By: Cindy Stegman RN BSN
Alverno College MSN 621
Spring 2010
stegmacm@alverno.edu
How to navigate this tutorial:
To advance to next slide click on
box
To advance to previous slide click on
To return to MAIN MENU click on
If you see the return button
QUESTION slide.
box
click on it to return to
Hover over the underlined text for an
explanation/definition
box
PURPOSE & OUTCOMES
To educate RNs and LPNs on the pathophysiology of
advanced lung cancer associated with dyspnea
At the end of the tutorial the learner will be able to:
• Identify pathophysiology of advanced lung cancer associated with
dyspnea
• Discuss key assessment components of the advanced lung cancer
patients experiencing dyspnea
• Describe evidence-based interventions for the advanced lung cancer
patients experiencing dyspnea
Content of Tutorial
At any time during tutorial you may click
to come to this screen and select next topic.
Let’s get started… taking a DEEP breath and relax!
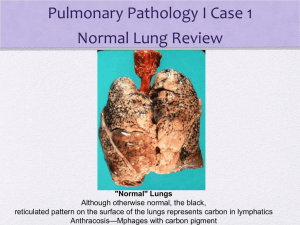
Anatomy of normal lung function
Pathophysiology of advanced lung cancer
Genetic relationship
Mechanisms of dyspnea
Causes of dyspnea
Stress & Immune/Inflammatory
response
Nursing assessment
Evidence-Based Nursing Interventions
Nursing-Sensitive Outcomes
Case Study
Clip art, 2010
Anatomy of
Normal Lung Function
Click each circle in the
diagram to recognize the
anatomy of the lungs
Trachea: Is the tube that runs from
your larynx to just above your lungs.
The trachea divides into TWO large
branches called the bronchi.
1
Bronchi: Entering the lung, the
bronchi divide into the left and right
side of lung. They continue to
branch & divide into smaller
bronchi.
2
Bronchioles: Smallest conducting
airways at the terminal end of the
bronchi. At the most distal end gas
exchange takes place.
4
Pleura: A thin serous membrane
that lines the thoracic cavity &
cushions the lungs.
3
5
Porth, 2005
Alveolar sacs: Cup-shaped
structures which are the smallest
functional unit of the lungs.
Physiology of Normal Breathing:
-Automatic, quiet
- Movement that control ventilation are integrated by neurons located in:
- Medulla & Pons (Respiratory Center)
GOAL of Breathing: Oxygenation of the blood and removal of
Carbon dioxide.
Scroll across each picture
Porth, 2005)
What Stimulates your
respiratory
system to increase
breathing?
Click on star to
receive answer
Receptors
1)Chemoreceptors
- Peripheral chemoreceptors:
Located in the carotid and
aortic bodies
- Central chemoreceptors: Located in the Respiratory
center in the Medulla & pons
2) Lung & Chest wall Receptors
-
Stretch (smooth muscle)
- Irritant (Airway of epithelial cells)
- Juxtacapillary
Jantarakupt, P. & Porock, D. (2005).
or J receptors (alveolar wall)
A nurse walks into a room and observes a patient
breathing rapid and shallow. Respiratory rate
is 32 breaths/min and pulse ox at 80% on room
air. What receptors alerted the
respiratory center to turn ON ?
Incorrect.
These receptors are located in
the medulla & pons and
stimulate the resp. center when
there are high levels of carbon
dioxide in the blood.
Central
Chemoreceptors
Incorrect
In this situation because this
scenario did not mention
J Receptors
crackles
in the lungs that
would suggest pulmonary
edema.
Incorrect.
These receptors are located in
smooth Stretch
muscle and do not
stimulate the respiratory center
Receptors
when there is LOW oxygen in
the blood.
Correct!!
Peripheral
These
receptors alert the
respiratory center when there
Chemoreceptors
is LOW oxygen in the blood
What Causes Lung Cancer?
Repeated
EXPOSURE to
Carcinogens
Transforms:
Normal cell
into
Malignant
Genetic Damage
Cells in the respiratory
membrane that line the
bronchi become
THICK &
HARDEN
Clip
Art, 2010
Hoffman,
A.
