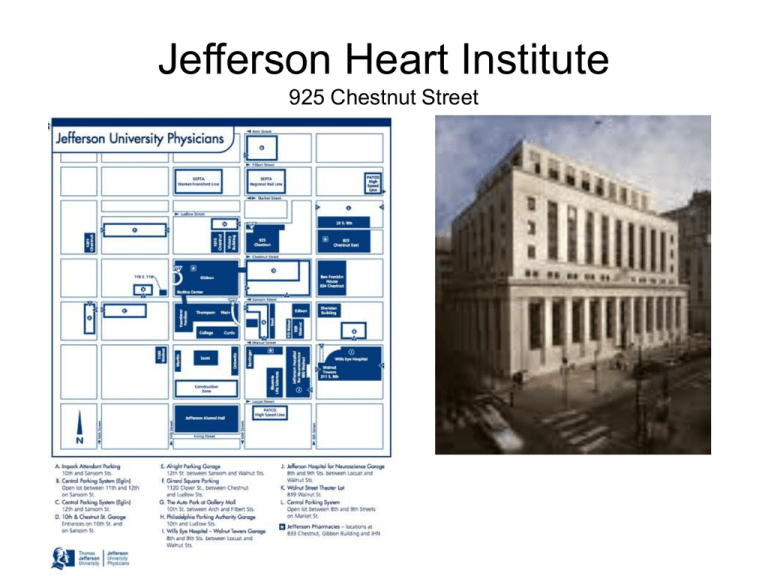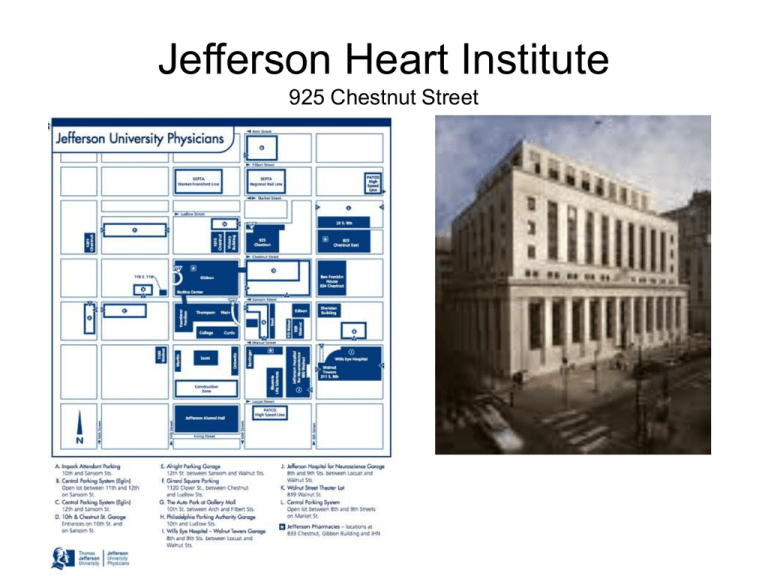
Jefferson Heart Institute
925 Chestnut Street
Referring Physician
Name of physician
Office Address
Pride
Communication
More referrals
“Carbon Copy”
Interested physicians
Office Address
Pride
Communication
More referrals
Reason for the visit
(a.k.a., chief complaint)
Reason for the visit
Pulmonary hypertension evaluation
Elevated pulmonary artery pressure by
echocardiogram
Elevated pulmonary artery pressure by right
heart catheterization
History of Present Illness
W.H.O. Functional Class
W.H.O. Group
Drugs trialed and response to therapy
Relevant family history
Relevant testing
Symptoms of PH
• Dyspnea
• Syncope
• Dizziness
Fatigue
Edema
Chest Pain
Non-specific nature of complaint can lead to:
• Confusion with other conditions
• Delayed diagnosis
Gaine et al. The Lancet, 1998. 352; 719
W.H.O. Functional Classification
Class I: Patients with PH but without resulting limitation of physical activity.
Ordinary physical activity does not cause undue dyspnea or fatigue, chest
pain or near syncope.
Class II: Patients with PH resulting in slight limitation of physical activity.
They are comfortable at rest. Ordinary physical activity causes undue
dyspnea or fatigue, chest pain or near syncope.
Class III: Patients with PH resulting in marked limitation of physical activity.
They are comfortable at rest. Less than ordinary physical activity causes
undue dyspnea or fatigue, chest pain or near syncope.
