Clostridium difficile
advertisement

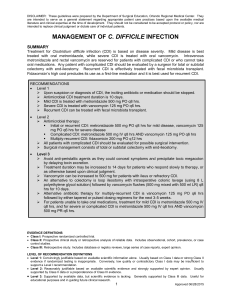
Clostridium difficile BATAM bijeenkomst 17 mei 2013 Dr DJ Bac, MDL-arts Dr MA Schouten, arts-microbioloog CDI • Berucht vanwege ribotype 027 • Diverse uitbraken sinds 2000 • Toename morbiditeit + mortaliteit + kosten CDI Clostridium difficile • • • • Gram positieve anaerobe staaf Produceert sporen Produceert toxines Nr 1 oorzaak nosocomiale diarree Risk factors clostridium difficile • Ziekenhuis opname • Antibiotica: • > 65 jaar • • • • • • • IBD PPI ?? sonde voeding diverticulose chemotherapie (GI) chirurgie dialyse Epidemiologie clostridium difficile Drager • Gezonde personen • Ziekenhuis • Jonge kinderen ~3% ~20% tot 80% Diarree • Hospital-acquired: • Community-acquired: ~ 10 % ~ 1,5-2 % 1e lijns probleem? • Clostridium difficile infection: it’s a family affair UK 2007-2012: 238 patiënten met CDI; verspreiding na ontslag? slechts in 3 gevallen verspreiding thuis (1) • Community-associated Clostridium difficile infection: How real is it? (2) Studie CDC: CA= diarree niet voorafgegaan door ziekenhuis bezoek afgelopen 3 maanden, >10.000 gevallen; 32% CA: hiervan 25% opgenomen na vaststellen CDI, recurrence rate 9%, PFGE type NAP1, NAP11, NAP4 Risicofactoren CA CDI: AB gebruik, protonpomp remmers literatuur: vlees, huisgenoten met CDI, kinderen < 2 jaar. 1: ICHE 2013, 2: Anaerobe 2013 1e lijns probleem? • Clostridium difficile carriage in healthy infants in the community asymptomatisch dragerschap volwassenen 1-7% Kinderen tot 2 jaar 2-75% drager maar zelf zelden ziek Studie: 10 gezonde kinderen van 1 jaar gevolgd + screening 2 dagopvangcentra Alle 10 verwerven CD en bleven maanden POS Dagverblijf 45% van de 85 kinderen CD POS Risicofactoren: ab gebruik, gebruik ab moeder zwangerschap, verandering voeding (met name bij verdwijnen Bifidobacterium cave melk / BV minder CD, flesvoeding meer CD) Geen relatie met aantal siblings of dieren Recente ziekenhuis opname enige risicofactor voor kolonisatie pathogene stam CID 2012 1e lijns probleem? • Clostridium difficile contamination of public tap water distribution system during a waterborne outbreak in Finland • Nov-dec 2007 drinkwater Nokia gecontamineerd met rioolwater • Grote uitbraak gastro-enteritis; Rol Clostridium difficile ? 10.000 inwoners, 8000 ziek, 1000 behandeld, 17 CD POS (65 getest) • 12 CD isolaten gevonden in water (5 kraanwater, 7 riool) • Aantal malen zelfde stam in water en patiënt SAGE 2013 Dieren • Clostridium difficile infection in the community: a zoonotic disease? (1) • Review LUMC; CD komt zowel bij mensen als dieren voor; verschillende biotypes • Bij vinden nieuwe types als verwekker humane infecties dan zoeken naar dierlijk reservoir • Clostridium difficile in faeces from healthy dogs and dogs with diarrhea (2) • Stockholm; 50 gezonde honden: 2 met CD; niet toxine producerend 20 honden met diarree: 2 met CD; toxine producerend, humane types 1: CMID 2012, 2: AVS 2013 Voeding • Detection of Clostridium difficile in retail ground meat products in Manitoba • 48 porties vlees (rund en varken); 6,3% CD POS • Verschillende types; wel allemaal bekend humane toxine producerende stamen JIDM 2012 DJB: klinisch beeld Diagnostiek • Gold standard: cytotoxicity assay • Kweek met toxine bepaling • Elisa (toxin A and or B, or GDH) – 72-92 % sensitiviteit – 89-98 % specificiteit • PCR – Sensitiviteit 92% – Specificiteit 96% • Sigmoidoscopy Behandeling • • • • De beste behandeling is nog steeds preventie! Lokaal: antibioticum formularium ZGV Gebaseerd op SWAB richtlijn SWAB weer gebaseerd op ESCMID “Infection control” strategie Rigorous hand hygiene Judicious use of antibacterial agents to preserve patients’ microflora Isolation of patients with faecal incontinence Barrier protection (e.g. gowns and gloves) Use of dedicated equipment for patients with CDI Environmental cleaning and disinfection Education of healthcare workers and visitors about CDI transmission Kelly & Lamont. NEJM 2008;359:1932–40 Vonberg et al Clin Microbiol Infect 2008;14(Suppl. 