Pulmonary Hypertension: What you need to know
advertisement
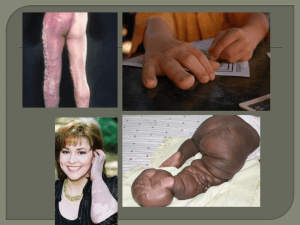
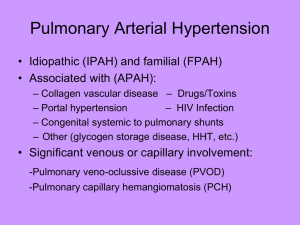
Pulmonary Hypertension: What you need to know William Leeds, DO, FCCP Pulmonary & Sleep Associates Veritas Clinical Specialties Topeka, KS What is Pulmonary Hypertension? • Definition – Right heart catheterization showing • Sustained elevation of mean pulmonary artery pressure > 25 mmHg at rest • Secondary RHC parameters – MPCWP < 15 mmHg – PVR > 3 Woods Units WHO Classifications • Group I: Pulmonary Arterial Hypertension (estimated 15 cases per 1 million adults) – – – – Idiopathic (primary) Familial Drug- and toxin-induced Associated with connective tissue disease, HIV, portal hypertension – Associated with significant venous or capillary involvement – Persistent pulmonary hypertension of the newborn WHO Classifications, cont. • Group II: Pulmonary Hypertension Owing to Left Heart Disease • Group III: Pulmonary Hypertension Owing to Lung Diseases or Hypoxemia • Group IV: Chronic Thromboembolic Pulmonary Hypertension • Group V: Pulmonary Hypertension with Unclear Multifactorial Mechanisms WHO Functional Classes of PAH Class Description I Patients with PH but without resulting limitation of physical activity. Ordinary physical activity does not cause undue dyspnea, chest pain, or near syncope. II Patients with PH resulting in slight limitation of physical activity. They are comfortable at rest. Ordinary physical activity causes undue dyspnea or fatigue, chest pain, or near syncope. III Patients with PH resulting in marked limitation of physical activity. They are comfortable at rest. Less than ordinary activity causes undue dyspnea or fatigue, chest pain, or near syncope. IV Patients with PH with inability to carry out any physical activity without symptoms. These patients manifest signs of right-heart failure. Dyspnea and/or fatigue may even be present at rest. Discomfort is increased by any physical activity. Pathogenesis of PAH: Proliferative Vasculopathy Triggers (Initiation Factors) • Inflammation • Autoimmunity • Infection • Hemodynamic shear stress • Hypoxia • Drugs/chemicals/toxins Genetic Predisposition • BMPR-2 and ALK-1 genes • Kv channels • Oxygen-sensing mechanisms • 5-HHT Activation Pathogenic Vascular Mediators • Endothelial dysfunction – Vasoactive mediators – Growth factors Vascular Wall Remodeling • Proliferation • Vasoconstriction • In-situ thrombosis Adapted from Gaine S. JAMA. 2000;284:3160-3168. Slide courtesy of Roxanna Sulica, MD. Diagnosis of PAH • Often made late in the disease – Median duration between symptom onset and diagnosis is 27 months • Late diagnosis due to – Under-recognition – Nonspecific symptoms – Confusion with other conditions – iPAH is diagnosis of exclusion Signs and symptoms of PAH • No early symptoms • Progressive DOE, fatigue, palpitations, chest pains, cough, hoarseness, syncope • Symptoms of RHF – Ascites – Edema • Must screen highrisk populations – Family history of iPAH – Connective tissue disease – Pulmonary embolism – Congenital heart disease Prognosis of iPAh is poor with supportive care only Median survival 2.8 years Percentage surviving 100 80 60 40 20 0 0 0.5 1 1.5 2 2.5 3 Years of follow up 3.5 4 4.5 5 PAH/ssc progresses even more rapidly Percent survival 100 80 No lung involvement 60 Lung involvement without PAH 40 20 PAH 0 0 1 2 3 4 5 6 7 8 9 10 11 12 13 Years from diagnosis of pulmonary hypertension Diagnostic workup (CC: SOB) • CXR • Complete PFT • Initial labs (CBC, CMP, BNP) • Physical exam • Med hx/symptom review • Echocardiogram • If echo shows PAH – VQ scan/CT angio – Labs (ANA, RF, HIV, ANCA, anti-Scl 70, ESR, CRP) – Polysomnogram – 6MWT – RHC Right heart catheterization • • • • • • • PA pressure PCW pressure Cardiac output PA saturation Pulmonary vascular resistance