Women`s Health – Deborah Ehrenthal
advertisement

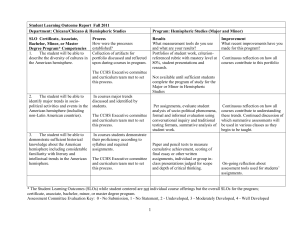
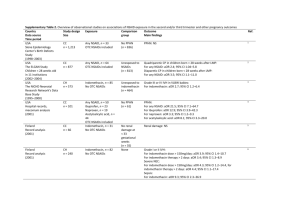
Using Clinical Data to Study Women’s Health Deborah Ehrenthal, MD Christiana Care Health Services Using Clinical Data to Study Women’s Health Deborah Ehrenthal, MD Christiana Care Health System Using Clinical Data to Study Women’s Health • Retrospective cohort studies • Studies to measure the effectiveness of system change • Linking data to study the life course Women’s Health Across the Life Course • • • • Demographic Psychosocial Behavioral Medical Reproductive Years Perinatal Outcomes • Mother • Neonate • Woman’s health status • Child’s health status Later years Breadth of Clinical Data at CCHS Inpatient Outside Sources Laboratory Pharmacy Blood Bank Individual Outpatient Billing Discharge Limitations & Strengths Limitations You work with the data you have, not the data you wish you had. Clinician determined outcomes can lead to some variation and difficulty quantifying disease severity. Data is collected for clinical purposes at variable intervals. Definitions can change over time. Challenging to pull data. Strengths Large cohort Real world diversity Real world setting Lower cost Shorter time-line Rich Data Source for Reproductive Age Women: CCHS Deliveries, 2008 Christiana Hospital (7538) 55% of births in Delaware Women’s Health Group (1395) Healthy Beginnings (533) Medical co-morbidity and the risk of prematurity in blacks Does the higher prevalence of medical co-morbidities among black women account for their increased risk of prematurity? Preterm birth rates, US Ehrenthal DB, Jurkovitz C, Hoffman M, Kroelinger C, Weintraub W. A population study of the contribution of medical comorbidity to the risk of prematurity in blacks. Am J Obstet Gynecol. 2007 Oct;197(4):409 e1-6. Retrospective Cohort Study Using Clinical Data: Adjusted Odds Ratios Maternal risk factor < 32 weeks aOR (95% CI) <37 weeks aOR (95% CI) <1500 g aOR (95% CI) <2500 g aOR (95% CI) African American 2.5 (2.0-3.1) 1.5 (1.4-1.7) 2.9 (2.3-3.7) 2.1(1.9-2.4) Hispanic 1.1 (0.7-1.7) 0.9 (0.8-1.1) 1.5 (1.0-2.3) 1.1 (0.9-1.3) Asian 2.3 (0.7-7.4) 0.8 (0.6-1.0) 1.1 (0.5-2.2) 1.1 (0.9-1.5) ORF=1 1.8 (1.4-2.2) 1.5 (1.3-1.6) 2.1 (1.6-2.6) 1.8 (1.6-2.1) ORF=2 or more 3.5 (2.2-5.4) 3.2 (2.5-4.1) 3.7 (2.3-6.0) 3.8 (3.0-5.0) Age < 20* 1.6 (1.2-2.2) 1.3 (1.1-1.5) 1.3 (0.9-1.9) 1.4 (1.2-1.7) Gestational hypertension 3.6 (2.8-4.6) 3.5 (3.1-4.0) 5.2 (4.1-6.7) 3.3 (2.9-3.8) Gestational Diabetes 0.8 (0.5-1.3) 1.2 (1.0-1.5) 0.7 (0.4-1.2) 0.9 (0.7-1.1) NS = not significant ORF= Overall risk factor. ORF=1: presence of one risk factor compared to no risk factor ORF=2: presence of two risk factors or more compared to no risk factor * The ORs associated with the other age categories (30-39 and ≥40) are not significant except for the outcome Gestational Weeks <32 weeks where the OR associated with age≥40 is 1.8 (1.0-3.0) Risk Factors for Cesarean Delivery, CCHS Cesarean Delivery Rates, US What are the risk factors at CCHS? Black race (aOR=1.4) Age 35+ (aOR=1.7) BMI 40+ (aOR=4.5) Weight gain (aOR=1.4) Gestational DM (aOR=1.4) Gestational HTN (aOR=1.4) Post-dates (aOR=1.6) Labor induction (aOR=1.9) Ehrenthal DB, Jiang X, Strobino DM. Labor induction and the risk of a cesarean delivery among nulliparous women at term. Obstet Gynecol. 