View &
advertisement

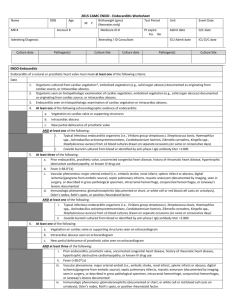
Supervisor : Dr: Mohammed Al marwala Presented by : Dr :Areej Aljabali Items of Presentation General definitions • Pathology • Pathogenesis • Pathophysiology • Clinical features • Diagnosis • Treatment • Prevention • Definition : Infective endocarditis is characterized by colonization or invasion of the heart valves or the mural endocardium by a microbe, leading to the formation of bulky friable vegetations composed of thromb and organisms, often associated with destruction of the underlying cardiac tissues. Acute ◦ Toxic presentation ◦ Progressive valve destruction & metastatic infection developing in days to weeks ◦ Most commonly caused by S. aureus Sub acute ◦ ◦ ◦ ◦ Mild toxicity Presentation over weeks to months Rarely leads to metastatic infection Most commonly S. viridans or enterococcus 55-75% of patients with native valve endocarditis (NVE) have underlying valve abnormalities MVP Rheumatic Congenital I.v. drug abuse ◦ 7-25% of cases involve prosthetic valves ◦ 25-45% of cases predisposing condition can not be identified Pathology : ◦ NVE infection is largely confined to leaflets ◦ PVE infection commonly extends beyond valve ring into annulus/peri annular tissue Ring abscesses Septal abscesses Fistulae Prosthetic dehiscence ◦ Invasive infection more common in aortic position and if onset is early Pathogenesis : Endothelial damage Platelet-fibrin thrombi Microorganism adherence Nonbacterial Thrombotic Endocarditis Endothelial injury Hypercoagulable state ◦ Lesions seen at coaptation points of valves Atrial surface mitral/tricuspid Ventricular surface aortic/pulmonic Modes of endothelial injury High velocity jet Flow from high pressure to low pressure chamber Flow across narrow orifice of high velocity ◦ Bacteria deposited on edges of low pressure or site of jet impaction Pathophysiology: Clinical manifestations ◦ Direct Constitutional symptoms of infection (cytokine) ◦ Indirect Local destructive effects of infection Embolization – septic or bland Hematogenous seeding of infection may present as local infection or persistent fever, metastatic abscesses may be small Immune response Immune complex or complement-mediated Local destructive effects Valvular distortion/destruction Chordal rupture Perforation/fistula formation Paravalvular abscess Conduction abnormalities Purulent pericarditis Functional valve obstruction Embolization Clinically evident 11 – 43% of patients Pathologically present 45 – 65% High risk for embolization Large > 10 mm vegetation Hypermobile vegetation Mitral vegetations (esp. anterior leaflet) Pulmonary (septic) – 65 – 75% of i.v. drug abusers with tricuspid IE Clinical Features : • Fever, chills, weakness, lethargy, weight loss, flu-like illness (not always present) • Longstanding IE (rarely seen now with earlier diagnosis): splinter haemorrhages, Janeway lesions, Osler nodes, Roth spots • Murmurs are present in 80 - 85% of patients with left sided IE Feature Frequency, % Fever 80–90 Chills and sweats 40–75 Anorexia, weight loss, malaise 25–50 Myalgias, arthralgias 15–30 Back pain 7–15 Heart murmur 80–85 New/worsened regurgitant murmur 10–40 Arterial emboli 20–50 Splenomegaly 15–50 Clubbing 10–20 Neurologic manifestations 20–40 Peripheral manifestations (Osler's nodes, subungual hemorrhages, Janeway lesions, Roth's spots) 2–15 Petechiae 10–40 Laboratory manifestations Anemia 70–90 Leukocytosis 20–30 Microscopic hematuria 30–50 Elevated erythrocyte sedimentation rate >90 Elevated C-reactive protein level >90 Rheumatoid factor 50 Circulating immune complexes 65–100 Decreased serum complement 5–40 Splinter Haemorrhages Janeway Lesions Osler Nodes Roth Spots • In IVDU right sided IE usually affect the tricuspid valve & occasionally the pulmonary valve, instead of systemic issues pulmonary embolism is the most important complication which can evolve into: • Pulmonary infarction • Pulmonary abscess • Bilateral pneumothoraces • Pleural effusion • Empyema • • The severity of valvular destruction depends on virulence of infecting organism & infection duration Heart failure can be the initial presentation Diagnosis : Modified Duke criteria It is based on clinical, microbiological & echo findings providing high sensitivity & specificity (~80%) for diagnosis of IE when applied to patients with native valve IE with +ve BC Modified Duke Criteria Major Criteria: Positive blood cultures Typical microorganism for IE from 2 separate blood culures Viridans sreptococci Sreptococcus bovis HACEK group Saph . Auresus Community acquired enerococci , in the absence of primary focus Persistently positive blood culture , defined as recovery of a microorganism consistent with IE from: Blood culture drawn more than 12 h apart OR All of 3or majority