EMS Diabetic
advertisement

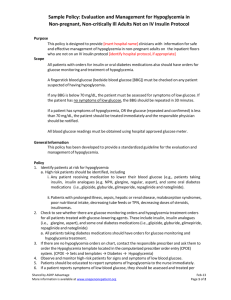
Diabetic Emergencies Not too Sweet – Not too Sour What is Diabetes? Diabetes Mellitus – a disorder of Insulin Diabetes Mellitus Type I – insulin dependent Usually starts at an early age Caused by autoimmune destruction of Beta cells No insulin production at all No Insulin = Death 1922 – first successful use of insulin to treat kids with DKA – always fatal up until that point. Currently – insulin pumps and various types of insulin are state of the art in treatment for Type I DM. Diabetes Mellitus Type II – insulin resistant Obesity, sedentary lifestyle Beta blockers, glucocorticoids, thiazides 90% of all diabetes in US Insulin is unable to do its work Dietary changes, medications or insulin may be needed Usually does not cause DKA Diabetes Mellitus Gestational Diabetes Occurs during pregnancy Resolves with delivery most of the time. Due to hormone levels and obesity Diabetes Insulin What is Insulin? A hormone made by Beta cells in the Pancreas Insulin works on multiple cells to regulate blood Glucose levels Muscle – prevents protein breakdown Adipose tissue – increases fat production Liver – increased glycogen synthesis Increased glucose and amino acid uptake Inhibits Glucagon production Effects Vasculopathy - Vascular damage Effects Nephropathy - Kidney Damage Effects Neuropathy – nerve damage Effects Retinopathy – eye damage Effects Diabetic Ketoacidosis Effects Hypoglycemia – caused by treatment Medications used in Treating Diabetes Antihyperglycemics – stimulate insulin production Sulfunylureas – Diabinese, Glucotrol, Diabeta, Amaryl Meglitinides – Prandin, Starlix Antihyperglycemics – do not stimulate insulin Biguanide – Metformin – Lactic acidosis Thiazolidinediones – Avandia, Actos Alpha-glucosidase inhibitor – Precose, Glyset DPP-4 Inhibit – Januvia, Onglyza Hypoglycemia The brain MUST have glucose to function Brain is not affected by insulin. Normal blood sugar levels range from 70-100 Low blood sugar can be caused by Taking insulin when you cannot eat or forget to eat Intentionally overdosing on insulin Taking the wrong type Exercising more than normal and not adjusting diet Certain diabetes medications, but not all Infections/illness which prevent eating Hypoglycemia Clinical symptoms Lethargy Unconsciousness Stroke-like symptoms (especially in those with prior strokes) Seizures Trouble speaking Confusion Cardiac Arrest Hypoglycemia Testing Fingerstick blood sugar Make sure machine gets calibrated regularly Make sure you have the right test strips that are not expired Clean finger off with alcohol Prick side of finger with lancet Squeeze finger (milk it) to get enough to cover testing area Read machine when test is complete DEMO TIME… Hypoglycemia Treatment – Glucose! IV Dextrose – AEMTs/Paramedics Adults – 50% 1 ampule (50ml = 25gm) Children – 25% 2ml/kg Neonates – 12.5% - 1ml/kg Oral Glucose – EMR/EMTs Must have gag reflex and be alert to avoid aspiration/choking Glucagon – for adults 1-2 mg IM if cannot get an IV Dextrose Class – carbohydrate Mechanism – provides metabolic substrate Contraindications Absolute – None Relative – hyperglycemia Dosage – 50ml of D50, repeat x1 if needed Peds – 2ml/kg of D25 Neonates – 1ml/kg of D12.5 Glucagon Class – hormone Mechanism – stimulates glycogen breakdown in the liver and muscle, increasing glucose levels Contraindications Absolute - sensitivity Relavtive – starvation, fasting, adrenal insufficiency Uses – hypoglycemia, beta-blocker overdose, calcium channel overdose, anaphylaxis (for folks on beta-blockers) Dosage – hypoglycemia – 1mg IV/IM Q20 min; beta-antagonist OD – 3-5mg IV; anaphylaxis 1-2mg IV Kids - <20kg – 0.5mg IV/IM; >20mg – 1mg IV/IM Side effects – Nausea, vomiting, diaphoresis, hypotension, rash Meter is broken… Get as much history as possible. Smell for ketones (only half of us can) Are there empty insulin bottles on scene? Recent exercise or illness? Err on the side of treating for hypoglycemia DKA No insulin activity = high blood sugar levels Can’t make glycogen, fatty acids and cannot move glucose into cells Cells starve Fatty Acid breakdown Ketosis High blood sugar sugar in urine peeing a lot dehydration acidosis Diabetic Ketoacidosis! Fruity odor to breath Increased respiratory rate Abdominal pain Nausea/Vomiting Tachycardia / hypotension Hyperglycemia Low Insulin activity = high blood sugars Still able to get some glucose in cells = no starvation = no ketosis Acidosis also less likely No fruity odor Generalized weakness Less nausea/vomiting Death very rare Hyperglycemia Treatment ABC’s IV fluids! Adults – 500ml – 1 liter WO Children – 20ml/kg fluid boluses May repeat if needed for hypotension or tachycardia What about Insulin Pumps If hypoglycemia – have patient turn off pump after you wake them up with D50 If hyperglycemia – don’t touch it May not be working Patient may be able to do a bolus on their own based on their sliding scale If infected, leave in place, but do not use. Alcoholic Ketoacidosis Chronic Alcoholics are malnourished Few glycogen stores After a binge, their glucose levels can drop, stimulating fatty acid breakdown Treatment is glucose with Thiamine Don’t withhold glucose if level is abnormal! You wanna refuse? While people have a right to make their own decisions, it must be an INFORMED decision They must: Be alert, oriented to person, place, time, and situation Know of the risk for relapse Have recovered within 10 minutes. FSBS >80 They should Have test strips available or have someone there to call back if they get hypoglycemic again. Have adequate follow-up. Questions A diabetic’s family calls 911 for sudden onset of left sided weakness that started 10 minutes prior to arrival. After ABCs, what is your next step? Questions A Diabetic teen-ager decides to say “f&^% you” to his diet, and eats an ice cream sundae. A day later, he calls 911 for vomiting and abdominal pain. His Glucose on fingerstick reads “Hi” What should you give? Questions You come across a “local regular” beside the bar. He smells of alcohol, and is lethargic. He looks like he hasn’t been eating regularly for quite some time. You consider _____ as a possible diagnosis, and _________