EPIDEMIOLOGY OF DIABETES MELLITUS
advertisement
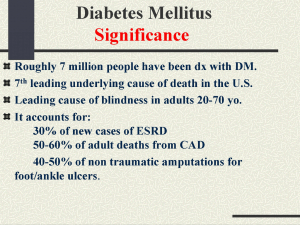
EPIDEMIOLOGY OF DIABETES MELLITUS Dr Salam Jassim Definition: It is a heterogeneous group of disorders characterized by hyperglycemia, and disturbances of carbohydrate, fat and protein metabolism with absolute or relative deficiency of insulin action and or secretion General Epidemiological Characteristics: It affects large number of people of about 100 million The number can increase to 230 million by 2010 It affects all ethnic and socioeconomic groups Incidence and prevalence are highly varied between and within countries 20-60 folds difference Considerable impact on economic and social condition, In1992 DM cost USA 90 billion $ General Epidemiological Characteristics: DM is an important cause of premature death and causes serious health consequences It is important RF of CHD CHD is the leading cause of death among diabetics In developing countries, the incidence and prevalence of Type 2 DM are rapidly increasing mostly due to modernization of life style In developing countries, mortality from acute complications is high due to lack of basic CLINICAL STAGING OF DM I. DM Regardless of underlying cause is subdivided into: Insulin requiring for survival Insulin requiring for control Not Insulin requiring II. Impaired glucose regulation It is a metabolic state intermediate between normal glucose homeostasis and DM IFG: Impaired fasting glycemia (fasting) FPG: > 110 mg/dl- <126 mg/dl (>6.1- <7 mmol/L) Whole blood : >100 mg/dl-<110mg/dl (>5.6< 6.1 mmol/L) IGT: Impaired glucose tolerance (postprandial) II. Impaired glucose regulation All those with IFG should have OGTT Individuals with IFG or IGT may be euglycemic in their daily life as seen through HbA1C IGT and IFG are not clinical entities, rather risk categories for future DM and or CVD They are often associated with Metabolic Syndrome III. Normoglycemia FPG < 110/dl CLINICAL STAGING OF DM Clinical staging regardless of its etiology, progress through several clinical staging during its natural history Individual subject may move from one stage to another in either direction Clinical staging reflect the hyperglycemia which reflect the extent of the disease process Diagnosis: Diagnosis is clear when symptoms are severe with gross hyperglycemia Sever hyperglycemia under stress is not sufficient Diagnosis: Asymptomatic subject: A single abnormal test is not sufficient At least one additional result within diabetic range , if it fails , then surveillance with periodic retesting taking in consideration ethnicity , family history , age , adiposity, and concomitant risk factors Glycated Hb had similar sensitivity and specificity for glucose test OGTT is indicated if casual blood test is uncertain Diagnostic range Fasting Plasma Glucose: 126 mg/dl (7.0 mmol/L) Whole blood: 110mg/dl (6.1mmol/L) In epidemiologic studies FPG is sufficient or 2hr after 75 gm oral glucose load AETIOLOGICAL CLASSIFICATION I - Type 1 B-cell destruction usually leading to absolute insulin deficiency (low or undetected c-peptide level) Insulin is usually required for survival Risk of ketoacidosis Type 1 a) Autoimmune DM Results from autoimmune destruction of B-cell Destruction could be rapid especially in children or slow especially in adults (Latent Autoimmune Diabetes in Adults LADA) Markers of Immune destruction Islet cell auto Abs Insulin Auto Abs Auto Abs to glutamic acid decarboxylase (GAD) Type 1 a) Autoimmune DM – Some individuals may be metabolically normal before the disease become evident, but the progress of B cell destruction can be detected – Immunological markers are present in 85-90% of those patients – Peak incidence in childhood and adolescence – Environmental factors play a role – Genetic predisposition – Patients are usually not obese – Other autoimmune diseases may be present Type-1 b) Idiopathic No known etiology Seen more in Africans and Asians II – Type 2 They have relative rather than absolute insulin deficiency with resistance to insulin action They do not require insulin for survival They may remain undetected for long time They have increased risk of macro and micro vascular complications The autoimmune destruction does not occur Ketoacidosis is infrequent Obesity is very common Insulin level could be normal or elevated II – Type 2 Insulin sensitivity can be increased by decreasing weight, increasing physical activity and or pharmacologic treatment The risk of this type increases with age, obesity, lack of physical activity It is more in women with GDM and individuals with HT or Dyslipidemia Genetic predisposition is common Prevalence showed racial / ethnic variation III – Other specific types Genetic defects of B cell function Genetic defects of insulin action Diseases of exocrine pancreas Endocrinopathies Drugs or chemical induced DM infections Uncommon but specific forms of immune mediated DM Other genetic syndromes sometimes associated with DM GESTATIONAL HYPERGLYCEMIA AND DIABETES It is carbohydrate intolerance resulting in various severity of hyperglycemia with onset or first recognized during pregnancy GESTATIONAL HYPERGLYCEMIA AND DIABETES Elevated fasting or postprandial plasma glucose level in the early pregnancy (first trimester, and first half of second trimester) indicates that DM antedate