Deep space infections of the neck and floor of mouth (28 Jan 2009)
advertisement

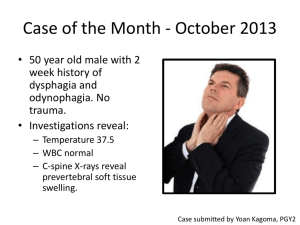
Deep space infections of the neck and floor of mouth Dr David Maritz Introduction • Penicillin 1940’s • Odontogenic infections • Deep anatomic fascial space • Threaten vital structures Introduction • Most important: • Submandibular • Lateral Pharyngeal • Retropharyngeal / Danger / Prevertebral • Clinical examination underestimate extent in 70% Potential pathways of extension of deep fascial space infections of the head and neck Fascial spaces around the mouth and face Figure 69-4 Natural progression of dental infection. The pathways by which such infections may travel are: 1, postzygomatic (from canine fossa in cuspid and bicuspid region; pterygomaxillary fossa communicates from rear); 2, vestibular; 3, facial; 4, submandibular; 5, sublingual; 6, palatal; 7, antral; 8, pterygomandibular; 9, parapharyngeal; 10, masseteric. (Redrawn from Rose LF, Hendler BH, Amsterdam JT: Temporomandibular disorders and odontic infections. Consultant 22:125, 1982.) Downloaded from: Rosen's Emergency Medicine (on 15 January 2009 05:57 PM) © 2007 Elsevier Clinical examination of odontogenic infections Stages of infection • 4 stages • Inoculation Cellulitis Abscess Rupture • Spreading odontogenic infection Trismus • Inability to open mouth widely • Inflammation muscles of mastication • Masticator space / Pterygomandibular space • Difficult intubation Airway / Physical evaluation • Pharyngeal swelling – difficulty swallowing • Difficulty sleeping supine • Sniffing position – Retropharyngeal space • Head deviated to opposite side – Lateral pharyngeal space • Muffled voice – Epiglottitis • Distant quality to voice – Retropharyngeal / Lateral Pharyngeal • Elevated tongue – Sublingual space Intraoral examination • • • • • • • Caries Swellings of oral vestibule Periodontal disease Tooth mobility Pericoronitis Swellings Position of uvula Radiographic evaluation • Rapid CT scanners • Contrast enhanced CT • Postero-anterior / lateral soft tissue x-rays of neck • Dental panoramic view (Orthopantomogram) Lateral radiograph of the neck Figure 69-5 Periapical abscesses (arrows) as seen on Panorex film. Downloaded from: Rosen's Emergency Medicine (on 15 January 2009 06:07 PM) © 2007 Elsevier Culture and sensitivity testing • Penicillin resistance 30 – 50% 1. Submandibular Space Introduction • ‘’Ludwigs angina’’ • ‘’Angina maligna’’ • ‘’Morbus strangulatorius’’ • ‘’Garotillo’’ Early appearance of patient who has Ludwig’s angina with characteristic submandibular ‘’woody’’ swelling Anatomy and pathogenesis • Sublingual and submylohyoid spaces • Odontogenic ( periapical abscesses of mandibular molars – 2nd / 3rd) • Communicate freely: • Entire submandibular space • Buccopharyngeal gap – lateral pharyngeal space – retropharyngeal space Anatomic relationships in submandibular infections Routes of spread of odontogenic orofacial infections along planes of least resistance Clinical manifestations • Mouth pain / stiff neck / drooling / dysphagia • No trismus • Woody inflammation • No lymph node involvement • Protruding tongue Ludwig's Angina • Involvement submandibular spaces bilaterally and submental space in midline • Rapid spread to lateral pharyngeal / retropharyngeal space • Rapidly obstruct upper airway Early Ludwig's angina Early Ludwig's angina Submandibular space abscess and Cellulitis Potential complications • Airway compromise • Spread into the lateral pharyngeal space and beyond Figure 69-6 Extensive spread of infection of odontogenic origin involving masseteric, sublingual, submental, and submandibular spaces with extension to mediastinum. A, Preoperative. B, Postoperative. Note drainage from mediastinum. (From Guernsey LH: Practical problem solving in oral surgery. In Cohen DW [ed]: Continuing Dental Education, vol 2, suppl 10. Philadelphia, University of Pennsylvania School of Dental Medicine, 1979.) Downloaded from: Rosen's Emergency Medicine (on 15 January 2009 06:09 PM) © 2007 Elsevier Figure 69-6 Extensive spread of infection of odontogenic origin involving masseteric, sublingual, submental, and submandibular spaces with extension to mediastinum. A, Preoperative. B, Postoperative. Note drainage from mediastinum. (From Guernsey LH: Practical problem solving in oral surgery. In Cohen DW [ed]: Continuing Dental Education, vol 2, suppl 10. Philadelphia, University of Pennsylvania School of Dental Medicine, 1979.) Downloaded from: Rosen's Emergency Medicine (on 15 January 2009 06:07 PM) © 2007 Elsevier Therapeutic considerations • Mixed infection – synergistic interaction • Immunocompromised • MRSA • Candida / Aspergillus 2. Lateral Pharyngeal Space Potential pathways of extension of deep fascial space infections