Approach to Respiratory Failure
advertisement

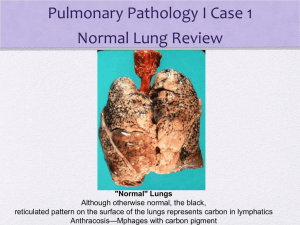
Approach to Dyspnea Mani S. Kavuru, MD Professor & Division Chief Pulmonary & Critical Care Medicine Thomas Jefferson University / Hospital Key learning Objectives • Familiarize with eliciting history relevant to dyspnea & scales utilized; • Be able to define a diagnostic approach to dyspnea, with emphasis in the outpatient area; • Develop facility with common pulmonary diagnostic modalities from PFTs, exercise studies, imaging, and biopsy • Apply these concepts in case-based scenarios ATS Definition of Dyspnea • Patient self-reported, subjective • “Breathing discomfort, qualitatively distinct sensations varying in intensity” • Arises from “interactions among multiple physiological, psychological, social, and environmental factors and may induce secondary psychological and behavioral responses” • Prefer “breathlessness” as patient-centric Dyspnea • Subjective • Discomfort associated with the act of breathing in circumstances it is unexpected; • Further characterize by: ◊nature of onset (acute, chronic), duration ◊evolution over time ◊associated symptoms (cough, CP, wheeze, orthopnea) ◊physiologic vs. pathologic ◊quantify (“no SOB” is inadequate) Caveats re. Dyspnea Evaluation • Note discrepancy between patient’s perception (under-reported) and physician’s clinical evaluation (under-recognized); • Be able to recognize fatigue vs. activity intolerance vs. dyspnea; • Be aware of natural history of dyspnea in various clinical settings and disease entities; • Co-existence of multiple causes of dyspnea is common; so need to be able to define relative contribution of lung disease (as opposed to obesity, anemia, LBP); • Be adept at distiguishing cardiac vs. pulmonary causes of SOB; • FEV1 as a surrogate marker can be misleading; • PFTs and exercise studies do not assess severity of feeling of breathlessness (a sensation); but rather impact on functional capacity or physiological consequences; • Don’t be fooled by “normal O2 sat’n”; Pathogenesis of Dyspnea • Dynamic hyperinflation • Increased ventilatory demand relative to capacity • Abnormalities in gas exchange • Inspiratory muscle weakness • Cognitive & psychological influences (i.e. fear, anxiety) • Other The “Oxygen Cost” Diagram “What can you do before you become short of breath?” Patient makes a mark on a 10cm line at the point beyond which they become breathless The oxygen cost diagram is more sensitive to change than the MRC scale - it consists of a 10cm line with everyday activities placed proportionately according to their oxygen cost. Patients place a mark on a 10cm line, beyond which they become Reference breathless. The ability score is the distance in centimetres from the zero point. McGavin CR, Artvinli M, Naoe H, McHardy GJR. Dyspnoea, disability and distance walked: comparison of estimates of exercise performance in respiratory disease. Br Med J 1978; 2: 241–243 Bausewein. Respiratory Med 2007 1. A 62 y/o WM smoker (200+ pk-yr) with progressive dyspnea and activity intolerance over past 6 mos; Exam: markedly reduced BSs with prolonged expiration, distant heart tones, 1+ edema; CXR is clear; spiro shows FEV1 to be 30%, FVC 50%, ratio 0.32; RA PaO2 is 78; 2. A 45 y/o with hx of pred-dependent asthma since childhood; is a smoker; has gained 100+ lbs; several prior admits for resp failure; now presents to clinic with worsened SOB, wheezing; Exam: verbal, no distress, audible wheezing, morbidly obese; RA O2 sat = 98%; 3. A 75 y/o non-smoker presents with Clinical Evaluation for Lung Disease • PFTs: spirometry (screening/simple), lung volumes, DLCO, O2 assessment; [assess for copd, asthma, UAO, ILD] • Exercise assessment (6MWT, GXT) [assess functional status of any cardiopulm disease] • Bronchoprovocation challenge [assess for asthma] • Serial chest radiographs, CTA / HRCT chest [assess for ILD, cancer, CHF, HP, other] • Targeted Labs: cbc, chems, HPP, CVD, other [assess for anemia, CVD, HP, sarcoid, vasculitis] • Bronchoscopy (BAL, TBBx, EBUS) [assess for any parenchymal lung disease that produces infiltrates on CXR/CT] • Surgical lung biopsy (VATS, mede) [assess for any parenchymal lung disease that produces infiltrates on CXR/CT] Spectrum of Dyspnea & Respiratory Syndromes “Normal” CXR/CT • Asthma • COPD & emphysema • Occupational “asthma-like” syndromes • Cardiac causes • Upper