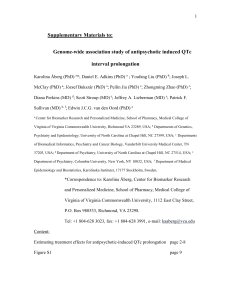
QT Prolongation Considerations for IM Hospitalists
advertisement
QT Prolongation Considerations for IM Hospitalists Lenny Noronha, MD UNM Hospital Medicine Best Practices 2/8/12 Outline • Review cardiac cycle, pathophysiology • Discuss risk factors for Prolonged QT, TdP • Analyze medication classes prescribed by Hospitalists • Propose “Best Practices”, discuss Special thanks to: • • • • • • • Carlos Macias, MD Brook Parrish, MD Davin Quinn, MD Nicole Klein, MD Vincent Zummo, PA Katya Calvo, MD Shmuel Inbar, MD Case 44yf adm to Red Med team for GI sx, AMS Adm to Pres 1 wk prior, ureter stented, on cipro 500 po bid. 1. AMS: “MRI pending”. Attributed to K 2.8 and ketones in urine. 2. UTI: Order cultures, start zosyn 3. “Prolonged QTc” Will repeat EKG after electrolytes replaced. 4. Lip lac may need to be sutured. 5. Pain control: tylenol and oxycodone 6. Hospital issues Case cont’d Pt seen by neuro before IM eval. “Feeling funny…my heart fluttering like a butterfly” QTc 600 documented. Impression: • LOC c tongue abrasion, split lip, most likely secondary to seizure • Low potassium • Prolonged QT Initial ED EKG, K 2.8, QTc 602 HD 2, K 3.6, QTc 511 Subsequent course HD 2 EEG normal. Cardiology consult HD 3 after several runs of nonsustained polymorphic VT (8-9 beats). QTc range 528 – 699 during admission, despite electrolyte replacement Outpt EKG from 1yr prior: NSR, QTc 467 ID, Pulm consults for complex infection Started on Bb, titrated to tolerance Family all had EKG’s. Daughter’s QTc 462. Pt dc’d c LifeVest, had ICD placed after 14 d course abx, ureteral stone/stent removed ZOLL LifeVest Wearable Defibrillator http://lifevest.zoll.com/medical-professionals/ What is normal, prolonged? “Prevention of Torsade de Pointes in Hospital Settings”, Barbara Drew, et al, JACC Scientific statement, 2010; 55, 9:934-947 “The QT interval: Too long, too short or just right”, Sami Viskin, Heart Rhythm, May 2009,: 6, 5: 711-715 Next 9 slides adapted from: Antiarrhythmic Overview Carlos Macias, MD Jan 31st 2012 Fellows Conference Part 1. Basic principals • Cardiac action potential – Electrical impulse of the heart is the summation of thousand of tiny electrical currents generated by thousands of individual cardiac cells. – Electrical activity of an individual cardiac cell is described by the cardiac action potential. Part 1. Basic principals • Depolarization – Phase 0 – Rapid sodium channels in the cell membrane are stimulated to open. – Allows positively charged Na ions to rush into the cell. – Voltage spike – positively directed change the transmembrane potential – Na channels are voltage dependent. – The speed of the slope determined how fast the next cell will be stimulated to depolarize. – Anything that causes the causes the slope to change will affect conduction velocity. Part 1. Basic principals • Repolarization corresponds to phases 1-3 • Accounts for most of the action potential • Time from the end of phase 0 to late in phase 3 is considered refractory period. • Duration of the action potential determines the refractory period. – Anything that increases duration of the action potential also changes the refractory period. Part 1. Basic principals • Repolarization begins rapidly – Phase 1 – Interrupted by plateau (Phase 2) “slow” Ca channels – Most important ionic shift during repol is the outflow of positive K ions. – At least six different K “currents” have been identified. – At the end of repolarization the transmembrane voltage returns to baseline. Part 1. Basic principals Part 1. Basic principals Mechanism of cardiac tachyarrhythmias Most tachyarrhythmias are thought to be due to one of the following mechanisms: – Automaticity – Reentry – Channelopathy (congenital LQTS) – Triggered activity (dig tox arryth, CCB-sens VT, TdP) Prolonged Repol sets up EAP Molecular mechanisms of inherited arrhythmias, Wolf, Berul, et al, Curr Genomics. 