pregnancy Normal OGTT in early pregnancy does not exclude the possibility that GDM is not going to develop High Risk Groups Older women Women with previous history of large for gestational age baby Women from certain ethnic group Any women with elevated fasting or casual blood glucose High Risk Groups It is better to screen such groups during the first trimester to detect previous undiagnosed DM Formal systematic testing for gestational DM is usually done between 24 and 28 weeks After the pregnancy ends, the woman should be re-classified as having: DM, IGT, or Normal Glucose Tolerance based on OGTT done 6 weeks or more after delivery Women with GDM are at increased risk for subsequent DM THE METABOLIC SYNDROME Working definition: Glucose intolerance, IGT or DM and /or insulin resistance together with 2 or more of the following: Raised arterial BP (>140/90) Raised Pl.TG =/> 150 mg/dl and/or low HDL-C (<35mg/dl in males; < 39 mg/dl in females) Central obesity waist: hip ratio: Males: >0.9, Females: >0.85 And /or BMI >30 Microalbuminurea (>/= 20 ug/min or Albumin/creatinin ratio >/= 30 mg/gm) Other components: hyperuricemia, coagulation disorders, raised PAI-1 THE METABOLIC SYNDROME There is heterogeneity in the strength of insulin resistance Metabolic syndrome increases risk of Macro vascular disorders Management should include control strategies of all the components and not only hyperglycemia Metabolic syndrome may be present for up to 10 years before detection of the PRIMARY PREVENTION OF TYPE 1 DM It should be done before onset of type 1 pathological process.i.e: before development of immunological markers It is still EXPERIMENTAL Because of the very low prevalence, it required screening test of high specificity and sensitivity, inexpensive and easy to perform Screening include: Family history Genetic markers (HLA) Immunological risk markers (ICA, IAA, Anti GAD) Metabolic risk factors Screening Screening is costly and technically difficult Those have these factors have 10 folds excess risk Still 95-97% of them do not develop the disease later Primary Prevention Strategy Deprivation of caw milk protein in the neonatal and early infancy Administration of free radical scavenger, as nicotinamide Allowing B-cell rest by administration of early insulin treatment Encouraging the development of Antigen tolerance by administration of early insulin treatment or oral antigens Immunosuppression or Immunomodulation PRIMARY PREVENTION OF TYPE 2 DM No population based studies on primary prevention of type 2 DM Prevention should be based on efforts to decrease insulin resistance and promotion of insulin secretion Life –style measures that decrease insulin resistance: Correction and prevention of obesity Avoidance of high fat diet Encouraging using unrefined sugar and soluble fibers Avoidance or cautious use of diabetogenic drugs Encourage physical activity SECONDARY PREVENTION OF TYPE 2 DM Aims at retarding progression of DM, decrease risk or severity of complications and so decrease premature morbidity and mortality 1. Screening for undetected DM 2. Control of hyperglycemia, and other metabolic abnormalities 3. Correction of other CV RFs (smoking, dyslipidemias, obesity) Screening approaches: Population approach Selective screening: on high risk individuals Opportunistic screening: most appropriate and highly cost effective TERTIARY PREVENTIONOF TYPE 2 DM Aims at decreasing morbidity and mortality by delaying or arresting the complications Good glycemic control (by intensive treatment, frequent monitoring of blood glucose level) slow or arrest development of early microvascular complications COMPLICATIONS OF DM ACUTE COMPLICATIONS 1. Hypoglycemia Affect the brain and the heart The risk is more among: 1. Hypoglycemia unawareness and counter regulatory unresponsiveness as in autonomic neuropathy, B-blockers and alcoholism 2. Infants 3. Patients with IHD or TIA Prevention: health education Cautious exercise Glucagons for emergency Caution and health education when changing treatment 2. Diabetic ketoacidosis 10-15% mortality, 50% of them are avoidable 1. 2. 3. Precipitating factors Infection Acute illnesses Insufficient insulin treatment 1. 2. Prevention: Health education Early control of precipitating factors 3. Infections Poorly controlled diabetics are at increased risk of: 1. TB , lung and other organs 2. fungal infection of skin and mucus membrane 3. anaerobic infection of deep tissues 4. UTI ( increasing diabetic nephropathy) CHRONIC COMPLICATIONS I. Macrovascular Complications Atherosclerosis: CAD, CVA, PVD The most common complication among diabetics, account for 75% of their deaths DM increases CAD and CVA by 2-3 folds and PVD by 4 folds Diabetic women lose their relative protection against CAD before Atherosclerosis: Role of hyperglycemia as CRF mediated through: 1. Glycation of LDL particles 2. Glycation of arterial wall protein 3. Stimulate insulin secretion Atherosclerosis: Hyperinsulinemia is independently associated with atherosclerosis through its effect on BP, TG, PAI-1 level or arterial wall metabolism Obesity (especially central) increases liability to atherosclerosis and DM through: Increased insulin resistance, hyperinsulinemia, Dyslipidemia, and HT Among diabetics the process of atherosclerosis is accelerated with Atherosclerosis: Screening for RFs of macrovascular complications: Lipid profile, BP, Ht, waist/hip ratio, smoking history, family history, urinary albumin excretion Presence of macro vascular complications is ascertained through: 1. Clinical history: history of MI, TIA, and intermittent claudication 2. Physical examination: bruit, peripheral pulses, evidence of ischemia on ECG The sensitivity and specificity of these measures are moderate CHRONIC COMPLICATIONS II. Microvascular complications 1. Diabetic Retinopathy It is asymptomatic gradual process, so screening is vital at least every 2 years Drugs and glycemic control can not prevent it It is responsible for 86% of blindness among Type 1diabetics, and 35% of Type 2 diabetics. 