Goal Directed Patient Assessment
advertisement
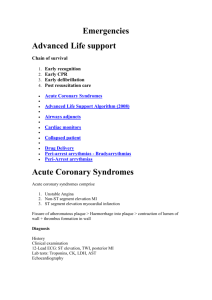
Goal Directed Patient Assessment Dan Batsie dbatsie@apems.org • How is an EMT different than a taxi driver? Goals of the EMT • • • • • • Go home Identify resuscitation Identify/intervene in immediate life threats Identify ongoing (subtle) life threats Symptom relief Customer service Dr Reuben Strayer Bottom Up Approach Bottom Up Approach • • • • • • Final diagnosis Ancillary testing Differential diagnosis Diagnostic testing Comprehensive physical examination Comprehensive history •Symptoms •Allergies •Medications •Past medical history • Last meal • Events • What’s wrong with the patient? • What does the patient need? iv. Specific respiratory conditions—definition, causes, assessment findings and symptoms, complications, and specific prehospital management and transport decisions A. Asthma B. Pulmonary Edema C. Chronic Obstructive Pulmonary Disease D. Pneumonia E. Spontaneous Pneumothorax F. Pulmonary Embolism G. Epiglottis H. Pertussis I. Cystic Fibrosis J. Environmental/Industrial Exposure/ Toxic Gasses K. Viral Respiratory Infections Asthma Pulmonary edema COPD Pneumonia Spontaneous pneumo. PE Epiglottitis Cystic fibrosis Pertussis Respiratory infections Toxins Although there are many pathologies to consider, the emergent needs of the patient are relatively few. Interventions Medications 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 1. 2. 3. 4. 5. 6. 7. 8. Restraints CPR Defibrillation Hemorrhage control Foreign body airway/suction NPA/OPA BIAD PPV CPAP Supplemental O2 Splinting/immobilization Cool/warm Childbirth Transport Request ALS PASG Wound care/bandaging O2 Epi auto-injector Albuterol Charcoal Aspirin Nitronox Glucose NTG Simple ≠ Dumb Top Down Approach (What does the patient need?) • Safety • Identify the need for resuscitation/correction of a primary assessment problem • Identify the need for other immediate action • Identify life threatening conditions • Symptom relief • Customer service Primary Assessment 1. 2. 3. 4. Airway Breathing Circulation Disability Primary Assessment 4. 1. 2. 3. Circulation Airway Breathing Disability Primary Assessment Circulation Airway Breathing Disability Circulation What are the goals of our assessment? Primary Assessment Is it safe? Primary Assessment ID Resuscitation Prevent Hypoxia Prevent Hypoperfusion EXsanguinating hemorrhage Airway Breathing Circulation Disability Massive hemorrhage Airway Respiration Circulation Hypothermia/Head injury Airway • Is it open? • Will it stay open? X A B C D Prevent Hypoxia Initial Assessment Revisited Breathing Is it adequate? <8 >20 Breathing Adequacy • Oxygenation • Ventilation Identify Respiratory Failure Bad signs • Hypoxia despite O2 • Hypercapnia • Poor tidal volume • Anxiety/Combativeness Super bad signs • Tiring • Rate changes • Respiratory pattern changes • Lethargy, somnolence • Silent chest Are the perfusing? Prevent Hypoperfusion Do we need to leave right now? • Airway • Breathing • Circulation • Disability • Expose • Fit into CUPS • Get Vitals • History/Head to Toe • Scene Survey • Primary Assessment – ABCD • Secondary Assessment – History • OPQRST, SAMPLE – Physical • Diagnostic testing • Reassess • Safety • Resuscitation • Correction of a primary assessment problem • Identification of life threatening condition • Symptom relief • Customer service Secondary Assessment • Not important if interventions are necessary or ongoing • May not be an achievable goal. Assessment is more than just identifying interventions N Engl J Med, Vol. 345, No. 19 Every 10 minute increase in the time to reperfusion therapy increases mortality by 1% Missed AMI doubles mortality Eastern Maine Medical Center Average Door to Balloon Time 2011: • • • • Self transported - 70.56 min. EMS Transported with activation - 40.29 