2008 May; 9(3): 160–168. Basic principals Triggered mechanism Ectopy triggered if threshold exceeded Current concepts in the mechanisms and management of drug-induced QT prolongation and torsade de pointes, Gupta, American Heart Journal, Jue 2007; 153: 891-899 Drug-Induced Prolongation of the QT Interval,Dan M. Roden, M.D., N Engl J Med 2004; 350:1013-1022 Notes on TdP • Usually self-limited • Typical symptoms: palpitations, syncope, “seizure-like activity” • Immediate tx: Mg Sulfate 2g IV bolus, followed by 2-4g IV infusion over 2 hours Drugs and the QT Interval — Caveat Doctor Barbara A. Liu, M.D., and David N. Juurlink, M.D., Ph.D. N Engl J Med 2004; 351:1053-1056 Patient Factors • • • • • • Female gender Age > 65 Electrolyte loss (i.e. Diuretics, Diarrhea) Cardiac disease Liver or Renal disease, Hypothyroidism Congenital LQTS (1:2500 gen population) – h/o unexplained syncope, FH sudden death < 40 Direct Drug Effects Most meds that prolong QT thought to block IKR Psychiatric • Antipsychotics • TCA’s • Lithium • Citalopram Antimicrobials • Macrolides • Quinolones •Azoles •Pentamidine •Amantadine Other • Methadone •Hydroxyzine •Loratidine •Tacrolimus •Cocaine Cardiac • Quinidine, procainamide • Flecainide • Amiodarone, Sotalol Indirect Drug Effects Common C P450 3A4 Inhibitors Cardiovasc • Diltiazem • Verapamil Psych • Fluoxetine • Midazolam Antimicrobials • Macrolides! • Ketoconazole • INH • HIV meds - Amprenavir, Delavirdine - Nelfinavir, Ritonavir Endocrine •Ethinylestradiol •Gestodene •Mifepristone •Raloxifene •Tamoxifen Others • Grapefruit juice •Resveratrol •Irinotecan FYI :This is the mechanism for patients with liver disease Clinical Features Associated with risk of TdP “Cardiac side effects of psychiatric drugs” Mackin, Human Psychopharmacology 2008; 23: 3-14. Literature: Antibiotics “Oral Erythromycin and the Risk of Sudden Death from Cardiac Causes”, Ray, NEJM 2004 Response to case reports of TdP assoc c IV erythromycin Retrospective review of TN Medicaid cohort investigated from sudden death ‘88-’93. Compared matched population “person years” of current and former users of oral erythromycin to patients using amoxicillin at time of investigation “Oral Erythromycin and the Risk of Sudden Death from Cardiac Causes”, Ray, NEJM 2004 Led to numerous letters, review articles, and… 2006 ACC/AHA/ESC Guideline Recommend removing of offending agent in patients with drug-induced LQTS 2010 ACC/AHA Scientific Statement, “Prevention of Torsades de Pointes in Hospital Settings Recommend continuous cardiac monitoring for drugs at risk to cause TdP. If QTc becomes > 500ms or increases > 60ms, seek alternative therapies, assess for drug interactions. Patients should not be transported from the unit for procedures. Literature: Antipsychotics 1980’s: Dose-dependent risk of QTP, TdP, sudden death noted with antipsychotics, especially droperidol, haldol and thioridizine 1990: UK Committee on Safety of Medicines recc gradual dose increase, EKG before and periodically in patients receiving high doses Literature Review cont’d 2007: FDA label warning for QTP/TdP from Haldol IV in response to adverse events reports. Recc: continuous tele monitoring 2010 Systematic Review (Meyer-Massetti) Methods:Cases of QTP/TdP from Pubmed, Embase, Scopus databases (1823-2009; FDA MedWatch reports (‘97-’08) Results: 70 cases, 2 deaths. 