5):2–20 Behandeling: ESCMID recommendations: An initial mild episode of CDI • Discontinuation of the antibacterial treatment that induced CDI, if possible • Avoidance of treatments that reduce gut transit – e.g. opioids, including those used in diarrhoea relief (loperamide etc) • Provision of supportive care – e.g. fluid and electrolyte replacement • Observation for signs of clinical deterioration Bauer et al. Clin Microbiol Infect 2009;15:1067–79. Behandeling: ESCMID recommendations: First episode of CDI • • Aim of treatment is to eradicate C. difficile from the intestines and promote restoration of the normal colonic microflora Cessation of antibacterial therapy, if possible, is usually the first step Diagnosis ESCMID recommended treatment Non-severe first episode Metronidazole 500 mg tid orally for 10 days* Severe first episode Vancomycin 125 mg qid orally for 10 days (or teicoplanin 100 mg bid) IV metronidazole 500 mg tid for 10 days plus intracolonic vancomycin 500 mg in 100 mL saline every 4–12 hours and/or vancomycin 500 mg qid by nasogastric tube if oral therapy impossible * Intravenous (IV ) if oral therapy is not possible Bauer et al. Clin Microbiol Infect 2009;15:1067–79. Behandeling (10-14 dgn) • Metronidazol 3 dd 500 • Vancomycine 4 dd 125-500 mg • • • • • • • • • • eerste keus: po en iv geen selectie VRE Goedkoop vaak recidieven tweede keus: alleen po selectie VRE Duur vaak recidieven Ernstige colitis vancomycin Snapshot of current treatments for initial episodes of CDI in Europe Treatments used in an initial episode of CDI in a recent European survey 0.2% 18% Oral metronidazole IV metronidazole 11% Oral vancomycin Intracolonic vancomycin 71% Bauer et al. Lancet 2011;377:63–73. Cure rates: Metronidazole & vancomycin p=0.36 p=0.02 39/40 p=0.006 69/71 30/31 37/41 66/79 28/38 *Patients were stratified by mild or severe disease based on severity assessment score developed for this study. Patients received one point each for age >60 years, temperature >38.3°C, albumin level <2.5 mg/dL, or peripheral white blood cell count >15,000 cells/mm3 within 48 hours of enrolment. Two points were given for endoscopic evidence of pseudomembranous colitis or treatment in an intensive care unit. Patients with ≥2 points were considered to have severe CDI. Zar et al. Clin Infect Dis 2007;45:302–7. Recurrence of CDI • Recurrence of CDI has been identified by ESCMID as the most important problem in the treatment of CDI1 • CDI recurrence is common, occurring in up to 32% of cases within 30 days following treatment2–4 • Rate of reported recurrences strongly depends on definition applied1 • Recurrence appears to be related to a combination of:5 – A failure to re-establish the colonic microflora – The presence in the intestines of spores of C. difficile – A sub-optimal host immune response to the infecting organism and its toxins 1. 2. 3. 4. 5. Bauer et al. Clin Microbiol Infect 2009;15:1067–79; Louie et al. N Engl J Med 2011;364:422–31; Lowy et al. N Engl J Med 2010;362:197–205; Bouza et al. Clin Microbiol Infect 2008;14:S103–4; DuPont. N Engl J Med 2011;364:473–4. Risk factors for a recurrence of CDI • Immunocompromised patients1 • Exposure to other antibacterial agents that disrupt the normal colonic microflora2–5 • Previous episode of CDI2,4–6 • Renal impairment7,8 • Aged 65 years or over2,4,9 • Impaired immune response to C. difficile toxin A2 • Severe underlying disease2 • Prolonged hospitalisation9 • Concomitant use of antacid medications (PPI)10 PPI, proton pump inhibitor • Intensive care unit (ICU) stay5 1. 