Everyday Mindfulness - Department of Family and Community
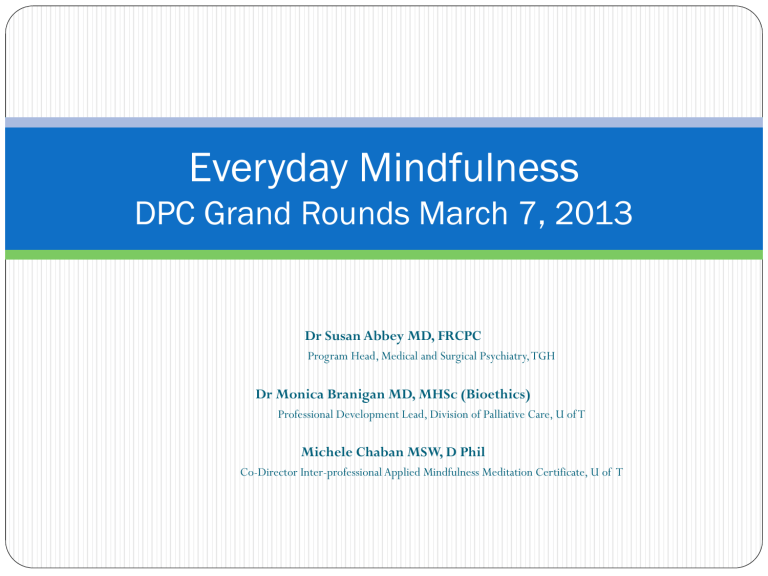
Everyday Mindfulness
DPC Grand Rounds March 7, 2013
Dr Susan Abbey MD, FRCPC
Program Head, Medical and Surgical Psychiatry, TGH
Dr Monica Branigan MD, MHSc (Bioethics)
Professional Development Lead, Division of Palliative Care, U of T
Michele Chaban MSW, D Phil
Co-Director Inter-professional Applied Mindfulness Meditation Certificate, U of T
My intention
To create community around mindfulness in palliative care
Objectives
Discuss simple mindfulness interventions designed to benefit practitioners
Review interventions of benefit for people dealing with life threatening illness
Consider mindful questions to address pain and suffering
How can we cultivate mindfulness?
Paying attention we can bring awareness to
Mind
Heart
Body
Each center is associated with different ways of knowing, listening and speaking
Each functions from a different place
Neocortex
Limbic system
Brainstem
The head center
Our thinking center
Knowing through rational thought
Listen to content: description, explanation, story, beliefs, assumptions
Speaking: “I think...”
Values: control
Pitfalls: critique, judgment,
“I already know”
Pamela Weiss
The heart center
Our feeling center
Knowing through openness, attunement, acceptance
Listening to feelings, emotions, mood
Speaking: “I feel....”, “I am angry....”
Value: approval
Pitfalls: emotional reactivity- entanglement or distancing
Pamela Weiss
The body center
Our sensing center
Knowing through intuition, perception
Listen to energetic tone, physical cues
Speaking: “I sense......”
Value: safety
Pitfalls: tension, agitation, flight, fight or freeze
Pamela Weiss
The three centers from our patient’s point of view
Mind: tell me what I can do to make the pain better and give me an explanation that makes sense to me
Heart: let me know that you accept my pain is real
Body: allow me to feel safe
The three centers from the provider point of view
Three part check in
Start with the body: big breath, relax shoulders down, expand back, sides, front
Bring awareness to your heart: feeling tone or mood
Notice your thoughts or general flavour: critical, curious….
2.
3.
Mindful approach to pain
1.
Begin with a three part check for yourself so you can meet the patient as a whole person
Invite the patient to check in with their three centers
Notice the energy between you and the patient- are you connected?