100% of Type 1 diabetics developed Diabetic retinopathy, 75% of proliferate type 60% of Type 2 diabetics developed diabetic retinopathy, 10% pf proliferative Type Diabetic Retinopathy Timely laser photocoagulation can prevent 90% of sever visual loss Treatment of HT and avoidance of smoking are important in its control 2. Diabetic Neuropathy It is the commonest complication of DM The prevalence is increased with: 1. 2. 3. 4. Increased duration of DM Increased glycated Hb level Smoking History of CVD Types of Neuropathy A. Peripheral Neuropathy Polyneuropathy: Distal sensorimotor neuropathy, Proximal motor neuropathy Focal neuropathy: mononeuropathy, entrapment neuropathy Multifocal neuropathy B. Autonomic Neuropathy Types of Neuropathy The most common is the distal sensorimotor neuropathy which is classified into: 1. Early: asymptomatic, detectable sensory loss, positive neurological tests 2. Symptomatic: sensory loss, frank numbness, parasthesia+/- pain 3. Severe: motor involvement, disabling symptoms, potential for ulceration, infection, necrosis, and gangrene Screening Tests Inspection: feet: dry skin, hair or nail abnormality, callus or infection Vibration sensation on the dorsum of big toe: normal, reduced, absent Ankel Reflex: normal, reduced, absent Types of Neuropathy Cardiovascular autonomic neuropathy Serious and can precipitate death. They have difficulty in detecting hypoglycemia and / or spontaneous recovery from hypoglycemia Prevention: Education of patients and PHC physicians Good glycemic control Aldose reductase inhibitor 3. Diabetic Nephropathy A major cause of premature morbidity and mortality in diabetics DM increases risk of Renal Failure by about 17-20 folds 25% of ESRD are due to DM Diabetic Nephropathy Diabetic Nephropathy can be divided into: 1. Incipient (sub clinical) nephropathy Microalbuminuria: 30-300mg/24 hours HT may be present 2. Clinical nephropathy Persistent proteinuria >300 mg/ 24 hours Usually accompanied with HT Diabetic Nephropathy 3. Advanced nephropathy Significant reduction of GFR, Symptoms of uremia +/- nephritic syndrome 4. ESRD Prevention Tight glycemic control Yearly urinary microalbumin test Dietary protein restriction Vigorous control of BP Prevention Other supportive measures: – Correction of lipid abnormalities, metabolic bone diseases, and anemia – Avoidance of fluid retention – Vigorous treatment of UTI – Avoidance of nephrotoxic drugs 4. DIABETIC FOOT It is infection, ulceration, destruction, of deep tissues with neurological and peripheral vascular diseases Diabetics have 15 folds risk of amputation than non diabetics DIABETIC FOOT Incidence of amputation is associated with: 1. Duration of DM Glycemic control HT Smoking 2. 3. 4. DIABETIC FOOT Lower limb amputation is more in developing countries: 1. Lack of proper foot wear 2. Inadequate hygiene 3. Poorly controlled DM Screening 1. 2. 3. Abnormal vibration test Presence of foot deformity Past history of lower extremity ulceration or amputation Screening should be done by a trained physician Prevention Regular attendance to health care settings Formal teaching sessions Provision of appropriate written and or audiovisual materials The patient should be advised – Not to walk bare-footed – Daily looking to foreign bodies in the shoes – Avoid bathroom surgery – Treat fungal disease and minor cuts – Usage of mirror to examine plantar side of the foot – Test the degree to which pain sensation is lost – Prevent burns AMPUTATION IS A PREVENTABLE COMPLICATION EDUCATION OF DIABETIC PATIENTS It is the corner stone of DM management It covers: self care changing behavior to prevent and control of complications encourage interaction with health care providers Contents of Educational Program Nature of disease, types, clinical presentation, diagnosis, complications, types of treatment, side effects, exercise, self monitoring , avoidance and recognition of hypoglycemia, and hyperglycemia, foot care , pregnancy and OC, avoidance of smoking, CV RFs, need for follow up, self management skills and attitudes Active participation of the family is vital in DM management Types of education methods 1. 2. 3. Individual counseling Group teaching Educational materials: posters, pamphlets, books… Special educational programs are needed for special groups as children and pregnant women Education of Health Professionals Basic understanding of DM and its managements Training in educational methods Training of dietetics and nurses Education of the community Prevention or modification of dietary habits and other life-style characteristics that link with DM