Class IV: Patients with PH with inability to carry out any physical activity
without symptoms. These patients manifest signs of right heart failure. They
are comfortable at rest. Dyspnea and/or fatigue may even be present at rest.
Discomfort is increased by any physical activity. (Syncope)
W.H.O. Classification - 2008
1. Pulmonary arterial hypertension (PAH)
1.1 Idiopathic
1.2 Heritable
1.2.1 BMPR2
1.2.2 ALK1, endoglin (with or without hereditary hemorrhagic telangiectasia)
1.2.3. Unknown
1.3 Drug- and toxin-induced
1.4 Associated with
1.4.1 Connective tissue diseases
1.4.2 HIV
1.4.3 Portal hypertension
1.4.4 Congenital Heart Diseases
1.4.5 Schistosomiasis
1.4.6 Chronic hemolytic anemia
1.4 Associated with significant venous or capillary involvement
1.5 Persistent pulmonary hypertension of the newborn
1’. Pulmonary veno-occlusive disease (PVOD) and/or pulmonary capillary
hemangiomatosis (PCH)
W.H.O. Classification - 2008
2. Pulmonary hypertension owing to left heart disease
2.1 Systolic dysfunction
2.2 Diastolic dysfunction
2.3 Valvular disease
3. Pulmonary hypertension owing to lung diseases and/or hypoxemia
3.1 Chronic obstructive pulmonary disease
3.2 Interstitial lung disease
3.3 Other pulmonary diseases with mixed restrictive and obstructive pattern
3.4 Sleep disordered breathing
3.5 Alveolar hypoventilation disorders
3.6 Chronic exposure to high altitude
3.7 Developmental abnormalities
4. Chronic thromboembolic pulmonary hypertension (CTEPH)
5. Pulmonary hypertension with unclear multifactorial mechanisms
5.1 Hematologic disorders: myeloproliferative disorders, splenectomy
5.2 Systemic disorders: sarcoidosis, Langerhans cell histiocytosis: lymphangioleiomymatosis,
neurofibromatosis, vasculitis
5.3 Metabolic disorders: glycogen storage disease, Gaucher disease, thyroid disorders
5.4 Others: tumoral obstruction, fibrosing mediastinitis, chronic renal failure on dialysis
Past Medical History
W.H.O. Group 1
Heritable
Collagen vascular disease
HIV
Portal hypertension
Anorexigenic agents
Hemoglobinopathies
Past Medical History
W.H.O. Group II
Left heart disease
W.H.O. Group III
Lung diseases and/or hypoxemia
W.H.O. Group IV
Chronic thromboembolic PH
W.H.O. Group V
Unclear multifactorial mechanisms
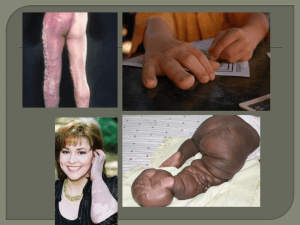
Heritable pulmonary arterial hypertension
Dresdale, 1953 reported family
NIH Registry, 1987: 6% with one or more
affected family members
Autosomal dominance
Fetal wasting
Genetic anticipation
Incomplete penetrance
Idiopathic PAH - Epidemiology
• Female
• Young to middle age
• NIH Registry, 1991
Idiopathic PAH - Epidemiology
Distribution of patients with pulmonary arterial
hypertension according to age based on sex
Pulmonary Arterial Hypertension in France
Results from a National Registry
Am. J. Respir. Crit. Care Med 2006, 173:1023
Congenital Heart Disease
Epidemiology
Shear stress from increased pulmonary blood flow
Increased pulmonary artery pressures
Majority of unrepaired truncus arteriosus develop PH
Large VSD, 50% develop PH
ASD, 10% develop PH
Eisenmenger’s syndrome
Medical or surgical therapy effective
Connective Tissue Diseases
Epidemiology
-Limited systemic sclerosis
o SLE, MCTD, RA, Sjogren’s
Survival Curves of Scleroderma Patients with Pulmonary
Hypertension, Lung Involvement, or No Major Organ Involvement
100
Survival, Percent
90
80
70
None
60
50
Lung Involvement
(without PH)
40
30
20
PH
10
0
0
1
2
3
4
5
6
7
8
9
10
11
Years from Diagnosis of PH
Koh,
Koh, et al. Br J Rheumatol.