min. ED Bypass- 16 min. EMS transported without activation - 77.69 min. EMT’s don’t diagnose! Cardinal Presentations iv. Specific respiratory conditions—definition, causes, assessment findings and symptoms, complications, and specific prehospital management and transport decisions A. Asthma B. Pulmonary Edema C. Chronic Obstructive Pulmonary Disease D. Pneumonia E. Spontaneous Pneumothorax F. Pulmonary Embolism G. Epiglottis H. Pertussis I. Cystic Fibrosis J. Environmental/Industrial Exposure/ Toxic Gasses K. Viral Respiratory Infections iv. Specific respiratory conditions—definition, causes, assessment findings and symptoms, complications, and specific prehospital management and transport decisions A. Asthma B. Pulmonary Edema C. Chronic Obstructive Pulmonary Disease D. Pneumonia E. Spontaneous Pneumothorax F. Pulmonary Embolism G. Epiglottis H. Pertussis I. Cystic Fibrosis J. Environmental/Industrial Exposure/ Toxic Gasses K. Viral Respiratory Infections Asthma Pulmonary edema COPD Pneumonia Spontaneous pneumo. PE Epiglottitis Cystic fibrosis Pertussis Respiratory infections Toxins • Ask questions to get answers • Use history to make decisions • One question leads to the next • Questions are used to narrow your focus Don’t ask a questions if you already know the answer. 1 Question • Are you sexually active? • Is there a wheeze? Is there a wheeze? How long has this been going on? Do you still have your appendix? Have you had a fever? Do you have CHF? Are you a diabetic? Have you ever had kidney stones? Do you feel the urge to push? How far did you fall? Were you trying to hurt yourself? Any hives? Have you ever had a seizure before? How fast were you going? When did this start? When was the last time you were normal? Do you have asthma? Did you just eat a greasy meal? How big was the knife? Are you able to speak? Do you still have your appendix? What exactly did you take and how much? Ripping or tearing pain? Are you a smoker? Have you urinated/moved your bowels recently? Are you allergic to… Are you sexually active? Have you been coughing? Has this ever happened before? Any recent injuries/illness? Can you describe the pain? Do you have any pain? Is anyone else sick in the house? Do you take an ED medication? Do you have a history of alcohol abuse? Turn possibilities into probabilities General Impression Primary Assessment History Field Diagnosis History Physical Exam Better Diagnosis Assemble the Pattern Use physical exam and specific diagnostic testing to prove your conclusions Other Important and often forgotten goals Patient safety Symptom Relief Symptom relief? • Can be done without diagnosis • Not always an ALS procedure Cool Air and Dypsnea • Stimulation of mechanoreceptors mediated through the trigeminal nerve on the face may alter afferent feedback and modify the perception of dyspnea. • Shown to reduce dyspnea in normal volunteers in response to hypercapnia and inspiratory resistive loads Schwartzstein, R. et al. Cold facial stimulation reduces breathlessness induced in normal subjects. Am. Rev. Respir. Dir. 13658-61 1987 Customer service Customer service Questions? Dan Batsie dbatsie@apems.org • Scene Survey • Primary Assessment – ABCD • Secondary Assessment – History • OPQRST, SAMPLE – Physical • Diagnostic testing • Reassess • Safety • Resuscitation • Correction of a primary assessment problem • Other immediate action • Identification of life threatening condition • Symptom relief • Customer service What are the goals of our assessment? Primary Assessment Airway Breathing Circulation Disability CPR Airway PPV Hemorrhage control Seal chest wounds Transport N Engl J Med 2004;351:647-56. • • • • • • Symptoms Allergies Medications Past medical history Last meal Events • What’s wrong? (symptoms/events) • Has this ever happened before? (PMHx) • Allergies • Medications • Last meal