& Gift, A. (2007)
Cilia
become
Stiff (Unable to sweep
debris away)
Lung Cancer Cell Dividing
Permission from http://images.wellcome.ac.uk/
- Lung cancer cells are highly invasive & may extend into the mediastinum or pleural cavity
- Lung network is highly vascular and metastasis occurs early
- Distant metastasis may occur in the brain, liver, bones, or kidneys
Hoffman, A., & Gift, A. (2007)
What we know increases risk for
development of Lung Cancer
• Active tobacco exposure
• Passive smoke exposure (Second hand)
• Shared environment
• Asbestos (school, home, work, person-person)
Clip Art, 2007
• Environmental exposure (Radon & heavy metals)
• Nickel, arsenic
National Cancer Institute, 2010
Clip Art, 2007
Clip Art, 2007
Clip Art, 2010
Research in the works…
Study produced by:
•National Cancer Institute
•National Human Genome Research Institute
•National Institutes of health
Study involved:
-52 families with a minimum of Three 1st-degree family members
affected by either lung, throat, or laryngeal cancer
-Used 392 known genetic markers & compared the alleles of each
affected and non-affected family member
National Cancer Institute, 2010
Study that was printed in 2004 in the
American Journal of Human Genetics
Research in the works Cont…
Discovered:
A region on Chromosome 6
(susceptibility to Lung caner)
WORK is needed to:
Look closer in this REGION
to find the exact
GENE that causes
this susceptibility
National Cancer Institute, 2010
Clip Art, 2010
Mechanisms of
Dyspnea
•Divided into 3 pathologies:
• Chemical Stimulation
• Neural Stimulation
• Emotional Stimulation
Clip Art, 2007
Chemical Stimulation
Central
respiratory
chemoreceptors
PaCO2
Clip Art, 2007
Eliminate
Carbon
Dioxide
Peripheral
respiratory
chemoreceptors
PaO2
Clip Art, 2007
Jantarakupt, P. & Porock, D. (2005)
American Thoracic Society. (1998).
Neural Stimulation
Neural Pathways for breathing receive signals from receptors in:
- Lungs
- Skin
- Muscles
- Joints
These receptors are called “Mechanoreceptors”
Once
mechanoreceptors are
stimulated they will
cause an individual to
breathe faster
- Stretch receptors in (trachea, bronchi) are stimulated with lung expansion
- Irritant receptors (epithelium of airways) stimulated by smoke,
pollens, fungi, cold air, & mold
- Movement of lower and upper extremities stimulate receptors in muscles &
joints
- Painful stimuli will elicit mechanoreceptors within the skin
Jantarakupt, P. & Porock, D. (2005)
Emotional Stimulation
• Emotional distress
• Anxiety
• Anger
• Depression
THE CAUSE & EFFECT relationship is unclear but…
Clip art, 2007
Emotional changes CAN stimulate the
respiratory center, which in turn AFFECTS the
Individual’s breathing pattern
Jantarakupt, P. & Porock, D. (2005).
Dyspnea is a distressing and
debilitating symptom that cancer
patients may experience.
- It is SUBJECTIVE (what the patient says)
- An uncomfortable, frightening experience
Dyspnea is estimated to occur
in 15-55% at the time of diagnosis
and up to 18-79% during the
last week of life
Oncology Nursing Society. (2010).
Clip art, 2007
(
Stress and Dyspnea:
What’s the CONNECTION?
Stress response or General
Adaptation Syndrome (GAS) is
meant to protect an individual
during ACUTE episodes stress. If
the GAS is continually stimulated
by chronic stressors,
this can be a threat to an
individual’s homeostasis.
Clip Art, 2010
Porth, C., (2005)
Stress and DYSPNEA Cont…
Dyspnea: Acute or Chronic
ALERT:
STRESS
RESPONSE
Advanced Lung Cancer
PATIENT
Physical &
Psychological Stress
Stress and Dyspnea Cont…
Results:
In release of catecholamines (such as epinephrine and
norepinephrine) and cortisol, which:
- Increases heart rate
- Dilates the bronchioles
Stress causes Vasoconstriction to…
- Skin: which becomes Pallor and cold
- GI tract: which causes nausea, No bowel sounds, & digestion stops
- Kidneys: which decreases urinary output
Inflammatory and Immune
response stops!
Porth, C., (2005))
Endocrine-Neurotransmitter pathway… PRODUCE
Physical
Behavioral
CHANGES
ADAPT
to
ACUTE
STRESS
WHAT factors AFFECT our ability to ADAPT
to STRESS??
Sleep-Wake
Cycles
Sleep is the
most restorative
function in
which tissues
are regenerated.