airway disease • Pulmonary vascular disease • Neuromuscular disease • Other (anemia, obesity, deconditioning) Abnormal CXR/CT • Acute pneumonia syndromes, alveolitis • Chronic fibrotic diseases (IPF, CVD, sarcoid) • Pneumoconioses • Malignancy • Cardiac disease • PE • Other Clinical vignette #2 (Q4) A 45 y/o non-smoker presents with episodic dyspnea and cough of 4 months’ duration. She denies nasal drainage, wheezing or heartburn. A chest x-ray is normal. Which of the following is the next best step? a. Empiric therapy with antibiotics b. 24 hour pH monitoring c. Exercise and/or cold air challenge d. Spirometry, if airway obstruction is present, proceed with methacholine challenge test e. Spirometry, if normal, proceed with methacholine provocation test Clinical vignette #3 (Q8) 60 y/o non-smoker with progressive dyspnea over 8 mos; hx is remarkable for prior thyroid cancer, s/p 2 surgeries, XRT to neck. W/up shows normal ABGs, spirometry, lung volumes/DLCO, HRCT chest, V/Q scan. Which is next best test to establish a diagnosis? a. b. c. d. e. Open lung biopsy Flow volume loop 100% shunt study 2D echocardiogram with bubbles Methacholine provocation study Clinical Vignette #4 (Q9) 50 y/o male ex-smoker (20 pk-yrs) with DOE, daily cough +/sputum, activity intolerance, wheezing; Exam: reduced breath sounds; CXR: hyperinflated, clear; spiro: severe reduction in FEV1 with no BD response and reduced DLCO; several family members died prematurely. Which of the following is the best approach? a. b. c. d. e. Blood test to prove diagnosis, then optimize inhalers, home O2, and start intermittent monthly infusions Proceed to lung transplantation Bronchoscopy with BAL, biopsy Liver biopsy Serum cotinine levels Clinical vignette #5 (Q11) • 66 y/o WF smoker with 6-12 mos hx of progressive dyspnea, cough, activity intolerance. Exam shows clubbing of fingers, bibasilar crackles, trace edema. PFTs show reduction in DLCO and volumes with normal ratio and flows; RA PaO2 55; CXR is diffusely abnormal. What is the most likely abnormal compartment? a. b. c. d. e. Upper airways Pulmonary vasculature Small airways, tethering structures Interstitium “Bellows” or resp muscles/nerves Vignettes, Questions • • • • • • Clinical vig #1 (Q 1-3) Clinical vig #2 (Q4-7) Clinical vig #3 (Q8) Clinical vig #4 (Q9-10) Clinical vig #5 (Q11) Clinical vignette #6 (Q12) Initial Approach to Respiratory Disease • Typical Symptoms – – – – – – – Dyspnea Cough +/- sputum Activity intolerance Fatigue Chest pain Wheezing Note: pattern of sx • History – Temporal aspects • acute or chronic – Assoc systemic sx – Response to therapies – Family history • IPF, CTD • Exposures – – – – – – – Sick contacts Tobacco Occupational Hobbies Pets Drugs Radiation Classification of Lung Diseases • Obstructive Disease: asthma; chronic bronchitis; emphysema; CF; • Restriction--Intra-parenchymal disease (lung tissue is abnormal, e.g. HP, pulmonary fibrosis) • Restriction--Extra-parenchymal disease (lung tissue is normal); chest wall deformities, kyphosis, scoliosis, obesity, pleural effusions, ascites – Neuromuscular disorders (“bellows”) Clinical Vignette #1 • 22 y/o woman non-smoker with episodic chest tightness, wheezing, SOB, coughing with exposure to cold air, exercise • FMHx: allergies, eczema, asthma • Exam: tachypnea; bilat wheezes • CXR: clear • Spirometry: reduced flows (i.e. FEV1) Question 1 Which of the statements regarding this disease is incorrect? a. There has been a recent upward trend b. Death occurs frequently c. Excessive use of -agonists has been implicated d. Subgroups of patients are at greatest risk e. Inadequate use of certain medications have been implicated Question 2 All of the following features are typical for bronchial asthma except: a. Airway hyperreactivity b. Severe hypoxemia c. Obstructive impairment with reversibility d. Mild increase in diffusing capacity (DLCO) e. Airway inflammation Spirometry • Two main measurements: – total volume exhaled (FVC) • lung/thorax expansion – HPP, IPF - restrictive lung diseases – volume exhaled in 1st second of exhalation (FEV1) • airway diameter – obstructive lung diseases » asthma, emphysema, chronic bronchitis, etc. Question 3 • What is the single best maintenance therapy for chronic moderate asthma? a. b. c. d. e. Prednisone Albuterol or epinephrine Inhaled steroids Cromoglycates Leukotriene blockers Question 5 A 20 y/o with