of the head and neck Anatomy and pathogenesis • Anterior / muscular compartment • Posterior / neurovascular compartment • Carotid sheath • 9 to 12 cranial nerves • Sympathetic trunk • Peritonsillar abscesses Clinical manifestations • Anterior compartment • Dysphagia • Trismus • pain • Posterior compartment • No trismus • Neurologic / vascular • Edema epiglottis / larynx Abscess of lateral Pharyngeal space Potential complications • NB: Posterior compartment • Laryngeal edema • Vagal nerve • Horner's syndrome • Cranial nerve palsies • Suppurative jugular thrombophlebitis (lemierre syndrome) • Carotid artery erosion Lemierre’s Syndrome • Septic thrombophlebitis of internal jugular vein • Septic emboli – lung / liver abscesses / septic arthritis • Fusobacterium necrophorum Jugular venous thrombosis Therapeutic considerations • Suppurative • Posterior more conservative • Anterior more aggressive treatment 3. Retropharyngeal / Prevertebral / Danger Space Introduction • Caudal extension of infection • Considered together Anatomy and pathogenesis • Between pharynx-esophagus and spine • Delineated by fascial planes: 3 layers of deep cervical fascia Retropharyngeal space • Base skull to C7 / T1 • Mediastinal spread • Pleural / pericardial spread • Deep cervical chain of nodes in children • Other causes eg: oesophageal instrumentation, foreign bodies…. Retropharyngeal abscess Retropharyngeal space Danger space • Base skull to diaphragm • Contiguous spread from adjacent spaces Prevertebral space • Between prevertebral fascia and vertebral bodies • Base skull to coccyx • Contiguous with psoas muscle sheath • Haematogenous spread NB • Local instrumentation • Contiguous spread • Different microbiology Clinical manifestations Retropharyngeal danger space • Sore throat / dysphagia / stiff neck • Upper airways obstruction • Head tilt contralateral side • Pleuritic chest pain • Bulging posterior oropharynx Lateral radiograph of the neck Prevertebral space • Spinal cord compression • Epidural abscess Potential complications • Laryngeal inflammation • Rupture with aspiration • Descending necrotizing mediastinitis • Pyothorax / pericardial involvement • Spinal epidural collections • Psoas muscle infection Therapeutic considerations • Retropharyngeal / danger space: • Adequate anaerobic / oral gram + cover • Surgery if indicated • Prevertebral: • Surgical drainage • NB gram + / MRSA / gram - rods 4. Buccal space • Subcutaneous space • Connects to: infraorbital space, periorbital tissues, superficial temporal space • Hemophilus influenzae Cellulitis: • Children • Recent URTI / sinusitis Buccal Cellulitis (Hib) 5. Infraorbital space • Lower lid / periorbital swelling • Point medially (inner canthus) or laterally (lateral canthus) • Septic thrombophlebitis angular vein → cavernous sinus 6. Orbital space • Preseptal Cellulitis • Subperiosteal abscess (orbital wall) • Orbital Cellulitis / abscess → optic nerve damage / cavernous sinus thrombosis 7. Vestibular space • Diffuse facial swelling • Elevation of the oral vestibule • Potential space between oral mucosa and muscles facial expression • Draining sinus 8. Subperiosteal space • Dental infection • Perforates cortical layer but not periosteum • Eg: mandibular subperiosteal infection 9. Submental space • Secondary spread from submandibular space 10. Masticator space • Severe trismus • Surrounding muscles of mastication Masticator space infection with trismus Masticator space abscess 11. Temporal space • Trismus (infratemporal fossa – part of masticator space) • Cavernous sinus thrombosis Deep temporal space infection with spread to parotid space Treatment The admission decision • Airway issues • High fever • Dehydration • Need for I+D • Inpatient control systemic disease • Immune compromise Airway security • Protect against aspiration • ETT ruptures abscess • Trismus / Swelling • Maintain airway reflexes during intubation Surgical treatment • Gravity dependent surgical drainage • Antibiotics secondary • Tooth extraction Antibiotic therapy • Predominately anaerobic nature • Initially: aerobic streptococci ( penicillin ) • Later: anaerobic bacteria ( penicillin resistant ) • Synergistic interaction Complications Mediastinitis • Airway security • Contrast CT • Open thoracotomy • Broad spectrum antibiotics Cavernous sinus thrombosis • Ascending septic thrombophlebitis • Anterior route – angular vein (infraorbital space) • Posterior route – facial vein (buccal space) • Congestion retinal veins • CN 6 paresis → ophthalmoplegia / blindness • Severe orbital / periorbital / infraorbital swelling Cavernous Sinus Thrombosis • Treatment: • • • • Tooth extraction root canal Drainage deep spaces High dose IV antibiotics Anticoagulation Summary • Preventative dental care • Effective antibiotics