Infestation and Infection of GIT + Parasitic Infections of - PBL-J-2015
Giardia lamblia
• Is a microscopic parasite that causes diarrhoeal illness known as giardiasis.
• Found on surfaces or in soil, food or water that has been contaminated with faeces
• It may be passed from person-to-person or even animal-to-person
• Incubation period is 1-2 weeks
• Symptoms include watery diarrhoea, abdominal cramps, nausea, flatulence, dehydration
• MOA = attaches to mucosa of small intestine: epithelia cells are damaged affecting transport and absorption
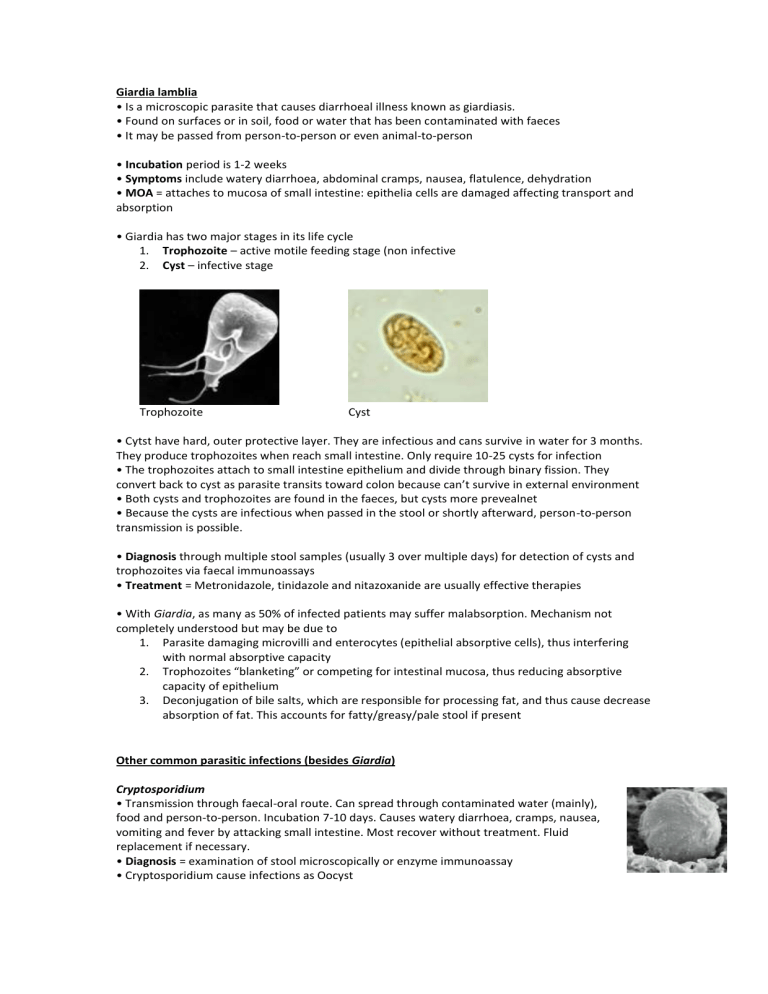
• Giardia has two major stages in its life cycle
1.
Trophozoite – active motile feeding stage (non infective
2.
Cyst – infective stage
Trophozoite Cyst
• Cytst have hard, outer protective layer. They are infectious and cans survive in water for 3 months.
They produce trophozoites when reach small intestine. Only require 10-25 cysts for infection
• The trophozoites attach to small intestine epithelium and divide through binary fission. They convert back to cyst as parasite transits toward colon because can’t survive in external environment
• Both cysts and trophozoites are found in the faeces, but cysts more prevealnet
• Because the cysts are infectious when passed in the stool or shortly afterward, person-to-person transmission is possible.
• Diagnosis through multiple stool samples (usually 3 over multiple days) for detection of cysts and trophozoites via faecal immunoassays
• Treatment = Metronidazole, tinidazole and nitazoxanide are usually effective therapies
• With Giardia, as many as 50% of infected patients may suffer malabsorption. Mechanism not completely understood but may be due to
1.
Parasite damaging microvilli and enterocytes (epithelial absorptive cells), thus interfering with normal absorptive capacity
2.
Trophozoites “blanketing” or competing for intestinal mucosa, thus reducing absorptive capacity of epithelium
3.