YES: together you work with “the pain”
NO: the patient remains alone with “their pain”
The Two Darts
"When an untaught worldling is touched by a painful (bodily) feeling, he worries and grieves, he laments, beats his breast, weeps and is distraught. He thus experiences two kinds of feelings, a bodily and a mental feeling. It is as if a man were pierced by a dart and, following the first piercing, he is hit by a second dart. So that person will experience feelings caused by two darts....
Sallatha Sutta
How do we usually approach pain?
The standard pain history
Major focus on the body- the first dart
Does not fully acknowledge the second dart
DISCONNECT: as HCPs we often may come from our head center and may ask that our patients respond from their body center
Questions for the mind
What do you think about when you have pain?
Where does your mind go when you have pain?
Are there any thoughts that trigger your pain?
Are there any stories that come to you when you have the pain?
What is the meaning of your pain?
Questions for the heart
Tell me about the pain in your heart.
How does your heart feel the pain?
What in your life is causing pain in your heart?
What is your heart feeling ?
Questions for the body
Standard pain history
Where do you feel the pain?
What words describe it?
What makes it better?
Etc
How does the rest of you body feel?
Are there parts of your body that experience comfort?
Do you sense that your body is trying to tell you something?
Commitments
May I check in with myself in order to bring my wholeness to the patient that I may see them as whole and not broken
May I expand my awareness of pain beyond the first dart and allow the patient to explore body, mind and heart
May I see my own frustration and helplessness as something that connects me to the patient and not use it against myself
Resources- MBSR
The MBSR Clinic
Location: Toronto General Hospital
Time: Monday morning, Monday afternoon or
Wednesday evening
Instructors: Dr. Susan Abbey and
Sarah Greenwood, RN, BScN
Cost: $75.00
Call: 416- 340-4452
MBSR and Mindfulness
Centre for Mindfulness in Medicine, Health Care and Society http://www.umassmed.edu/cfm/index.aspx
see for professional courses and teacher training and annual scientific conference
Communities of practice
Mindfulness Toronto http://mindfulnesstoronto.ning.com/ see for mindfulness courses, events, MBSR and sitting groups
See posted “Resources” on Community Space
Continuing professional development
Applied Mindfulness Meditation at the Factor Inwentash
Faculty of Social work http://www.socialwork.utoronto.ca/conted/certificate/mi ndfulnessmed.htm
Centre for Mindfulness Studies, Toronto http://www.mindfulnessstudies.com/
Insight Meditation Center- online http://www.insightmeditationcenter.org/programs/onlinecourses/
Continuing professional development
Being with Dying Program at Upaya http://www.upaya.org/bwd/
Metta End of Life Practitioner Program http://mettainstitute.org/EOLoverview.html
Mindful Practice: Focus on Serious and Life-Limiting Illness,
University of Rochester http://www.cvent.com/events/mindful-practice-focus-onserious-and-life-limiting-illness/event-summary-
9a33a7d3cfbe4e4993128c6c7aa1964e.aspx
Online meditation podcasts
UCLA Mindful Awareness Research Center http://marc.ucla.edu/body.cfm?id=22
Tara Brach, Buddhist meditation teacher http://www.tarabrach.com/audiodharma.html
Insight Meditation Centre http://www.audiodharma.org/series/1/talk/1762/
Dan Siegel http://brainsciencepodcast.com/bsp/meditation-and-thebrain-with-daniel-siegel-md-bsp-44.html
For patients
Mindfulness Based Cognitive Therapy (MBCT) for People with
Cancer
Facilitators: Dr. Mary Elliott, MD, FRCPC
Dr. Evan Collins, MD, FRCPC
Dates: TBA
Location: Pencer Centre Group Room, 18 th Floor, Princess Margaret
Hospital
How to register: Physician referral required. Please complete the attached referral form and send to sherene.tay@uhn.ca
or fax to
416-946-2047.
Fees: Course covered by OHIP.
For patients
MBSR at Wellspring http://www.wellspring.ca/Odette/Programs/Full-List-of-
Programs/Mindfulness-Based-Stress-Reduction.aspx
Let’s talk…….
monica.branigan@utoronto.ca