The-View-from-Washington
advertisement
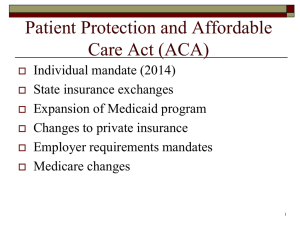
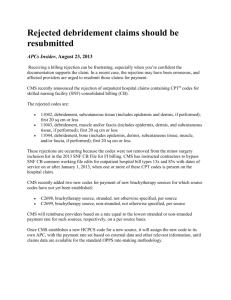
Cynthia Morton, Executive Vice President National Association for the Support of Long Term Care (NASL) June 2012 Supreme Congress CMS Court Whether Medicaid expansion is coercive on states Constitutionality of individual mandate Decision expected last week of June, begin of July Possible outcomes: o Entire ACA upheld (remains valid) o Individual mandate unconstitutional but severable o All or major parts of ACA declared unconstitutional Sequestration 2% cut Enormous pressure to cut o Pent-up frustration among conservatives about fiscal recklessness in Washington Lame Duck Session– o Doc “fix” past 12-31-12 o Therapy Cap Exceptions Extension, fatigue o Reauthorization of Highway Trust Fund o Alternative Minimum Tax (AMT) o Research & Development Tax Credit o Bush 2001 Tax Cuts o National Health Service Corps Scholarship Program & F. Edward Hebert Armed Forces Health Professions Scholarship & Financial Assistance Program (Tax) o 50% of cuts come from defense; 50% from domestic o o o o o programs 2% across-the-board cuts to Medicare Medicaid and CHIP exempt Takes effect January 2013 Congress may exempt defense; may cut other programs to offset defense cuts Medicare is very vulnerable No extensive policy changes this year in the payment update (also called market basket). FY 2013 SNF MB projection is 2.6% o Subtract the productivity adjustment; estimated to be about 1% o FY 2013 MB update: 1.6% +/- 0.2% By statute, CMS must provide the full market basket and could only be changed by Congress. According to CMS: • No current payment system for any individual provider type provides both the quality and the cost efficiency that both CMS and Congress believe can be achieved. • Playing with payment system as a way to achieve better quality savings for Medicare has been going on since the inpatient hospital DRG system was introduced. • None of the tinkering and the changes have succeeded. • The provider types are silos with no real connection between them: they lack team work, communication, beneficiary transition concern etc. • Utilization drives care: the more the merrier. Payment for overdoing and unnecessary services. Population Health Experience of Care Integrated CareJourneys not Fragments Patient centered Prevention Reduction of medical errors/ patient safety Based on best science available Per Capita Cost Cost ReductionSpecifically NOT by withholding or reducing care 8 Inpatient Hospital Medicare Medicaid Managed Care Long Term Hospital Inpatient Rehab Physicians SNF Home Health 9 Medicare Medicaid Dual Care Models Medical Homes ACOs Bundled Payors Managed Care 10 Care Coordination through Financial Alignment Demo 3 years; Enrolling January 2013 Integrates benefits and aligns financial incentives between the two distinct and separate programs Duals: 9.1 million of 97 million on Medicaid or Medicare Sickest, most expensive, half have three or more chronic conditions and six in ten have cognitive limitations o Medicaid spends 69% of dollars on LTC (includes HCBS) o Medicare spend 6% on SNF o 60% 40% 20% 0% 27% 39% 16% 15% Medicare Medicaid Spending Enrollment CMS expects 26 states to participate Tests Two Models: o Capitated Model: Three-way contract among State, CMS and health plan to provide comprehensive, coordinated care in a more cost-effective way. o Managed FFS Model: Agreement between State and CMS under which States would be eligible to benefit from savings resulting from initiatives to reduce costs in both Medicaid and Medicare. The challenges and the potential of this health reform experiment are enormous Combined data set-- individual state profiles that show the demographics, utilization, and spending patterns and costs of dually eligible individuals in each state This is a very large demo. Status: 26 States are actively pursuing one or both of the models (18 States capitated, 6 States managed FFS and 2 States both) State Draft Proposals: o 26 States (AZ, CA, CO, CT, HI, ID, IA, IL, MA, MI, MN,MO, NM, NY, NC, OH, OK, OR, RI, SC, TN, TX,VT, VA, WA, and WI) have posted their draft proposals for public comment. Official Proposal Submission to CMS: o Proposals can be found online: http://www.cms.gov/Medicare-MedicaidCoordination/Medicare-and-MedicaidCoordination/Medicare-MedicaidCoordinationOffice/FinancialModelstoSupportStatesEffo rtsinCareCoordination.html Partnership for Patients: Public-private partnership to improve the quality, safety and affordability of health care for all Americans by reducing hospital readmission rates by 20% by the end of 2013. Community Care Transitions Program: Provides support for high-risk Medicare beneficiaries following a hospital discharge. 23 sites will work with CMS and local hospitals to provide support for patients as they move from hospitals to new settings, including skilled nursing facilities and home. Independence at Home: Tests a new service delivery model that utilizes physician and nurse practitioner directed primary care teams to provide services to high cost, chronically ill Medicare beneficiaries in their homes. Launched in April 2011 “Take the Pledge”--More than 6,500 partners, including over 3,167 hospitals, 2,345 physician, nursing and pharmacy organizations, 892 consumers and consumer groups, and 256 employers and unions. Focus on physicians, nurses and other clinicians working in and out of hospitals to make patient care safer and to support effective transitions of patients from hospitals to other settings. Two Concrete and Measurable Goals: o Keep patients from getting injured or sicker. By the end of 2013, preventable hospital-acquired conditions would decrease by 40% compared to 2010. o Help patients heal without complication. By the end of 2013, preventable complications during a transition from one care setting to another would be decreased so that all hospital readmissions would be reduced by 20% compared to 2010. Tests models for improving care transitions from the hospital to other settings and reducing readmissions for high-risk Medicare beneficiaries. Goals: o Improve transitions of beneficiaries from the inpatient hospital setting to other care settings, to improve quality of care, o Reduce readmissions for