average practice 2014-2015, threshold QOF loss + organisational point loss = £2,000 (estimate) on thresholds + £6200 for recycled organisational points = £8200 Ameliorated by funding increase and can be earned back for new work but still represents new workload (and prices the new QOF indicators lower than would have happened in negotiation) Funding redistribution in Wales 450 practices are within £15 per weighted patient of each other Other 25 anything from £15-55 above average Some practices would be seriously destabilised, others would gain – Global sum only practices would all gain – Practices with small (less than 10%) correction factors would probably also gain a little – Higher correction factors would lose – the vast majority either small, rural, multi-site or odd demographics (university practices) These are exactly the practices where the Carr-Hill factors were altered by Westminster in 2003 Funding redistribution in Wales (2) • Commitment to model to practice level • Acknowledgement that some outliers may need off-formula solution • Recognition of the limitations of modified Carr-Hill • Commitment to consider rurality, smallness and multi-site practice • Commitment to negotiate not impose Changes to locum superannuation Responsibility for locum superannuation payments to move to practices Transfer of funds into Global Sum Equivalent to cover this (as this is all expenses) Practices use locums differently, likely to have disproportionate impact on small practices Likely to be bad for locums What can you do? Protect your patients – don’t chase targets that put your patients at risk or treat them inappropriately – protect patient care by saying NO to unresourced workload shift from secondary care Prioritise your practice – may need to reconsider involvement in optional work outside the practice particularly if full backfill costs not met What can you do? (2) Start to plan for the changes – look at the bottom line of your accounts not the top line and consider the cost of your services and work. Tell your AM or MP if patient services are adversely affected Engage all members of your practice, involve all GPs Be fair to your locums – pay promptly Keep up to date on the BMA website bma.org.uk/gpcontract What are we doing? Meeting the WG ministers and Civil servants regularly Talking to AMs Talking to patient groups Working with the media Gathering your views at road shows Developing guidance for GPs Preparing for the future Also coming our way… Health Inspectorate Wales scrutiny (but not charges) Revalidation Pension changes Secondary care dumping to meet efficiency targets Recruitment and retention crisis? Questions and discussion Remember: – Use the BMA website to understand the proposals in detail – Stay in touch with your LMC via their website and newsletters – Write to Health Minister and your AM. If these changes will hurt your practice, tell them. If MPIG funding proposals would damage patient care in your practice – tell them.