If an individual
cannot sleep at
night, due to
dyspnea, this is
affecting their
ability to restore
their energy.
Porth, C. (2005)
Nutrition
Mental
Health
Status
Severe emotional
distress often disrupts
physiological function
and limits an
individuals ability to
make appropriate
choices related to
adaptive needs. If a
dyspnea is present, this
is causing emotional
distress and affecting
their ability to enjoy
daily activities due to
the stress of not being
able to breathe.
Malnutrition is one of
Click
each circle
the moston
common
causes of
immunodeficiency.
Most advanced lung
cancer patients have
major issues with
nutrition due to loss of
appetite & weight loss
from treatment &/or
disease process itself.
Hardiness
A personality
characteristic which
includes: A sense of
purpose in life and to
view stressors as a
challenge rather
than a threat. If
dyspnea is affecting
their hardiness, the
individual will see
this stressor as a
threat and slowly
become susceptible
to sadness.
What happens if
DYSPNEA
continues to stimulate
our
Stress Response??
Exhaustion OCCURS!
Coping mechanisms
are depleted.
WEAR & TEAR on
the System
Chronic stress will occur & LEAD to:
Loss of Appetite
Sleep disturbance
Depression
Clip Art, 2007
Porth, C., 2005
What does this mean for an
advanced lung cancer
patient if this cycle
continues ?
Immune & Inflammatory
responses diminish
which means:
The advanced lung cancer patient is at an
increased risk for infections
Clip Art, 2007
The AGING advanced
lung cancer patient has
less ability to adapt to
environmental stressors
Porth, C., 2005
Decreases their
immune
responsiveness
&
ability
to heal wounds
If the GAS is constantly stimulated,
what does this mean for the
aged advanced lung cancer patient?
Aging can be viewed as a low-grade chronic
inflammatory state which is termed as
“inflammaging”
Due to the thymus
decreasing in size as we
age , this affects T-Cell
function within the
body. Ultimately,
compromises the
immune system
responsiveness to heal
wounds.
Porth, C. 2005 & Franceschi, C. & Bonafe, M. 2003
Click on ARROW
twice
Due to inflammaging,
this can cause chronic
activation of
inflammatory responses.
Eventually, leads to the
infiltration of
macrophages,
lymphocytes, &
fibroblasts, which causes
persistent swelling and
scar formation to occur.
Cancer-Related Causes
of DYSPNEA:
1)Direct cause of the cancer
2)Indirect result of the cancer
3)Result of cancer treatment
4) Other
DIRECT
-Primary or metastatic cancer to lung
- Pleural tumor
Permission from http://images.wellcome.ac.uk/
- Pericardial effusion
- Ascites
INDIRECT
-Anemia
-Pneumonia
- Pulmonary emboli
- Cachexia
Tyson, L. (2006)
Dyspnea from Treatment
1) Surgery
2) Radiation (which can cause)
- - Pulmonary Pneumonitis
- - Pulmonary fibrosis
3) Chemotherapy agents that can either cause:
-
Pulmonary Edema
Cytoxan, Gemzar, Methotrexate, Mitomycin
-
Pulmonary Pneumonitis/Fibrosis
Cytoxan (later development), Gemzar (later sign of fibrosis),
Bleomycin (Pneumonitis), Methotrexate, Carmustine
Polovich, M., Whitford, J., & Olsen, M. (2009).
Clip Art, 2007
Co-Morbidities that cause
Dysnpea
- Obesity
- Age
- Asthma
- CHF or COPD
Other:
- Anxiety
Clip art, 2007
DiSalvo, W., at el., (2008)
Oncology Nursing Society (ONS)
In 2003, ONS developed their own definition of
oncology nursing-sensitive patient outcomes
(NSPO’s), which focused around:
-Patient’s problems are significantly affected by nursing interventions.