Vasodilator challenge Exercise challenge Treatment options • Treat the underlying/contributing condition • Oxygen if needed – Check 6MWT and nocturnal oximetry • • • • Oral medications Inhaled medications IV medications Surgical interventions Targets for PAH therapy Oral medication options for PAH • Warfarin (iPAH) • Calcium channel blockers (amlodipine) – Blocks entry of calcium into heart and muscle cells – Improves ability of heart to pump blood – Relaxes smooth muscle in walls of heart and smooth muscles – Only a small number of PAH patients respond – Side effects: nausea, h/a, rash, edema, dizziness, fatigue Oral medication options, cont. • PDE-5 inhibitors – Blocks the action of phosphodiesterase – Dilates pulmonary vasculature – Side effects: vision problems, h/a • Endothelin receptor antagonists – Blocks vasoconstrictive effects of endothelin-1 – Dilates pulmonary vasculature – Side effects: liver toxicity and anemia (requires routine monitoring), edema Inhaled medication options • Inhaled iloprost (Ventavis) – Dilates systemic and pulmonary vessels – Inhaled multiple times daily – Side effects: cough, h/a, throat pain • Inhaled treprostinil (Tyvaso) – Dilates systemic and pulmonary vessels – Inhibits platelet aggregation – Inhaled multiple times daily – Side effects: cough, throat irritation, h/a IV medication options • IV epoprostenol (Flolan) – Directly dilates peripheral vessels – Inhibits platelet aggregation – Must be initiated in hospital – Cannot be stopped abruptly – Side effects: h/a, nausea, jaw pain, flushing, hypotension Surgical options • Atrial septostomy • Heart-lung transplant Treatment options summarized Case Studies • GL • BB • KS Case Study GL • Presented to pulmonary service in September 2006 at age 53 • Chief complaint was progressive SOB with exertion • PMH: scleroderma dx at age 39, unspecified arrhythmia, GERD, depression, allergies, arthritis, and migraine h/a • PSH: tonsillectomy GL, continued • Current medications: inderal, nexium, miacalcin, percocet, tramadol, mucinex, alavert, vitamin C • Allergies: imitrex (unknown reaction) • FH: COPD in father, lung ca and COPD in brothers • SH: 30 pk-yrs of cigarette use; quit in 2000 GL Diagnostics • CXR 8/20/03: “mild decrease of lung volumes and mild increased prominence of interstitial markings in both lung bases since 1992 Some degree of interstitial lung disease cannot be ruled out” • PFT 9/19/06: FVC 2.19 L (70%), FEV1 1.79 L (70%), FEV1/FVC 82, IC 1.67 L (77%), RV 1.15 L (64%), TLC 3.44 L (70%), Diffusion 36%, DL/VA 2.53 L (55%) GL Diagnostics, cont. • Echocardiogram 8/21/06: EF 60-65%, abnormal LV diastolic filling/impaired relaxation, mild AR, mild MR, mild TR, mild PR, RVSP 68 mmHg • RHC 11/01/06: mean RA 10, mean RV 7, PAP 70/29 (mean 44), MPCWP 13, CO ~4L; adenosine trial showed decreased MPAP 38 • 6MWT: 390 m, O2 sat nadir 92% on room air GL Treatment Course • November 2006: bosentan, sildenafil, and warfarin initiated • August 2007 CT: mild bibasilar interstitial fibrosis • October 2007: oxygen added – 6MWT 183 m; O2 sat nadir 83% on room air • November 2007: transtracheal oxygen initiated • February 2008: Ventavis added GL Treatment Course, cont. • August 2008: referred to KUMC – RHC: normal EF, RA 8, MPAP 47, MPCWP 1214, CO 5.4 – 6MWT 428 m; O2 sat nadir 92% on 3L – CT chest: progression of bibasilar fibrosis – IV prostacyclin held due to stability of RHC findings • October 2008: unable to proceed with lung transplant due to financial issues • May 2009: 6MWT 292 m; O2 sat nadir 86% on 4L GL Treatment Course, cont. • June 2009: – RHC: MPAP 66, MPCWP 22, CO 4.6 – Significant GERD symptoms • February 2010: transitioned from Ventavis to Tyvaso • July 2010: symptoms acutely worsened – Hospitalized for hemoptysis – Hospice discussed GL Treatment Course, cont. • November 2010: last contact – Echo: EF 65%, RV severely dilated with moderate systolic dysfunction, RA severely dilated, moderate TR, PAP 84 – PFT: FVC 1.83 (60%), FEV1 1.59 (65%), FEV1/FVC 87, TLC 62%, Diffusion 11% Deceased February 2011 GL Discussion • Questions/comments? Case Study BB • Presented to pulmonary service in July 2002 at age 45 • Chief complaint was progressive dyspnea on exertion for last 6 months • PMH: poss. CVA or seizure age 19 w/no further recurrence • PSH: none • FH: CAD in father, mother, brother (brother had heart surgery at age 46) • SH: no tobacco or illicit drug use Case Study BB, cont. • Current medications: Combivent inhaler and previous use of prednisone without significant improvement in symptoms • Allergies: NKDA BB Diagnostics • PFT 7/10/02: FVC 3.78 L (108%), FEV1 2.64 L (91%), TLC 6.18 l (114%), VC 3.78 L (108%), RV 2.4 L (128%), Diffusion 94% • ABG on room air 7/19/02: pH 7.395, pCO2 36.8, PO2 57.1, BE -2.0, HCO3 21.9, O2 sat 88% • LHC 7/19/02: RA 1, RV 0, MPAP 50, MPCWP 11, CO 4.21 L • O2 sat 88% with ambulation BB Treatment Course • July 2002: Placed on Oxygen, digoxin and bosentan • Referred to Mayo Clinic, Rochester MN – Diagnosed with Primary Pulmonary Htn • September 2002: initiated on warfarin • RHC 12/02: RA 7, MPAP 43, MPCWP 15, CO 4.73; Flolan trial showed MPAP 46, MPCWP 10, CO 7.43 – Amlodipine added BB Treatment Course, cont. • Echo 9/8/03: EF 63%, moderate RV enlargement, moderately decreased RVSF, RVSP 77 • Echo 11/04: RVSP 74, moderate RV enlargement, mild TR • Echo 02/06: severe RV enlargement, RVSP 81 • February 2006: Sildenafil added • Care turned over to Mayo Clinic physicians • Last contact May 2006 BB Discussion • Questions/comments? Case Study KS • Presented to pulmonary service August 2011 at age 46 • Chief complaint was increased dyspnea and LE edema x 2 months • PMH: DVT/PE 1996, HTN, DM, hypothyroid, obesity and allergies • PSH: none • FH: father died age 48 of AMI; HTN, DM • SH: works at a bank, denies cigarette and illicit drug use Case Study KS, cont. • Current medications: amlodipine, vit E, levothyroxine, MVI, losartan/hctz, ASA, furosemide, fish oil, metformin, Ca/Vit D, omeprazole, warfarin, potassium • Drug allergies: NKDA KS Diagnostics • Labs 7/12/11: BNP 430, Hgb 11.1, Hct 34.6, BMP WNL, HIV neg. • CT 7/22/11: no pulmonary emboli/no acute process • Cardiac stress test 7/27/11: LVEF 57%, dilated RV, normal EKG • Bilateral LE doppler 8/3/11: no DVT • VQ lung scan 8/3/11: high probability for PE in lateral segment of RLL KS Diagnostics, cont. • Echo 7/27/11: normal LVF, abnormal septal motion likely r/t right-sided volume overload, trace MR, RA and RV significantly enlarged, mod TR, RVSP 107 • PSG 8/4/11: AHI 106, REM AHI 109, baseline O2 sat 84%, O2 sat nadir 53% KS Treatment Course • August 2011: warfarin, nasal CPAP w/O2, and weight loss initiated; CV meds adjusted • October 2011: hospitalized for dizziness secondary to abnormal uterine bleeding (Hgb 6.2) – Consideration given to IVC filter • 098 Case Study CZ • First presented to pulmonary service February 2010 at age 66 • Chief complaint was dyspnea, cough and sputum production • PMH: a-fib, chronic bronchitis, HTN, hypothyroid • PSH: constrictive pericarditis surgery • FH: CAD in parents • SH: 20 pk-yrs of cigarette use, no illicit drug use Case Study CZ, cont. • Current medications: Toprol, warfarin, vit D, calcium, ASA, furosemide, levothyroxine, albuterol, Benicar, omeprazole, simvastatin • Allergies: cefdinir, penicillin, codeine, propoxyphene CZ Diagnostics • PFT 2/12/10: FVC 1.48 L (58%), FEV1 1.14 L (59%), FEV1/FVC 77, TLC 5.03 L (110%), VC 2.53 L (98%), RV 2.5 L, Diffusion 115% • Echo 9/8/10: LV hypertrophy, EF 75%, moderate RV enlargement with reduced RVSF, mod-severely dilated RA, mild TR, RVSP 45-50 • RHC 9/8/10: MPCWP 31, MPAP 43, CO 2.7, post-nitric oxide infusion CO 2.7