Rheumatol. 1996;35:9891996;35:989-993
12
13
HIV
Epidemiology
0.5% prevalence– no decline since HAART
Occurrence depends upon length of infection, not CD4 count or prior opportunistic infections
Portopulmonary Hypertension
Epidemiology
-2-6% prevalence in cirrhotics, higher in liver transplant candidates (8%)
-Risk increases with duration of portal hypertension
-High cardiac flow states and LV diastolic dysfunction complicate PH
Portopulmonary Hypertension: Survival - 21st Century
Le Pavec J et al. Am J Respir Crit Care Med 2008
Pulmonary Hemodynamic Scenarios in the Setting of Portal Hypertension
Type
MPAP
PAOP CO
PVR TPG
↑
n
↑
↓
n
II. Increased pulmonary venous vol. ↑
↑
↑
↓
n
↑
↓
↑
↑
↑
↑
↑
↑
↑
↑
I. Hyperdynamic, high flow state
III. Portopulmonary hypertension
Pulmonary vascular obstruction;
normal volume
Pulmonary vascular obstruction;
excess volume
M Krowka. Medscape Cardiology 2006
Associated Drugs and Toxins
Epidemiology
Definite:
Appetite suppressant drugs (anorexigens)
Fenfluramine and dexfenfluramine
Aminorex
Toxic Rapeseed Oil
Likely:
L-tryptophan
Methamphetamine
Cocaine
Hemoglobinopathies
Epidemiology
Sickle cell disease
•
•
•
•
•
•
PH 10-30%
Yearly echocardiogram
50% - 2 year mortality with PH
Thromboembolic disease
Restrictive pulmonary disease
Left heart disease
Homozygous beta-thalassemia
Hereditary spherocytosis
Chronic ThromboEmbolic
Pulmonary Hypertension (CTEPH)
Cumulative Incidence
Historically considered rare:
0.1-0.5% of acute, non-fatal pulmonary embolism:
Fedullo PF et al. N Engl J Med 2001
6 months
1.0%
12 months
3.1%
24 months
3.8%
Pengo V, et al NEJM 2004
Past Surgical History
Lung resection
Thyroidectomy
Splenectomy
CABG
Cardiac valve repair/replacement
Repair of congenital heart defect
Family History
Pulmonary hypertension
CHF/sudden cardiac death at a young age
Sarcoid
Connective tissue disorders
Clotting disorders – DVT, PE, CVA
Social History
Tobacco
ETOH
Recreational Drugs
methamphetamines
Cocaine
IVDU
Prescription diet pills
Bush tea
Pets (birds)
Social Network – “Friends and Family”, not “Verizon”
Allergies /Adverse Reactions
Beware of hypotensive response to vasodilators
CCBs
Nitrates
Sildenafil
Medications
Nitrates
Calcium channel blockers
Warfarin
Beta blockers
Oxygen
Diuretics
Digoxin
Medications
ERAs (Bosentan)
Hepatotoxins – monitor LFTs, Hgb
Glyburide may increase risk of hepatoxicity
Cyclosporine
Ketoconazole
Statins
Warfarin
(Ambrisentan*)
Medications
PDE V Inhibitors
• Sildenafil (Revatio)
• Tadalafil (Adcirca)
Medications
Prostacyclins
Parenteral
ng/kg/minute
ml/24 hrs
Route of administration
Inhaled
mcg/dose
frequency
Inhaled Iloprost (Ventavis)
TYVASO Inhalation System
1. Inhalation device
assembled
2. Measuring cup
3. One inhaled treprostinil
ampule
Mouthpiece
Inhalation piece
4. Carrying case provided
Filter shell
Device base
25
Review of Systems
Neurologic: Headache, prior TIA/CVA, lightheadedness
or syncope
HEENT:
Epistaxis, dry eyes, dry mouth, oral ulcers.
CV:
Anginal quality chest pain, orthopnea,
PND, palpitations, peripheral edema
Rheumatologic: Joint pain or swelling, Raynaud’s
phenomenon
GU/Gyn: Hematuria, Gravida : Para (spontaneous
abortions)
GI:
Liver disease, dysphagia, heartburn,
hematemesis, varices or hemorrhoids, ascites
Review of Systems
Hematologic/Lymphatic: DVT, PE, CVA, TIA
(hypercoaguable state) swollen lymph glands
(Sjogren’s, sarcoid)
Dermatologic: Rashes, skin lesions, painful ulcers on
fingertips.