-Interventions developed within the scope of nursing practice; are sensitive
to nursing care and represent the consequences or effects of nursing
interventions
-Result in changes in patients' symptom experience, functional status,
safety, psychological distress, and/or cost
Oncology Nursing Society, 2003
NSPO’s for
Dyspnea:
1) Symptom Management
-
Decrease in patient’s perception of breathlessness
Patient maintains activity level within capabilities
Respiratory rate remains at comfortable level
Patient is able to manage episodes of dyspnea
2) Psychosocial Distress
- Promoting relaxation and stress reduction
- Education and support to patients and their families
Crowley. (2005) & ONS PEP, (2008)
ASSESSMENT
1) SUBJECTIVE (Pt’s own description, feeling, of breathlessness)
- At rest
- With activity
- Assess dyspnea with a Visual Analog scale
- Number Scale (1-10)
- Mild-Moderate-Severe
2) VITAL SIGNS
- Respiratory rate (Rate, Irregular, Depth)
- Weight
Clip Art, 2007
Clip Art, 2007
Assessment Cont…
3) CARDIOPULMONARY:
- Accessory Muscle use
- Edema
- Tachycardia
- Underlying cause (fever, etc.)
- Auscultation
Clip Art, 2007
-Wheezes, crackles, cough
- Secretions (amount, consistency)
4) INTEGUMENTARY:
- Pallor (Anemia)
- Cyanosis (Low oxygen, hypoxia)
Itano, J. & Taoka, K. (2005)
Assessment Cont…
5) MENTAL STATUS
- Restlessness
- Confusion
- Memory Difficulties
6) PSYCHOSOCIAL Distress:
- Depression
- Anxiety
- Fear
Clip art, 2007
G. S. is a 65 year-old man diagnosed with Stage IV
Lung cancer in October 2009
- His presenting symptom at the time of diagnosis is rib pain.
- During the next few weeks, G.S has received several radiation treatments to his ribs.
- After his radiation treatment, G.S has also received system chemotherapy.
(Up to this point, G.S. has tolerated this treatment fairly well)
December of 2009 (post radiation/chemotherapy tx) G.S had a PET scan that
showing worsening enlargement of primary tumor.
January 2010 G.S. was switched to salvage Taxotere chemotherapy regimen
Over the next few weeks to months G.S. is seen in the clinic with increased
weakness, hypotension, nausea, and dehydration.
Continued
Today March 2010, G.S is seen in the clinic:
- G.S. is looking frail & ashen in color
- Knees down bilateral has +3 pitting edema
- Oxygen saturation measuring at 87% on room air
- No appetite
- Lost of five pounds since February
- Denies any pain
- C/o of shortness of breath with activity
- Uses a walker to assist with ambulation
- C/O of insomnia, due to trouble breathing at night
- On auscultation: fine wheezes heard throughout bases of lungs
HOME MEDICATION:
- MS Contin 30 mg BID
- Fluconazole 200 mg
- Ativan 0.5-1 mg every 8 hrs PRN
- Oxycodone 5 mg (1-3) every 2 hrs PRN
These are all possible Nursing Interventions to help
relieve G.S’s DYSPNEA.
Click on all the buttons at the bottom to understand WHY?
A) Suggest to G.S to get a prescription of Morphine Sulfate in an immediate release
capsules to help relieve his dyspnea
B) On assessment, heard audible wheezes in upper lung fields. Suggest an albuterol inhaler treatment
C) Suggest to G.S to take his Ativan before strenuous activities & before sleep to help relieve his anxiety
D) G.S. oxygen saturation on room air was 87%. Supplement oxygen to help relieve his dyspnea.
E) Due to the edema (swelling) in his legs, ask his physician for an order of lasix
F) Suggest to his wife to place a fan on G.S’s face and nose, as this might help relieve his dyspnea or use
breathing techniques to slow down his breathing during periods of dyspnea.
G) Educate G.S on relaxation techniques & encourage G.S to sleep in his recliner to keep upper body
at least at 45-90 degree angel to help with sleep.
A
B
C
D
E
F
G
Opioids
on Cancer-Related
Dyspnea
•
Immediate-release oral agents
• Parenteral
RECOMMENDED for Practice:
WHEN
OXYGEN
OR REST
DO NOT
RELIEVE
DYSPNEA
• Morphine (most common)
• Hydromorphone (Dilaudid)
NCCN, 2010, DiSalvo, W., Joyce, M., Tyson, L., Culkin, A., & Mackay, K., 2008, & Oncology Nursing Society, 2008.
Theory of OPIATES
Opioids have a depressant effect on the central nervous
system, which alleviate dyspnea by blocking the neural
signals to hypoxia & hypercapnia.