Deconjugation of bile salts, which are responsible for processing fat, and thus cause decrease absorption of fat. This accounts for fatty/greasy/pale stool if present
Other common parasitic infections (besides Giardia)
Cryptosporidium
• Transmission through faecal-oral route. Can spread through contaminated water (mainly), food and person-to-person. Incubation 7-10 days. Causes watery diarrhoea, cramps, nausea, vomiting and fever by attacking small intestine. Most recover without treatment. Fluid replacement if necessary.
• Diagnosis = examination of stool microscopically or enzyme immunoassay
• Cryptosporidium cause infections as Oocyst
Entamoeba histolytica
• Most common cause of parasitic diarrhoea in the world
• Transmitted through faecal-oral route. Can spread through contaminated food, water and surfaces. Incubation 7-21 days. Causes bloody diarrhoea and abdominal pain. By attacking small intestine. Can also cause ulcers in large intestine. Treated with metronidazole
• Diagnosis = stool samples and serology tests
• Life-cycle similar to Giardia in that it has both trophozoite and cyst phase. Cysts are infectious.
Helminths
• Diagnosis for all below = stool microspcopy for eggs
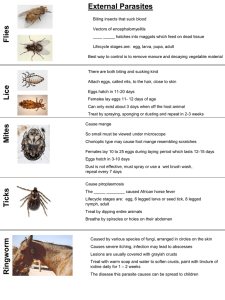
Hookworm
• Hookworm disease caused by Necator americanus or Ancylostoma duodenale
• Found in tropical and subtropical climates
• MOA/life-cycle: adult eggs are passed in faeces, larvae then develop in faeces and/or soil, infective larvae then penetrate skin where they enter circulation and are carried to lungs, they are eventually coughed up and swallowed into small intestine where they mature into adults, adult worm can lay eggs which pass through faeces and cycle starts again
• Symptoms: rash + itch at entry site, adult worms can cause abdominal pain and diarrhoea
• Treatment: Mebendazole to treat and preventative measures such as improved sanitisation and wearing shoes
Strongyloides sterocoralis (threadworm)
• Found in tropical and subtropical climates
• MOA/life-cycle: Similar to hookworm except eggs hatch into larvae in intestinal mucosa before being passed in faeces. These larvae mature directly into infective larvae and can penetrate the intestinal mucosa (autoinfection) or enter a non-parasitic (or free-living cycle) outside human host
• Symptoms: rash + itch at site of entry, abdominal pain, nausea, episodes of diarrhoea and costipation
• Treatment: Ivermectin for treatment and preventative measures as for hookworm
Ascaris lumbricoides (roundworm)
• Found throughout world, but particularly in areas of poor sanitisation
• Faecal oral transmission
• MOA/life-cycle: adult worms live in small intestine, female may produce appx. 200,000 eggs per day which are passed in faeces and can be either unfertilized (non-infective) or fertilized (infective). After infective eggs swallowed, larvae hatch, penetrate intestinal mucosa and reach bloodstream where they are carried to lungs, further mature in lungs, get coughed up and swallowed back into small intestine where they develop into adult worms which can then lay eggs and cycle starts again
• Symptoms: asymptomatic, but if show symptoms vomiting and abdominal discomfort may occur + intestinal obstruction or malnutrition
• Treatment: mebendazole, albendazole or piperazine
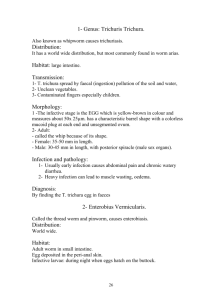
Enterobius vermicularis (pinworm)
• MOA/life-cycle: eggs are deposited or perianal area, infection occurs by scratching area and putting hands near mouth where infective egg enters (eggs also be acquired off surfaces), following ingestion of eggs larvae hatch in small intestine and adults establish themselves in colon
• Symptoms: asymptomatic, but if show symptoms perianal pruritus and abdominal discomfort
• Diagnosis: touch perianal area with tape to collect eggs then use microscopy
• Treatment: mebendazole
Trichuris trichiura (whipworm)
• MOA/life cycle: unembryonated eggs passed in faeces, eggs develop in soil to become infective, swallowed, larvae hatch in small intestine, move to colon and adult worm lives in cecum and ascending colon. Female produces eggs and cycle begins again
• Symptoms: asymptomatic, but can have diarrhoea, abdominal pain with heavy infection. And anaemia and growth retardation in children with heavy infection
• Treatment Mebendaole or albendazole