Progress in diagnosing and treating Clostridia difficile in IBD patients

Progress in Diagnosing and Treating
Clostridium difficile in IBD patients
Alan C. Moss
MD, FEBG, FACG, AGAF
Associate Professor of Medicine
Director of Translational Research
Disclosures
• Consultant; Janssen, Theravance, Bayer, Roche
• Research Support; Pfizer, NIDDK, Salix, Shire
Case - 58 yr. old male patient
• Extensive ulcerative colitis since 2005
• in remission on mesalamine 2.4g/day
• August 2014 – Diverticulitis
• Rx antibiotics for 10 days
• “Flare-up” of colitis; increased mesalamine to 4.8g/d
• Stool negative for C.difficile
• Persistent diarrhea, abdominal cramps
• Rx prednisone 30mg
• PCR test comes back “positive” for
C.difficile
• Rx Metronidazole
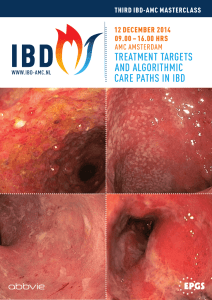
Case - Sigmoidoscopy
Day 5 of metronidazole;
•
Still having 4-6 stool /day, cramps
Clinical Dilemmas with C. difficile Infection (CDI) in
IBD
C. difficile PCR test results in patients with IBD
Which antibiotic to use in IBD?
Should I stop the immunosuppressants?
Are fecal transplants safe in treating recurrent C. difficile in patients with IBD?
C.difficile
Testing in IBD
Conundrum of C.difficile infection (CDI) in IBD
Diarrhea
Abdominal pain
Altered microbiome
Elevated calprotectin
Endoscopic lesions
Active IBD 7%
C.difficile
Infection
Diarrhea
Abdominal pain
Altered microbiome
Elevated calprotectin
Endoscopic lesions
Regnault H, Dig Liver Dis. 2014 Oct 4. pii: S1590-8658
Martinelli M, Inflamm Bowel Dis. 2014 Dec;20(12):2219-25
Clinical Specificity of PCR Testing
• Positive predictive value of PCR test for C.diff
.;
• PPV 42-98% - versus toxigenic culture
• ‘clinical’ specificity unclear – colonization vs. infection
• PCR detects <10 pg of genomic DNA
• Switch from EIA to PCR testing – doubling of “+” results
• Prevalence of C.diff
in 2,500 in-patients with IBD;
•
4%+ EIA, 5%+ PCR (9%+ EIA, 13%+ PCR in non-IBD)
Burnham C, Clin Microbiol Rev. 2013 Jul;26(3):604-30
Shakir F, Gastroenterol Hepatol (N Y). 2012 May;8(5):313-7
Deshpande A, Curr Med Res Opin. 2012 Sep;28(9):1553-60
ELISA in PCR+ Stool Samples in IBD
• ? PCR+ / ELISA - samples = colonizers
Lamouse-Smith, J Pediatr Gastroenterol Nutr. 2013 Sep;57(3):293-7
C.difficile
Infection Treatment in IBD
Antibiotics for Severe C.diff Infection in IBD
• 114 hospitalized patients with IBD
• 20 UC patients with severe CDI
• 65% got vancomycin with / or after metronidazole
• Not controlled for UC severity
Horton A, Antimicrob Agents Chemother. 2014 Sep;58(9):5054-9
Khanna R, Inflamm Bowel Dis. 2013 Sep;19(10):2223-6
Suggested Approach to C.difficile Infection (CDI) in IBD
Determine Disease & Infection Severity*
Non-severe disease
Severe disease
Vancomycin 125mg QID
‘Complicated’ disease
Recurrent infection
•
Vancomycin with taper
• Fecal transplant
•
Rifaximin / Fidoxamicin
Metronidazole for first infection
Vancomycin 500mg QID
Issa M, Clin Gastroenterol Hepatol. 2007 Mar;5(3):345-51.
Ananthakrishnan, A, Alim Pharm Ther 2012; 35 (7): 789-795
Horton A, Antimicrob Agents Chemother. 2014 Sep;58(9):5054-9
Khanna R, Inflamm Bowel Dis. 2013 Sep;19(10):2223-6
What is ‘Severe’ CDI with IBD?*
‘Severe’ IBD with CDI
• Serum albumin < 3 g/dL
• Haemoglobin < 9 g/dL
• Serum creatinine >1.5 mg/dL
• 3-9 fold greater risk of colectomy or death
‘Severe’ CDI
• WBC count of >15,000 cells/mm
• Age >60 years
• Temperature > 100.9 F
• Albumin <2.5 mg/dl
• Pseudomembranes
• ICU admission
Zar F, Clin. Infect. Dis. 45:302 –307. doi:10.1086/519265
Ananthakrishnan, A, Alim Pharm Ther 2012; 35 (7): 789-795
Could a sigmoidoscopy help?
Only 13% of patients with CDI and IBD have pseudomembranes
Ben-Horin SJ Crohns Colitis. 2010 Jun;4(2):194-8
Stop or Increase Immunosuppressants during IBD Flares with CDI?
Escalate or Stop IBD Treatment in CDI?
• IBD experts divided on what to do!
• ECCO retrospective study;
• 155 hospitalized patients with IBD and CDI
• 77% Rx metronidazole
• Risk factors for death, colectomy, megacolon, shock;
>2 immunosuppressants during therapy
Albumin <2.5mg/dl
Ben-Horin S Inflamm Bowel Dis. 2011 Jul;17(7):1540-6
Ben-Horin S, Clin Gastroenterol Hepatol. 2009 Sep;7(9):981-7
Case – Follow-Up
• Metronidazole changed to Vancomycin
• Albumin 2.1, age >60, CRP 58
• Still 4-6BM /day, blood
• Infliximab 10mg/kg infusion
• 2-4 BM /day, no blood
• CRP 10
• Discharged on vancomycin taper
• In remission in office 2 weeks later