MORPHINE
Act at
central/peripheral
opioid receptors
sites &
central nervous
system
(Respiratory
center)
Wickham, R. (2002) & Gift, A. & Hoffman, A. (2007)
Respiratory
drive at
rest and
activity
Block
respiratory
responses to
hypoxia
&
hypercapnia
Recommendations:
Treating COUGH/DYSPNEA/ or AIR HUNGER
- 2-10 mg Morphine orally every 4 hr prn
- 1-4 mg Morphine IV every 4 hr prn
NCCN, 2010
REMEMBER!!
Naïve
Vs
Tolerant
1) RE-ASSESS patient
2) SIDE EFFECTS: dysphoria, dizziness, drowsiness,
urinary retention, constipation.
Re-assure patient:
Opiates will help them rest without the feeling of “suffocation”
Jantarakupt, P. & Porock, D. (2005), NCCN, 2010, & Wickham, R. (2002).
LOWER dose
of Morphine
used to treat
Dyspnea,
BUT
Action of
Morphine for
dyspnea is
shorter than
its analgesic
effects!
Patient/Family MYTHS & FEARS
about OPIOIDs
1) ADDICTION
- Reassure patient they are taking opioids to relieve their
cancer-related dyspnea. Dyspnea can change from day to day
depending on the progression of their disease state. As nurse
providers, reassure patient that the dosage may increase in the
future due to repeated administration of that opioid dose. The
body will eventually build up a tolerance for that dose of opioids and
the individual will not be receiving the desired effect.
Clip Art, 2010
2) Over SEDATION
- Reassure patient we will be monitoring them while receiving opioids
- This is for palliative treatment of dyspnea, so titrating the opioid dosage may be
necessary to get the desired effect.
Sleep & a comatose
- As the individual transitions from palliative care to hospice…
state to occur with the
DYING
patient’s
breathing is
now more rapid
& shallow
Wickham, R. (2002) & Johnston, M. (2007).
Retain
increased
amounts of
carbon
dioxide
Causes
dying patient
regardless if opioids
are administered or
not
QUIZ
1) Are extended-release opioids just as effective as
immediate-release?
CORRECT!
Immediate-release opioids have
been shown to be effective in
practice when treating dyspnea.
TRUE
Sorry
Extended-Release opioids have
NOT been established to show
effectiveness towards treating
dyspnea
FALSE
In the case of G.S, immediate-release opioids are an appropriate intervention,
because he has already has been exposed to opioids. REMEMBER… he is opioid
tolerant, so G.S. might need to repeat the dose more frequently to treat the
DYSPNEA. As nurse providers, we need to console & support G.S. if he has any
fears of using opiods, because sedation & addiction can be a fear patients have with opioid
usage. KEEP the patient’s GOAL in mind & reassure G.S. that this intervention
will be able to get him through tough periods of dyspnea to be able to endure certain
activities.
Bronchodilators
Bronchodilators relaxes
smooth muscles within the
bronchioles
•Inhaled or Nebulized
-B2 –adrengergic agonist
decreases
WORKLOAD of the lungs
• Albuterol
Nebulized Opioids??
Believed to
“TARGET”
stretch and
irritant receptors
in the lungs
Jantarakupt, P. & Porock, D. (2005) & Kallet, R., (2007)
SYSTEMIC
TOXICITY
NOT
Recommend for
Practice Due to:
Insufficient
Evidence
Quiz
1) Which option is correct to suggest an albuterol
inhaler to treat G.S’s dyspnea?
Sorry
G.S complained
ofmore
Short-Acting
bronchodilators are
effective
for patient’s
have either
shortness
ofwhobreath
air flow obstruction such as COPD,
while
walking
tocancer
the &
asthma,
or patient’s
with lung
is presenting with wheezing throughout
bathroom?
lung fields to suggest vasoconstriction.
Wickham, R. 2005
CORRECT
OnOnauscultation,
you
assessment you heard
wheezing
throughout
lung fields to
heard
wheezes
suggest vasoconstriction within
throughout
G.S.’s
lung
bronchioles. An
albuterol
treatment would
fields
be an appropriate
intervention for G.S’s dyspnea.
Benzodiazepines
DO NOT
WORK
DIRECTLY
ON THE
LUNGS
•Lorazepam
• Diazepam
Recommended Dosages:
Ativan: 0.5-1 mg orally or IV q 4 hrs prn
Diazepam: 2 mg po/SQ/IV q 12 hours (NCCN, 2010)
Sedative action
ANXIETY that stimulates dyspnea!!