a history of episodic asthma presents to the emergency department (ED) with dyspnea, wheezing, and chest tightness of several days duration. A PEFR was 200 1/min. Inhaled -agonists were administered 30 minutes apart x 3. She became asymptomatic. Which of the following is the next best step? a. Send home with -MDI q 4 hours b. Send home with inhaled steroids and PRN MDI c. Begin IV aminophylline, admit for observation d. Administer p.o. steroid in ED, discharge home with steroid taper over two weeks and PRN -MDI e. Assess ABGs and CXR prior to further treatment Question 6 Reversible factors that may contribute to "steroid-dependent" asthma include all of the following except: a. Misdiagnosis of asthma b. Presence of a co-morbid disease (i.e., sinusitis, GERD, etc.) c. Steroid receptor polymorphism d. Patient non-compliance with medications e. Poor control of environmental triggers Question 7 A 30 y/o non-smoker presents to the clinic with a 3 year history of episodic cough, chest tightness, and wheezing. She meticulously uses a -MDI at least 2 puffs every 6 hours with good relief of symptoms. She takes several additional puffs at night to help with sleep. A month ago, after an acute URI, she required ER care. She was very aggressively treated and discharged home on nebulized albuterol, atrovent, humibid, and theo/albuterol tablets. What is the single most important intervention now? a. Establish the correct diagnosis (i.e., obtain a methacholine provocation test) b. Carefully quiz the patient / family about compliance issues c. Instruct regarding proper MDI technique, spacer device, home PEFR monitoring d. Add inhaled corticosteroids e. Check theo level and optimize the dose Asthma "Mimics": Differential Diagnosis • • • Overlapping airway disorders – Chronic bronchitis and emphysema (COPD) – Cystic fibrosis – Bronchiectatic syndromes Anatomical airway obstruction – Foreign bodies – Laryngospasm, edema – Vocal chord paralysis – Laryngotracheobronchomalacia – Benign / malignant endobronchial tumors Other conditions associated with wheezing – Congestive heart failure ("cardiac asthma") – Pulmonary embolism – Aspiration (gastroesophageal reflux) – Loffler's syndrome – Factitious asthma (vocal chord dysfunction) Variable Extrathoracic : Fixed Upper Airway Obstruction Staging of COPD Criteria FEV1 % pred % of all pts Physician Mortality years I 50% +++ Generalist Average 30% 1 yr, Stage II III 35-49% < 35% ++ + Gen/Pulm Pulm/Gen at 10 90% 10 yr Intermediate Intermediate Yes Occasionally QOL Good Poor Cost Low High Need for ABGs? No Yes Need for acute care? Rarely Often Pre-op risk Moderate Modified from: ATS statement. Low Am J Respir Crit Care Med 1995;152;S83. High Which of the following are the best long term therapies for COPD to improve outcomes? (Q10) a. Inhalers (i.e. BDs) b. Prednisone c. Home O2 d. Smoking cessation e. Pulmonary rehab Other Imaging Modalities of the Thorax • • • • • • • • Computed Tomography (CT) chest Ventilation/Perfusion scan (V/Q scan) Pulmonary Angiogram (PA gram) Fluoroscopy; Tomograms Rib Films MRI chest (i.e. vessels, heart), spine Other cardiac studies (echo, thallium) PET scan Restrictive Lung Disease: Definition • Restrictive lung diseases are a group of conditions with a decreased ability to expand lungs to full capacity (can’t get air in) • Physiologically restrictive lung diseases are defined by reduced total lung capacity, vital capacity and functional residual capacity, often with preserved air flow. • Diagnostic Hallmark: a reduction in lung volumes while airflow is preserved • Oxygenation can be normal to decreased • Severity of restriction is measured by total lung capacity (TLC) Classification of Restrictive Lung Diseases • Intra-parenchymal disease (lung tissue is abnormal, e.g. pulmonary fibrosis) • Extra-parenchymal disease (lung tissue is normal) : altered/reduced thoracic cage compliance – chest wall deformities, kyphosis, scoliosis, obesity, pleural effusions, ascites – Neuromuscular disorders (“bellows”) Clinical Evaluation for Restrictive Lung Disease • History: dyspnea; activity intolerance; cough; orthopnea; reduced cough strength • ROS: exposures; associated symptoms; comorbid disease • Exam: decreased excursion; crackles; shallow rapid respirations; clubbing • Spirometry, Volumes, DLCO, O2 • Chest Radiographs • Targeted Labs Extra-parenchymal Disorders The chest wall, pleura