Slide 1 - Yorkshire and the Humber Deanery
advertisement
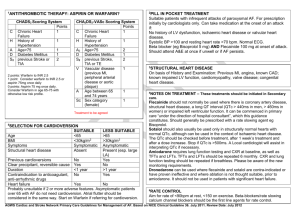
QT interval Lucy Adkinson July 2013 What we are going to cover • • • • Reminder of ECGs and what is the QT interval How to work out QTc Why do we care? What should we do or avoid? – – – – Risk factors Drugs Methadone General recommendations for practice • Evidence ECG Corrected QT : QTc • Adjust the QT for the heart rate • QTc : divide the QT interval by the square root of the preceding R-R interval – QTc = QT /√RR • Interpretation: QTc (msec) Male Female Normal <430 <450 Borderline 430-450 450-470 Abnormal >450 >470 The significance of prolonged QTc • Pro-arrhythmic state • Increased risk of ventricular arrythmia – Torsade de pointes Long QT • Inherited • Acquired: – Hypokalaemia/hypomagnesaemia – Drugs • Cardiac disease – Bradycardia, LVH, Heart failure, recent cardioversion from AF, ventricular arrhythmia Drugs and torsades • Potassium channel blockade • Modifies repolarisation and prolongs action potential • 40 + drugs linked with QT and torsade – (not all that prolong QT, cause torsade) – Drug induced torsade is relatively rare – can be as high as 2-3% with some (high risk) drugs Drugs and Torsade • Greatest with anti-arrhythmic drugs (class III) – Amiodarone, disopyramide, sotalol • In some drugs, risk only present with: – High doses – IV – Drug interaction • E.g. Ketoconazole inhibits CYP3A4 and impairs methadone metabolism – Impaired metabolism • E.g. CYP2D6 poor metabolisms may have high plasma concentrations of culprit drugs with normal doses • Hepatic or renal failure Which drugs? Drugs available associated with prolonged QT and torsade de pointes Anti-arrhythmics •Amiodarone •Disopyramide •Sotalol Psychotropic drugs •Chlorporomazine •Droperidol •Haloperidol •Pimozide Antimicrobials •Macrolides: clarithromycin, erythromycin, Antimalarials •Chloroquine Misc •Aresenic •Domperidone •Methadone •Saquniavir •Toremifine www.azcert.org http://www.azcert.org/medical-pros/druglists/list-01.cfm?sort=Generic_name Methadone • Prolongs QT – dose dependant and risk of torsade de pointes • Serious adverse events – more so than other opioids – FDA, 59 reports, 1 confirmed death from torsade • For practice – Role of ECG monitoring – Use in caution with: • • • • • • History of cardiac conduction abnormalities Ischaemic heart disease Liver disease Family history of sudden death Electrolyte abnormailites (or drugs which cause this e.g. Diuretics) Concurrent treatment with other drugs which potentially prolong QT, inhibit CYP3A4 Recommendations for practice • Be aware – polypharmacy in palliative care • But put in context – 300 patients in specialist palliative care unit • 48 (16%) had prolonged QT • Only 2 severely prolonged - >500msec • They both had IHD – Commonsense at end of life • If prescribing a drug: – Understand the pharmacology, drug-drug interaction, impaired elimination – Avoid concurrent use of QT prolonging drugs – Use lowest dose effective • If known prolonged QT avoid use of risk drugs • Cardiac disease (or other risk factors), avoid if possible – If no alternative, monitor ECG before and after and ensure electrolytes monitored • Report drugs which have prolonged QT to MHRA (yellow card) • Consider torsades as possible cause of palpitations, syncope, seizure like activity Summary • • • • • Review cardiac history Review drug history prior to any new drugs Check out drugs in PCF/ online Avoid multiple QT drugs In particular haloperidol, methadone, domperidone, macrolide antibiotics References • PCF – pages 727-733 • www.azcert.org • European Medicines Agency http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human /referrals/Domperidonecontaining_medicines/human_referral_prac_000021.jsp&mid=WC0b01ac 05805c516f