of 4 or more separate blood cultures , with first last drawn at least one h apart Single positive blood culture for Coxiella burnetii or antiphase I IgG AB titer more than 1: 800 Evidence of endocardial involvement Positive echocardiogram for IE TEE recommended in patients with PV ,rated at least possible IE by clinical crieria ,or complicated IE ( paravalvular abscess ) TTE as first test in other patients Definition of positive ECHO - Oscillating intracardiac mass, on valve or supporting structures , or in the path or regurgitant jets , or on implanted material , in he absence of an alternative anatomic explanation - Intracardiac abscess - New partial dehiscence of prosthetic valve New valvular regurgitation Increase in or change in preexisting murmur not sufficent Minor Criteria Predisposition such as a heart condition or IV drug use Fever Vascular phenomena - major arterial emboli, septic pulmonary infarcts, mycotic aneurysm, intracranial haemorrhage, conjunctival haemorrhage, & Janeway lesions immunological phenomena – glomerulonephritis , Osler s nodes , Roth spots , rheumatoid factor Other microbial evidence - serological tests, or a positive blood culture but does not meet a major criteria ( excluding single positive cultures for coagulase negative staph and organisms that do not cause endocarditis ) Definite IE 2 major criteria OR 1 major + 3 minor OR 5 minor criteria Possible IE 1 major + 1 minor OR 3 minor Rejected : Firm alternate diagnosis for manifestation of endocarditis OR Resolution of manifestation of endocarditis , with antibiotic therapy for 4 days or less OR No pathologic evidence of IE at surgery or autopsy after antibiotic therapy for 4 days or less Does not meet criteria for possible IE , as above TREATMENT : Goals of Therapy Eradicate infection Definitively treat sequelae of destructive intra-cardiac and extra-cardiac lesions Antibiotics : • Benzylpenicillin is the first choice for Streptococcus or Enterococcus penicillinsusceptible strains • Empirical treatment; flucloxacillin & gentamicin are the usual first line • Vancomycin is used in pts with intracardiac prosthetic material or suspected MRSA • For vanc-resistant MRSA: teicoplanin, lipopeptide daptomycin or oxazilidones (linezolid) is recommended • IV Abx is normally continued for 4-6 weeks, with the aim of sterilising the vegetations Indications for Cardiac Surgical Intervention in Patients with Endocarditis Surgery required for optimal outcome Moderate to severe congestive heart failure due to valve dysfunction Partially dehisced unstable prosthetic valve Persistent bacteremia despite optimal antimicrobial therapy Lack of effective microbicidal therapy (e.g., fungal or Brucella endocarditis) S. aureus prosthetic valve endocarditis with an intracardiac complication Relapse of prosthetic valve endocarditis after optimal antimicrobial therapy Surgery to be strongly considered for improved outcomea Perivalvular extension of infection Poorly responsive S. aureus endocarditis involving the aortic or mitral valve Large (>10-mm diameter) hypermobile vegetations with increased risk of embolism Persistent unexplained fever (10 days) in culture-negative native valve endocarditis Poorly responsive or relapsed endocarditis due to highly antibiotic-resistant enterococci or gram-negative bacilli Complications 1. Congestive heart failure • • • 2. Uncontrolled infection • • 3. Most common complication Main indication to surgical treatment ~60% of IE patients Persisting infection Perivalvular extension in infective endocarditis Systemic embolism • • • Brain, spleen and lungs 30% of IE patients May be the first symptom 5. 6. 7. 8. Neurologic events Acute renal failure Rheumatic problems Myocarditis High-Risk Cardiac Lesions for Which Endocarditis Prophylaxis Is Advised before Dental Procedures Prosthetic heart valves Prior endocarditis Unrepaired cyanotic congenital heart disease, including palliative shunts Completely repaired congenital heart defects during the 6 months after repair Incompletely repaired congenital heart disease with residual defects adjacent to prosthetic material Valvulopathy developing after cardiac transplantation Antibiotic Regimens for Prophylaxis of Endocarditis in Adults with High-Risk Cardiac Lesionsa,b A. Standard oral regimen 1. Amoxicillin 2.0 g PO 1 h before procedure B. Inability to take oral medication 1. Ampicillin 2.0 g IV or IM within 1 h before procedure C. Penicillin allergy 1. Clarithromycin or azithromycin 500 mg PO 1 h before procedure 2. Cephalexinc 2.0 g PO 1 h before procedure 3. Clindamycin 600 mg PO 1 h before procedure D. Penicillin allergy, inability to take oral medication 1. Cefazolinc or ceftriaxonec 1.0 g IV or IM 30 min before procedure 2. Clindamycin 600 mg IV or IM 1 h before procedure THANK YOU