Jantarakupt, P., & Porock, D., (2005) & NCCN, (2010). & Wickham, R., (2002)
Quiz
True or False:
Do benzodiazepines work directly on the lungs to relieve
Dyspnea?
Sorry
Benzodiazepines do
not directly work on
the lungs to relieve
dyspnea.
Benzodiazepines are
used for their sedative
use to decrease anxiety
that is commonly
associated with
dyspnea.
TRUE
YES
Benzodiazepines treat
anxiety associated
with dyspnea and do
not directly treat
dyspnea. In G.S’s case,
this can help his
anxiety & let him be
able to sleep at night
with out the fear of
suffocation.
FALSE
OXYGEN
- Increase oxygen saturation (SaO2)
- Hypoxia is present
DYSPNEA
• Lowers respiratory RATE
• Lowers respiratory EFFORT
Non-hypoxic Patients?
FEAR and Anxiety
Jantaarakupt, P. & Porock, D. (2005)
Clip Art, 2007
Click on box
Patient’s with advanced lung cancer have less
ability to remove carbon dioxide or transport
oxygen to other parts of the body due to the
physical changes cancer makes within lung tissue.
Patient’s with a history of COPD will be at higher
risk of retaining CO2.
CAUTION!!
CO2 Retainers
Quiz
True or False
Oxygen therapy is ONLY for patient’s who are truly hypoxic?
Incorrect
Oxygen therapy is
primarily used for hypoxic
patients, but in cases of
advanced lung cancer
patient’s who are
experiencing dyspnea,
oxygen has been proven to
help relieve the feeling of
shortness of breath.
True
Correct
Oxygen therapy can be used
for hypoxic & non-hypoxic
advanced lung cancer patient’s
experiencing dyspnea.
CAUTION should be used
when titrating oxygen if
patient is a CO2 retainer. In
the case of G.S. he is truly
hypoxic when his oxygen
saturation was at 87% on room
air. Oxygen therapy would be
an appropriate intervention to
treat his dyspnea.
False
OTHER Treatments:
Steroids & NSAIDS
INFLAMMATION in the LUNGS to
relieve dyspnea
More effective for patient’s with pre-existing conditions such as COPD
Side effects of steroids: Gastric toxicity, fluid retention, hyperglycemia
Lasix
Given when a patient is experiencing:
1) Pulmonary congestion
2) Lower extremity edema
LASIX is given for fluid
overload to
Decrease the demand
on the heart
Jantarakupt, P. & Porock, D., 2005 & Wickham, R. 2005
Gift A. & Hoffman, A. (2007).
What is the relationship between
G.S’s lower extremity edema and
him experiencing DYSPNEA?
In G.S.’s situation, there could be multiple factors
causing his lower leg edema, such as malnutrition,
medications, and/or worsening of his lung cancer
involvement . The edema is causing his heart to
pump harder to compensate for the extra fluid, which
is causing G.S. to have dyspnea at rest &/or with
activities. Lasix would be an appropriate short term fix
to help with the edema in lower extremities & relieve
dyspnea.
CLICK ON
Hoffman, A. & Gift, A. (2007)
1)Breathing Techniques
- Pursed-lip and diaphragmatic breathing
(Shown to optimize lung function, decrease stress, & relax
the breathing for that patient)
2) Increase airflow (generated
- Face
- Nose
by a FAN)
(Gives the perception of more airflow to the individual, which
may reduce the feeling of dyspnea)
3) Providing COOLER temperatures
- Decrease the feeling of dyspnea
DiSalvo, W., Joyce, M., & Belansky, H. (2009)
Clip Art, 2007
Clip Art, 2007
4) Positioning
- Sitting up (expansion of lungs)
5) Promoting Relaxation
Stress Reduction
- Massage
- Reducing external noise
(Decrease anxiety & stress associated with dyspnea)
6) Emotional & Psychosocial
Support
(Coaching and support have been shown to decrease the
feeling and anxiety associated with dyspnea)
Andry, J. (2008) & Tyson, L (2006)
Clip Art, 2007
Key Points to REMEMBER:
-Dyspnea is a SUBJECTIVE feeling & a debilitating symptom that patients
experience.
- Key ASSESSMENT skills are crucial to help understand the underline cause of the
dyspnea and/or the treatment options.
-Be consciously aware of evidence-based interventions that are already
incorporated into nursing practice, whether the dyspnea is oncology related or not.