42 of 54 cases of TdP preceded by QTP 68 had identified RF TdP cases had cumulative dose 5-645 mg Deaths had cumulative doses of 530, 634 mg 2010 Systematic Review (Meyer-Massetti) Discussion - APA 2004 recc: Haldol dosing initial IV dosing 1-2mg q 2-4h Geriatric: 0.25-0.5mg q4, titrate as needed Key Conclusion/UCSF policy: - IV haldol can be given in cumulative doses < 2mg without tele/serial EKG in patients without risk factors - Cardiac monitoring if doses greater than 2mg anticipated or risk factors for TdP 3/17/09 Especially in doses over 100 mg/d Recommendation 1 (Disclosure): Clinicians should inform patients of arrhythmia risk when they prescribe methadone. Recommendation 2 (Clinical History): Clinicians should ask patients about any history of structural heart disease, arrhythmia, and syncope. Recommendation 3 (Screening): Obtain a pretreatment electrocardiogram for all patients to measure the QTc interval and a follow-up electrocardiogram within 30 days and annually. Additional electrocardiography is recommended if the methadone dosage exceeds 100 mg/d or if patients have unexplained syncope or seizures. Recommendation 4 (Risk Stratification): If the QTc interval is greater than 450 ms but less than 500 ms, discuss the potential risks and benefits with patients and monitor them more frequently. If the QTc interval exceeds 500 ms, consider discontinuing or reducing the methadone dose; eliminating contributing factors, such as drugs that promote hypokalemia; or using an alternative therapy. Recommendation 5 (Drug Interactions): Clinicians should be aware of interactions between methadone and other drugs that possess QT interval–prolonging properties or slow the elimination of methadone. Suggested “Best Practices” 1. Awareness of “Patient Factors” for prolonged QT – Age > 65 – Female – ANY cardiac disease – Hypokalemia – Hypomagnesemia – Hypocalcemia – CKD, Chronic liver disease, hypothyroidism – FH Sudden death/prolonged QT Suggested “Best Practices” 2. Awareness of chronic outpatient medications most likely to prolong QT interval - Methadone - Erythromycin (i.e. gastroparesis) - Amiodarone - Atypical antipsychotics - Tricyclic antidepressants Suggested “Best Practices” 3. Obtain EKG or tele strip measurement of QTc in patients with Patient Factors/above meds before starting AND after doses of: - Antipsychotics - Macrolides - Quinolones - Pentamidine (i.e. PJP) - CYP 3A4 inhibitors Suggested “Best Practices” Do NOT add meds than can prolong QT in patients with QTc > 500 Discontinue meds that can prolong QT if QTc increases > 60msec after addition Suggested “Best Practices” 4. Patient Education www.qtdrugs.org www.azcert.com Suggested “Best Practices” 5. Document QTc in progress note if EKG ordered to measure 6. Add diagnosis to Powerchart problem list and Discharge Summary 426.82 – Long QT syndrome (I45.81 in ICD-10) 794.31 – Nonspec Abnormal EKG (R94.31) Suggested “Best Practices” For delirious patient with QTc > 500, consider: • Trazadone • Depakote • Seroquel, Abilify (less QT effect) • Telephone consultation with PES attending Questions? What is normal QT? References “Antiarrhthmic Overview”, Macias, Carlos, Fellow Conference 1/31/12 “Drugs and the QT Interval — Caveat Doctor”, Barbara A. Liu, M.D., and David N. Juurlink, M.D., Ph.D.N Engl J Med 2004; 351:1053-1056 “Oral Erythromycin and the Risk of Sudden Death from Cardiac Causes”, Wayne A. Ray, Ph.D., Katherine T. Murray, M.D., Sarah Meredith, M.B., B.S., Sukumar Suguna Narasimhulu, M.B., B.S., M.P.H., Kathi Hall, M.S., and C. Michael Stein, M.B., Ch.B.N Engl J Med 2004; 351:1089-1096 “Current concepts in the mechanisms and management of drug-induced QT prolongation and torsade de pointes”, Gupta, American Heart Journal, Jue 2007; 153: 891-899 “Drug-Induced Prolongation of the QT Interval”, Dan M. Roden, M.D., N Engl J Med 2004; 350:1013-1022 “Cardiac side effects of psychiatric drugs” Mackin, Human Psychopharmacology 2008; 23: 3-14. “Consensus statement on high-dose antipsychotic medication” Royal College of Psychiatrists, October 2005 “Prevention of Torsade de Pointes in Hospital Settings”, Barbara Drew, et al, JACC Scientific statement, 2010; 55, 9:934-947 “The QT interval: Too long, too short or just right”, Sami Viskin, Heart Rhythm, May 2009,: 6, 5: 711-715