2010 Jul;116(1):35-42. Trends in Cesarean Delivery, Anemia, and Peripartum Transfusion, CCHS 2000-2008 40 16 35 14 30 12 25 10 20 8 15 6 10 4 5 2 0 0 2000-1 2002-3 2004-5 2006-7 Year C-section Hgb <10.5 Transfusion 2008 Transfusion rate per 1000 deliveries Percentage Cesarean Delivery and Hgb <10.5 g/dL Trends in Cesarean Delivery, Anemia and Transfusion Rates, 2000-2008 Joint Effects of Anemia and Cesarean Delivery on the Odds of Transfusion Anemia (Hgb<10.5) Cesarean Delivery Number of women (%) Adjusted Odds Ratio* 95% CI No No 35048 (63.6) 1 Reference Yes 4133 (7.5) 2.98 2.36, 3.78 No 14185 (25.7) 3.52 2.56, 4.82 Yes 1746 (3.2) 17.08 13.15, 22.17 Yes *Adjusted for all factors included in the full model. Differences in the Prevalence of Anemia Contribute to Disparities in Outcomes 25 Percentage Anemic 20 15 Hgb<10.5 g/dL Hgb <9.5 g/dL 10 5 ul l ip 1 aro pr io us r 2 birt or h m or e Bl a H ck is pa ni c W hi te As ia O n th er s >3 5 N < 20 ye a 20 rs – 35 0 Demographic and Obstetrical Characteristics Limiting Elective Early Term Delivery Between 1990 and 2005 in the US: • Preterm delivery increased from 10.6% to 12.7% • Decrease in delivery at 40 and 41 or greater weeks • Increase in term deliveries between 37-39 weeks • Early term now defined: 37-38 weeks The “Term” Group, 1990 and 2006, US Source: Martin JA, Hamilton BE, Sutton PD, Ventura SJ, et al. Births: Final data for 2006. National vital statistics reports; vol 57 no 7. Hyattsville, MD: National Center for Health Statistics. 2009. Effectively Decreasing Elective Early Term Delivery, CCHS 2005-2009 Policy Change Data Linkage Across Institutions: The Delaware Birth Defects Registry Antenatal diagnosis Diagnosis at birth Postnatal diagnosis Delaware Center MFM CCHS Bay Health St. Francis Nemours: Outpatient Bayhealth MFM Nanticoke Birth Center Beebe MFM Nemours: Inpatient Public Health: Fetal Death, Infant Death, Birth Records, Newborn Screening Linked Database Understanding Determinants of Obesity Fetal origins of adult disease Influence of early factors, eg birthweight, breast feeding, maternal medical problems Role of social determinants Role of health care Maternal Perinatal Risks Maternal Medical/ Behavioral Risks Demographic & Social Factors Moderating Factors Neonatal Characteristic Childhood Obesity Mediating Factors Adult Obesity Delaware Mother-Baby Cohort: Linking CCHS and Nemours Obstetrical Other Inpatient Pharmacy Laboratory Mother+Baby Mother Laboratory Pharmacy Baby Billing Outpatient Outpatient Discharge Billing Discharge It Takes a Village My team • Kristin Maiden, PhD • Stephanie Rogers, RN • Ashley Stewart, MS, CHES • Amy Acheson, MA • Kate Stomieroski • Richard Butler CCOR • William Weintraub, MD • Claudine Jurkovitz, MD, MPH • Mark Jiang, MD, BS • Paul Kolm, PhD • James Bowen, MS CCHS ObGyn • Matthew Hoffman, MD, MPH • Melanie Chichester, RN • Suzanne Cole, MD • Richard Derman, MD, MPH CCHS Pediatrics • Louis Bartoshesky, MD, MPH • David Paul, MD TJU/Nemours Pediatrics • Judy Ross, MD • David West, MD • Sam Gidding, MD University of Delaware • Ben Carterette, PhD • Michael Peterson, PhD Johns Hopkins Bloomberg School of Public Health • Donna Strobino, PhD CDC • Charlan Kroelinger, PhD