and respiratory muscles are the components of respiratory pump (“bellows”). Disorders of these structures will cause lung restriction and impair ventilatory function. These are grouped as: • Non-muscular diseases of the chest wall. • Neuromuscular disorders. Extra-parenchymal Disorders • Diseases of the pleura & thoracic cage decrease compliance of respiratory system. • There is reduction in lung volumes, VA. • Hypoventilation with increased PaCO2 • Secondarily, atelectasis occurs leading to V/Q mismatch hypoxemia. Interstitial Lung Diseases • Common clinical, physiologic, and radiographic presentation – Dyspnea, diffuse interstitial abnormalities on CXR, and restriction on PFTs • Heterogeneous group of disorders • Affect the interstitium more than the airways and alveoli • Represent progressive inflammation and/or scarring processes Causes of ILD • • • • Infectious (acute): viral, pcp CHF (MS) Neoplastic (lymphangitic ca) Occupational/environment – inorganic-asbestos, silica, cwp – organic-HP (allergic alveolitis) – Gases (NO), fumes • Drugs • Radiation • Collagen-vascular disease – RA, Scleroderma, Ank Spon • Traumatic (fat emboli) • Acute interstitial pneumonitis • Idiopathic pulmonary fibrosis • Eosinophilic granuloma (HX) • Sarcoidosis • LAM • Veno-occlusive disease • Other Helpful Classification Interstitial Lung Disease Occupational Asbestos Silica Coal Organic Iatrogenic Granulomatous Radiation Sarcoidosis Chemotherapy Hypersensitivity Amiodarone Methotrexate CTD Other Idiopathic Scleroderma PM/DM RA SLE Histiocytosis LAM IPF NSIP COP AIP RB-ILD DIP High Resolution Chest CT • Ground glass – Represents early inflammation – More steroid responsive in certain entities • Fibrosis – Chronic scarring – Accompanied by traction bronchiectasis – Not steroid responsive UIP Slide courtesy of KO Leslie, MD. HRCT findings: linear and reticular opacities • Intralobular interstitial thickening – “fine reticular pattern” with lines of opacity separated by a few mmm – Fine lacy or netlike appearance – When seen in fibrosis, often seen in conjunction with dilated bronchioles (“bronchiolectasis”) – DDX: • IPF • Chronic hypersensitivity pneumonitis • Pneumoconioses • ILD: NSIP, DIP • Lymphangitis carcinomatosis • Pulmonary edema • Pulmonary hemorrhage • Pneumonia • Alveolar proteinosis Figure 3-24 Stage II Reticular nodules and BHL Clinical vignette #6 (Q12) 50 y/o male sedentary heavy smoker, farmer with progressive activity intolerance, fatigue; has birds inside the home; BMI is 34; Exam is notable for difficulty with speech and lying flat, but clear lungs; spirometry shows mild restriction, normal ABGs, HRCT chest & 2D echo. What is the next best step to clarify the diagnosis? a. Duplex LEs & V/Q scan b. Cardiology consult for a heart cath (both R and L) c. Bronch with BAL, possibly biopsy d. Serologies for extrinsic allergic alveolitis (farmer’s lung or psittacosis) e. Sitting/supine spiro, resp muscle assessment (MIP/MEP) Lung Volume Measures • • • • Vital capacity (VC) Residual volume (RV) Functional residual capacity (FRC) Thoracic gas volume (TGV) Lung Volumes in Disease Neuromuscular Disorders • Diseases affecting respiratory muscles, nerves, or NMJ • Muscular dystrophies, Guillain-Barre syndrome, ALS / Polio, myasthenia gravis. • Lead to dyspnea and respiratory failure. • The progress of disease can be monitored by FVC and blood gases. • Treat the underlying cause or assist ventilation. Pleural Diseases • Pleural effusion can be acute or chronic. • Pleural thickening / scarring / plaques– chronic disease results in reduced compliance of the lung and prevents expansion. • If the disease is bilateral – may cause restrictive lung disease. • Treatment = underlying disease. Diseases of the Chest Wall • Deformity of thoracic cage such as kypho-scoliosis, thoracoplasty. • Scoliosis – lateral curvature of spine, kyphosis – posterior curvature. • Patients develop exertional dyspnea, rapid shallow breathing. • Later complications = Hypoxemia, hypercapnia and cor-pulmonale. • Cause of death is respiratory failure or intracurrent pulmonary infection. • Treatment is non-invasive or invasive chronic ventilation. Causes of Oxygenation Failure • • • • Pneumonia syndromes Acute lung injury / ARDS Pulmonary edema, alveolar hemorrhage Shock syndromes Causes of Ventilatory Failure • • • • Depressed MS COPD; UAO Weakness, NMS Obesity / OSAS