Respiratory Education Slides
advertisement

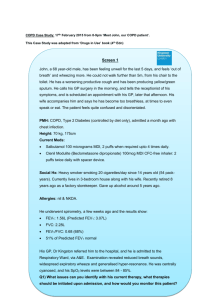
Management of End-Stage COPD Dr Patrick Fitzgerald GPwSI Palliative Care Sr Doreen O’Hara COPD CNS End-Stage COPD Identification Prognostication Holistic Assessment Pharmacological Management Non-pharmacological Management Advance Care Planning IDENTIFICATION AND PROGNOSTICATION Fig 1 Typical illness trajectories for people with progressive chronic illness. Adapted from Lynn and Adamson, 2003.7 With permission from RAND Corporation, Santa Monica, California, USA. Murray, S. A et al. BMJ 2005;330:1007-1011 Copyright ©2005 BMJ Publishing Group Ltd. Holistic Assessment Physical - How’s things? Emotional - What worries do you have? About the future? Personal - How are you coping? Social/Spiritual - Do you need any help at home? From chaplaincy? Information/Communication - GP letter/OOH/DNs Symptom control Common symptoms include: Dyspnoea Pain Anxiety/Depression Fear/Panic GI symptoms Cachexia and poor nutrition Dyspnoea Management Adapted from: Rocker G et al. Thorax 2009;64:910-915 Conscious experience arises from the sensory cortex If the sensory cortex perceives a mismatch between ventilatory demand and the body's ability to respond Treatment Once all COPD treatment is optimised then 1st line is immediate-release opiate: “There is evidence in favour of using oral or injectable opioid drugs for the palliative treatment of breathlessness” Cochrane review 2001 Low dose Oramorph to start eg. 1.25-2.5mg 4 hourly Remember: 30mg codeine @ = 3mg morphine Non-pharmacological Non-pharmacological interventions Cochrane 2008 “…interventions can help to relieve shortness of breath: vibration of patient's chest wall, electrical stimulation of leg muscles, walking aids and breathing training. Further interventions identified were counselling and support, either alone or in combination with relaxation-breathing training, music, relaxation, a hand-held fan directed at a patient's face, case management and psychotherapy. Reassurance Talking though fears Adjuncts Aperients: OPIOIDS ARE ALWAYS CONSTIPATING Anti-emetic for first week – which one? Benzodiazepines: “…on the basis of seven included studies… there is no evidence for a beneficial effect of benzodiazepines in the relief of breathlessness in adults with advanced disease”Benzodiazepines caused more drowsiness as an adverse effect compared to placebo, but less compared to morphine. Cochrane Review 2009 BUT – good for panic of breathlessness? Lorazepam 0.5-1mg tds prn: short-acting and sub-lingual formulation Steroids Harry is 82 Called by daughter to review Worsening breathlessness Can’t get out of chair Frail and upset OOH GP visits and wants to send to A&E Concern this is exacerbation – REVERSIBILITY? Harry gives history slowly Chest pain on inspiration More breathless past weeks Cachectic RR 25, p 98, bp 148/89, sats 90% on 24% O2 Chest - added noises noted - poor air entry 3 recent admissions to hospital, NIV last time Harry wants to stay at home Family demand admission as they feel they can’t cope Harry Issues Harry’s prognosis – what lies ahead? Harry's symptoms - what can we do? Harry’s wishes – how can we support his choice? What would be your management plan? Advance Care Planning PPC/PPD/ADRT What to record Where to record it Capacity to make decisions Who keeps the document? Where do they keep it? Who has access? EPACCS COPD Team Stockport New Palliative Care MDT Patients identified as worsening – GSF type register with plan of care developing. Interface with EPACCS Holistic assessment by Pall Care Team Management plan devised between teams Aim to support PPC Keeping patients where they want to be longer Does it stop admission? Is it OK to die in hospital? Key Worker Care Plan What Care Plan might you make for your COPD patients? Think GSF – anticipatory care Think PEPSI – holistic assessment Think COPD/Palliative Care Teams if symptoms severe – expert advice Think ACP/ADRT – patient choice in future plans Think OOH Anything else? Your Questions Contact me 07715518135 patrick.fitzgerald1@nhs.net Dr Fitzgerald 22