Medicare Bundled Payment Presentation
advertisement
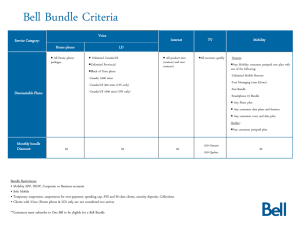
Bundled Payment Initiative: Your time to get ahead of the crowd? Paul Lee, Sharon Cheng, Marian Lowe Strategic Health Care September 29, 2011 Facilitating Change Test new payment and service delivery models Work across Medicare, Medicaid, and CHIP programs Expand the scope and duration of models proven effective IF those models are proven to also lower costs. $10B in direct spending for 2011-2019 Innovation Center Projects Comprehensive Primary Care (CPC) Initiative Multi-payer initiative to test new service delivery and payment models Monthly care management fee to primary care practices, opportunity for shared savings 5-7 localities will be selected Criteria For physicians: 60% of patients must be in participating plans & Medicare, use EHR, have at least 200 FFS Medicare patients For plans: Commit to contracts with participating practices that offer shared savings; provide attribution methodology with CMS Deadline: LOI due November 15; Application due January 17 5 Reasons to Participate Leadership opportunity Align payers Promote services Decrease readmissions, unnecessary services Physician partnerships Cautions Medicare margins are thin You are unlikely to beat your 2009 baseline You need funds to begin care redesign Deadlines Letter of intent Model 1: October 6, 2011 Models 2, 3, and 4: November 4, 2011 Application Model 1: November 18, 2011 Models 2, 3, and 4: March 15, 2012 Four options for participation Services Risk Goal Model 1 Part A inpatient Low: 0-2% discount, welldefined bundle Align physicians through gainsharing Model 2 Part A inpatient, Part B, including post-acute, DME, and Part B drugs Medium: 2-3% discount; 30, 60 or 90 day complicated bundle Offset revenue lost with reduced readmissions, other improvements Model 3 Post-acute Part A and B, including DME and Part B drugs High: 2-3% discount; long, undefined bundle Offset revenue lost to lower-intensity post-acute care Model 4 Part A inpatient and professional services during the stay Medium: 3% discount; short, discrete bundle Align physicians, reduce inpatient costs Have we seen this unicorn? Gainsharing Demo MedPAC and CBO models CARE tool research ACE Demo Designing the bundle CMS will provide dataset of fee-for-service Medicare claims, 2009 Use clinical logic to define related claims and choose the length of the episode Determine bid amount Propose quality measures Strong applications Offer significant savings Affect many beneficiaries and conditions Scalable and replicable Include other payers Incorporate IT Are “shovel ready” Opportunities for assistance SHC can help prepare you for bundling Evaluate your readiness to participate Prepare the letter of intent Prepare the data use agreement and work with you to analyze CMS administrative data Prepare or review and provide feedback on applications For Assistance Gwen Mathews, Partner Strategic Health Care 202.266.2600 gwen.mathews@shcare.net