2. 3. 4. 5. Cohen. J Ped Gastroenterol Nutr 2009;48:63–5; Kyne et al. Lancet 2001;357:189–93; Bauer et al. Clin Microbiol Infect 2009;15:1067–79; Bauer et al. Lancet 2011;377:63–73; Hu et al. Gastroenterology 2009;136:1206–14; 6. McFarland et al. Am J Gastroenterol 2002;97:1769–75; 7. Do et al. Clin Infect Dis 1998;26:954–9; 8. Bauer et al. Clin Microbiol Infect 2011;17(Suppl 4):A1–A4; 9. Pépin et al. Clin Infect Dis 2005;40:1591–7; 10. Kwok et al. Am J Gastroenterol 2012;107:1011–9. Pharmacotherapy of CDI: First recurrence • ESCMID recommends treating a first recurrence as a first episode unless the disease has progressed from non-severe to severe Diagnosis ESCMID recommended treatment Non-severe first recurrence Severe first recurrence Metronidazole 500 mg tid orally for 10 days* Vancomycin 125 mg qid orally for 10 days IV metronidazole 500 mg tid for 10 days plus intracolonic vancomycin 500 mg in 100 mL saline every 4–12 hours and/or vancomycin 500 mg qid by nasogastric tube if oral therapy impossible *Intravenous (IV ) if oral therapy is not possible; tid, three times daily; qid, four times daily Bauer et al. Clin Microbiol Infect 2009;15:1067–79. ESCMID recommendations: Second and later recurrences • ESCMID recommends treating second or later recurrences in the same way as severe first recurrence – With the option of using tapered or pulsed dosing regimens Diagnosis Second and later recurrences ESCMID recommended treatment Vancomycin 125 mg qid orally for at least 10 days Consider tapering vancomycin dose by decreasing daily dose with 125 mg every 3 days Consider pulse dosing with vancomycin 125 mg every 3 days for 3 weeks IV metronidazole 500 mg tid for 10–14 days plus retention enema of vancomycin 500 mg in 100 mL saline every 4–12 hours and/or vancomycin 500 mg qid by nasogastric tube if oral therapy impossible Bauer et al. Clin Microbiol Infect 2009;15:1067–79. NTVG 2005; 149: 2081 ESCMID recommendations: Surgical intervention • In the minority (<5%) of patients who develop fulminant colitis, surgical intervention (colectomy) may be needed • Surgical intervention carries a high rate of mortality • Optimal timing for colectomy has not been established • Current guidelines recommend intervention before: – The disease becomes too severe – Serum lactate levels exceed 5 mmol/L Bauer et al. Clin Microbiol Infect 2009;15:1067–79. Clinical limitations associated with current treatments for CDI • Although metronidazole and vancomycin are effective in a first episode of CDI, therapy remains suboptimal • Among the most significant drawbacks of current therapy for CDI are: – Rates of treatment failure with metronidazole of up to 18%1 – Rates of recurrent infection following treatment with metronidazole and vancomycin of up to 32% within 30 days following treatment2–4 – Risk of overgrowth of vancomycin-resistant enterococci (VRE) in patients who are already colonised with VRE5 1. Aslam et al. Lancet Infect Dis 2005;5:549–57; 2. Louie et al. N Engl J Med 2011;364:422–31; 3. Lowy et al. N Engl J Med 2010;362:197–205; 4. Bouza et al. Clin Microbiol Infect 2008;14:S103–4; 5. Al-Nassir et al. Antimicrob Agents Chemother 2008;52:2403–6. Fidaxomicine • • • • • • • • • Macrocyclisch antibioticum Remt bacteriële RNA polymerase Smal spectrum; Gram negatieve bacteriën resistent Remt sporenvorming Remt toxine productie Wordt beperkt geresorbeerd: lokaal werkzaam Zwangerschap / lactatie: onbekend Bijwerkingen: misselijkheid, braken, obstipatie... Dosering 2 dd 200mg 10 dagen Fidaxomicine • Extramuraal vergoed via GVS mits 18 jaar of ouder CDI Recidief na metronidazol behandeling Ernstige infectie • 1620 euro per kuur DJB: alternatieve therapie