Psychiatric: Confusion, memory loss, depression,
anxiety
HIV risk factors: Blood transfusions, known contacts,
HIV serum test (date)
Sleep:
Snoring, witnessed apneas, restless sleeper,
awakens unrefreshed, daytime hypersomnolence
Physical Examination
Jugular venous distention at 45o
Widened split S2
Loud pulmonic valve closure (P2)
TR murmur
Right ventricular heave, PA pulsation
Enlarged, pulsatile liver – hepatojugular reflux
Peripheral edema, ascites
Skin/Mouth:Telangiectasias, spider hemangiomas
*Infusion catheters and site problems
Guidelines for evaluating pulmonary hypertension
Barst, R. J. et al. J Am Coll Cardiol 2004
Laboratory evaluation
IVS
RV
LV
RA
LA
INCREMENTAL SHUTTLE WALK TEST (ISWT)
CPT code (pulmonary stress testing): 94620
Date
___/____/_____
ISWT: mls/JPA (7/09) page 1/1
Ordering physician
Patient name _____________________________
M. Scharf
Date of birth _____________
Patient indices
BP
HR
Dyspnea
Fatigue
SpO2
Pre-test
Post-test
______ mmHg
______ /min
______
______
______%
______ mmHg
______ /min
______ (Borg scale, 0-10)
______ (Borg scale, 0-10)
______%
Supplemental O2:
____ No
____ Yes, ____ L/min
ISWT results
Number of laps ______ x 10 m + _____ m (partial lap) = _____ m, total distance shuttled
Lap counter: place a vertical line below corresponding for each 10 m lap shuttled
Symptoms experienced during testing
____ none
____ yes
____ angina
____ lightheadness/dizziness
____ hip/leg/foot pain
____ other, explain ____________________________________________
Interpretation
No
Mild
Moderate
Severe
Exercise limitation
Exercise-induced hypoxemia:
______Yes
______ No
Reviewing physician M. Scharf
Reviewing physician signature (on file)
Patient name ___________________________
Physican(s) requested:
Fischman, Savage, or Wolinsky
Date of birth __________________________
Date of order _______________________________
Cardiac Catheterization Evaluation for
Pulmonary Artery Hypertension
o Right heart catheterization only
Diagnostic,
To detect PAH at rest
o Right heart catheterization with exercise
(PA mean <= 25 mmHg and Pcw<=18 mmHg)
Diagnostic,
To detect PAH with exercise
o Exercise challenge
o Right heart catheterization
(PA mean > 25 mmHg and Pcw <= 18mmHg):
Assess vasodilator
responsiveness
o inhaled NO protocol
o Right heart catheterization with
(PA mean >25 mmHg and 12< Pcw <= 18 mmHg)
To assess for occult diastolic
diastolic dysfunction in PH
o Exercise or NS fluid challenge
o Right heart catheterization with “O2 sat run”
Assess for shunt
o Left heart catheterization
o Measure LVEDP
(At discretion of cath physician)
To confirm Pcw accuracy
o Coronary angiogram
CAD
o LV gram
Pump, valves
Ordering physician ___________________________
Signature of physician ________________________
Cardiac Cath Evaluation for PAH. MLS/Jefferson Pulmonary Associates 5/10
Impression
1. (Suspected) Pulmonary (arterial) hypertension
(with/without) right ventricular dysfunction due to
__________: W.H.O. Functional Class 1 - 4
2. Other conditions contributing to cardio-respiratory
complaints
Recommendations and Plan
Defend you reason for your assessment
Defend your reason for testing ordered
Defend your reason for medical therapy
One paragraph per “Impression #”
Write so that the referring doctor will understand
Write so you may use this note as a reminder for what
you wish to do at next visit.
Jefferson Heart Institute – follow-up
Tools for Patients
Cardiology nurses for RHC teaching
PH literature tearouts
Teaching aides – RHC booklets
Parenteral infusion CDs
Inhalation device models
Tools for Fellows/Faculty
• Pulmonary order sheets
– Sleep lab
– Pulmonary function lab
PH Reading List
Projects
• ISWT - PAH
– retrospective: ongoing
– prospective: needs design
– other groups, e.g. pre-op assessment – needs collaboration with Surgery
• CT evaluation of PAH and RVD in subjects with PH W.H.O.
Group 1 – collaboration with Radiology: ongoing
• Echocardiographic evaluation of RV function in PH subsets –
collaboration with cardiology, ongoing.
• PROSPECT Registry
Thank you!