high risk beneficiaries, and o Document measurable savings to the Medicare program. Community organizations to partner with nursing homes Apply on a rolling basis $500 million available for 2011-2015 Targeting long stay resident 30 CCPT participants so far Announced March 2012 Targeted to long stay dual eligible Goal: o Reduce costly and avoidable hospitalizations Funding organizations to partner with nursing homes $128 million available Propose your own evidence based intervention and improvement strategy Applications were due June 14th ACA– Penalizes hospitals with greater-than-expected readmission rates for specific conditions. Payment reduction will be determined by an adjustment factor based on an assessment of excess readmissions, with a maximum payment reduction of 1 percent in 2013, 2 percent in 2014, and 3 percent in 2015 and beyond. An excess readmissions ratio will be calculated based on measures of readmissions currently used in the hospital inpatient quality reporting (IQR) program. Penalty applies to three conditions: o acute myocardial infarction (AMI), o heart failure o pneumonia Under Affordable Care Act Section 3022 Medicare Shared Savings Program An organization whose primary care physicians are accountable for coordinating care for at least 5,000 Medicare beneficiaries o Having a hospital or specialist in the ACO is optional o Secretary may include other providers o At least 50% of the primary care physicians must be meaningful electronic health record users by the start of the second reporting period Legal entity recognized under State law o shared governance o Participants have appropriate proportional control over decision making process Reimbursement & Care Delivery Bottom Line: Whether or not providers apply to become ACOs is unknown, but payers and providers are preparing their organizations for ACO-like changes in reimbursement and care delivery. 22 A “bundled payment” is simply a single payment for a package of services delivered by a group of providers during a defined episode of care. The Secretary shall develop a pilot program for integrated care during an episode of care provided to an applicable beneficiary around a hospitalization Implementation January 2013 Duration of pilot – 5 years Secretary to submit plan for implementation of an expansion of the pilot program no later than 01/2016 Model 2 – Acute and PAC bundle Model 3 – PAC bundle only Applications due June 28th, 2012 May expand the program nationwide after 01/2016 if it reduces spending and either does not reduce quality of care or improves quality of care. According to CMS’ Request for Application… Similarities: • The ACO concept of capitated payment or shared savings and a bundled episodic payment model both create a framework that rewards providers for taking accountability for the triple aim outcomes. Differences: • Bundled episodic payment models support accountability at the patient level while the ACO model does so at the population level. This reduces operational complexity at the provider level. Quality measures are coming from CMS and others Partnership to Improve Dementia Care -- reduce use of antipsychotic drugs in nursing home residents by 15% by end of 2012 o CMS data show that in 2010 more than 17 percent of nursing home patients had daily doses exceeding recommended levels. National Quality Forum’s MAP (Measures Application Partnership)– contract with HHS to develop measures across settings. June 2012 Report – 26 measures sensitive to the unique needs of dual eligible beneficiaries. o detecting and treating depression o screening older adults for fall risk o unplanned hospital readmissions within 30 days of an initial stay as a key measure of quality for the dual eligible population. Includes a “starter set” of seven that are most ready for immediate implementation in the field http://www.qualityforum.org Last year’s PPS rule and various OIG reports are telling us that our stakeholders do not understand the value of the amount of therapy we provide. Working jointly with American Health Care Association Developed a crosswalk to translate functional measures used by some companies to the Modified Barthel Index as used in the CARE tool project Once validate the crosswalk, begin to examine QM’s. Concern is that measures will be sensitive to change in the patients we see If we don’t do it, CMS will. Growing recognition of the importance of HIT and the role of LTC providers in ensuring smooth care transitions and avoiding readmissions Demonstrating “Meaningful Use” is how hospitals and eligible professionals get the payments LTPAC not included specifically in Stage 1 or 2 of Meaningful Use (grant program from HiTECH) LTPAC providers are forging ahead anyway General Requirements That Must Be Met: Certified EHR is used in a meaningful manner, including electronic prescribing Certified EHR is connected in a manner that allows for the exchange of health information Entity is capable of reporting on clinical quality measures and such other measures as selected by the Secretary of HHS Physicians o Physician adoption of any EHR system has more than tripled since 2002, going from 17 percent to 57 percent in 2011 (NCHS Data Brief). o The adoption of basic EHRs has doubled since 2008, going from 17% to 34% in 2011 (NCHS Data Brief). o Adoption has grown significantly among important subgroups of physicians including small practices and rural providers. Hospitals o Hospital adoption has more than doubled since 2009, increasing from 16% to 35% Over 2,800 hospitals and more than 90,000 doctors have received $5 billion in incentive payments for ensuring meaningful use of health IT since the program inception LTPAC Challenge Grants 4 Challenge Grants to Massachusetts, Maryland, Oklahoma, and Colorado through the state-based Health Information Exchange (HIE) program Focused on “improving long-term and post-acute care transitions” Written by NASL and others in the Collaborative http://www.ltpach ealthit.org/content /2012-2014roadmap-hit-ltpac State of play in information technology for our sector Keep Calm and Carry On! Know that our landscape is changing (when does it not?) Your data is important to your future Advocacy is important Cynthia Morton Executive Vice President Cynthia@nasl.org 202 803-2385 www.nasl.org