-Dyspnea is a symptom that can CHANGE from day to day. Reassure the patient
of this and the multiple interventions we can help to relieve dyspnea.
KEY POINTS
TO
REMEMBER
-Lastly, keep the patient’s GOAL in mind. Are the interventions appropriate and
will the patient be able to enjoy certain activities with some of the side effects
that may occur. Just remember to communicate & educate patients on these
interventions and just maybe, we can give them a little relief from their dyspnea!
REFERENCES:
About.Com. (2010). Smoking Cessation. Retrieved April 5, 2010 from, http://quitsmoking.about.com/cs/nicotinepatch/g/carcinogen.htm
American Cancer Society. (2007). Retrieved February 23, 2010 from, http://www.cancer.org/downloads/PRO/LungCancer.pdf
American Thoracic Society. (1998). Dysnpea: Mechanisms, Assessment, & Management. A Consensus Statement. American Journal of Respiratory and Critical
Care Medicine. (159) pp 321-340.
Andry, J. (2008). Palliative Practices From A-Z for the Bedside Clinician. In Esper, P. & Kuebler, K. (Eds.). Dyspnea. (2nd ed., pp. 117-122). ONS Publishing
Division, PA: Pittsburgh.
Crowley, M. (2005). Core Curriculum for Oncology Nursing. In Itano, J. & Taoka, K (Eds.), Supportive Care: Dying and Death. (4th ed., pp. 102-126) St. Louis:
Elsevier Saunders
DiSalvo, W., Joyce, M., Tyson, L., Culkin, A., & Mackay, K. (2008). Putting Evidence Into Practice: Evidence-Based Interventions for Cancer-Related Dyspnea.
Clinical Journal of Oncology Nursing. 12(2) pp. 341-352.
Franceschi, C. & Bonafe, M. (2003). Centenarians as a model for healthy aging. Biochemical Society Transactions. 31(2) pp: 457-461.
Guyton, A. & Hall, J. (2006). Blood Cells, Immunity, & Blood Clotting. Schmitt, W. & Gruliow, R. Medical Physiology (11th e.d.) pp. 439-450. PA: Elsevier Inc
Hoffman, A. & Gift, A. (2007). Oncology Nursing. In Langhorne, M., Fulton, J., & Otto, S. Lung Cancer. (5th e.d., pp. 258- 274). St. Louis: Elsevier Saunders.
Jantarakupt, P. & Porock, D. (2005). Dyspnea Management in Lung Cancer: Applying the Evidence From Chronic Obstructive Pulmonary Disease. Oncology
Nursing Forum. 32(4), pp. 785-795.
Johnston, M. P. (2007). Oncology Nursing. In Langhorne, M., Fulton, J., & Otto, S. Pain. (5th e.d. pp. 680-693). St. Louis: Elsevier Saunders.
Kallet, R. (2007). The Role of Inhaled Opioids and Furosemide for the Treatment of Dyspnea. Respiratory Care. 52(7): pp. 900-910.
Nation Cancer Institute, Retrieved on March 31, 2o10 from, http://www.cancer.gov/newscenter/pressreleases/lungcancerlocus
National Comprehensive Cancer Network Practice Guidelines, Palliative Care, Version 1, 2010. Retrieved on April 22, 2010 from http://www.nccn.org
Oncology Nursing Society, 2003. Retrieved on March 31, 2010 from, http://www.ons.org/Research/NursingSensitive/
Oncology Nursing Society, 2008. Putting Evidence into Practice. Retrieved on April 2, 2010 from, http://www.ons.org/Research/PEP
Polovich, M., Whitford, J., & Olsen, M. (2009). Chemotherapy and Biotherapy Guidelines and Recommendations
234-244.
for Practice. Oncology Nursing Society, pp.
Stedman’s Medical Dictionary for the Health Professions and Nursing. (2005). (5th e.d.) Baltimore, MD: Lippincott Williams & Wilkins.
Tyson, L. (2006). Dyspnea. Clinical Manual for the Oncology Advanced Practice Nurse. Sorrell-Camp, D. & Hawkins, R. (23) pp. 153-158.
Wickham, R. (2002). Dyspnea: Recognizing and managing an invisible problem. Oncology Nursing Forum, 29, 925-933.
Zerwekh, J. & Claborn, J. (2006). Illustrated Study Guide for the NCLEX-RN Exam. Respiratory System, pp. 281-316. MO: Elsevier Mosby.