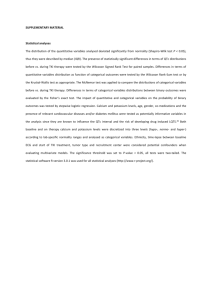
Supplementary Methods:
advertisement

Supplementary Methods: Simulation of Pseudo Transmural-ECGs with a 1D Cable Model: Transmural heterogeneity: The model used interpolated parameters with gradual changes in conductance of INaL and IKs of function of wall depth (Fig.1). This approach produces a more graded APD profile across the 1-D cable than that of a similar model that is constructed from only the three standard cell models. The more typical modeling approach assumes that three stereotyped cells are distributed to three distinct regions of the wall 1-4 . Here, the interpolated model parameters are developed to better match the properties of similar experimental preparation for which the longest APD is found in the deep sub-endocardium on the anterior ventricle wall 5. Note that later characterization showed M-cells localizes to more discrete subdomains termed islands rather the homogenous band that are parallel to the endoand epicardial surfaces 6. Moreover, the islands that may be localized more toward the epicardium than earlier reports suggesting locations closer to the endocardium. While a 1-D cable can not directly represent the island nature of M-cell locations, note the approach here is to match measured properties in canine wedges that presumably reflect spatially averaged response that blurs the more heterogeneous pattern of M-cells. For example, the model conduction velocity and APD distributions (Fig. 2) match experimental data (see Fig. 3 in 7). One feature that is not reproduced in the simulation is the discontinuity in RT and CT in the experimental data. This discontinuity is assumed to correspond to a rotation in the cellular orientation that is reported for the 30% of the wall which is subepicardial. The discontinuity in cellular orientation is not represented in the simulation that is composed to 192 equally spaced point models with equal conductivity between the cells. While INaL and IKs, were interpolated, the changes in Ca-handling parameters were not. That is, the model assumes a factor of two increase in forward and reverse rates of the SERCA pumps for the Epi cells as compared to the other cell types (as originally defined in the Flaim et al. model 8). This increase in SERCA rate is assumed for the range of 70% to 100% of the wall (epicardium). Correction of edge artifacts: An important feature on our modeling approach is to add 48 padding cells to either end of the array to a total length of 288 cells. The two sets of 48 cells are identical in formulation to their adjacent first and last cells in the core 192 cell array that is actually used for the APD and pseudo transmural-ECG calculations. The only difference is a reduction in INaL for shorter APD in the 48 padding cells to achieve APD distributions in the core 192 cells are similar to experimental data. The importance of the padding cells is to remove edge effects that arise in a 1-D array that approximates the transmural heterogeneity in a reasonable but also simplistic way. For example, an actual heart or wedge preparation would have a more complex arrangement of cells in a 3-D anatomical that would blur the abrupt boundary effects at the endo- and epicardial surfaces. However in a 1-D cable abstraction, the initial and final cells are electronically connected to only single neighbor versus two in the rest of the cable. Because of the altered coupling, a propagating wave will increase the APD in the first cells and decrease the APD in the final cells (Fig. 3A-B). With the padding cells the edge effect occurs in the padded regions, and the artifacts are minimized in the core 192 cells (Fig. 3C-D). To our knowledge, similar edge effects have not been reported elsewhere, which suggests our model approach may show higher sensitivity to small changes in repolarizing currents. However, more detailed comparisons would be required to confirm this speculation. While the AP propagates along the whole 288 cell array, only the central 192 cells are used for the analysis. Transmural voltage gradient calculation: The pseudo-transmural-ECG is computed based on the transmural voltage gradient from the epicardial to the endocardial sides of the heart. Under typical patterns of excitation from the endo- to the epicardium, the distribution of AP waveforms strongly depends on the propagation of both depolarization (producing the pseudo transmural Q wave) and repolarization (producing the pseudo transmural T wave). Note that the propagation of the repolarization occurs roughly in the opposite direction to that of depolarization (Fig. 2 bottom panel). That is, repolarization occurs first in the Epi cells and then proceeds towards the M and Endo cells to produce a positive T wave, similar to experimental measures 9. As such, the generation of the positive T wave in pseudo transmural ECG requires the correct sequence of repolarization events in the transmural direction. For example, a transmural ECG for an array of 192 identical cells will produce an inverted T-wave because the repolarization of the cell travels in a left to right direction (Fig 3E). Note that our pseudo transmural ECG results are reported as a difference between epicardial and endocardial electrodes in which the T-wave shows high sensitivity to the repolarization sequence (the reversal of the repolarization direction produces a negative T wave as seen experimentally 10 ). In contrast, most published studies report only a single electrode voltage located near the epicardium (e.g., 2, 3 ). Single electrode measurements produce T- waves that are highly dependent to the electrical activity near the epicardium and are mostly insensitive to the activity near the endocardium. Hence, single electrode measurements are not sensitive to the whole transmural repolarization profile to the same extent as the corresponding two electrode measurements. Supplemental Table 1. Summary of Mutations Mutation M1V A150fs/133 M159sp G168R Y171X Y184S L191fs+90X L191fs/90 R195fs/40 S225L R243C V254M L266P G269S A287fs+59X W305S T312I G314S Y315C A341E A341V A344A/sp S349W S349X P400fs/62 K422fsX10 P448fs/13 R518X Q530X S571fs/20 R591H R594Q D611Y A636fs/28 No. of patients 1 2 4 87 9 14 2 8 2 22 13 118 32 43 1 16 17 19 10 11 24 41 15 9 7 1 11 20 26 3 19 14 10 2 Supplementary Table 2 - Multivariate analysis: Risk factors for cardiac events (syncope, sudden death and aborted cardiac arrest) among all LQT1 patients by combined assessment of patient’s baseline QTc and mutation-specific TRP*Four subgroup of patients were studied: 1) top quartile TRP with QTc ≥ 500 msec; 2) top quartile TRP with QTc < 500 msec; 3) lower quartiles TRP with QTc ≥ 500 msec; 4) lower quartiles TRP with QTc < 500 msec. Lower quartiles TRP with QTc<500 msec was the control group. Parameter Hazard ratio 95% CI TRP: upper quartile (Q4) + QTc ≥ 500 msec 5.04 3.45 – 7.37 TRP: upper quartile (Q4) * QTc < 500 msec 3.13 2.09 – 4.67 TRP lower quartiles (Q13) + QTc ≥ 500 msec 1.97 1.34 – 2.90 TRP lower quartiles (Q13) + QTc < 500 msec 1.00 (Reference) *Multivariate analysis was carried out using Cox proportional hazards regression modelling; all models are further adjusted for gender/age and time-dependent beta-blocker therapy. Supplementary Table 3 - Multivariate analysis: Risk factors for cardiac events (syncope, sudden death and aborted cardiac arrest).* TRP dichotomized at the upper quartile for patients with QTc<500ms Parameter Hazard ratio 95% CI p-value TRP Q4 vs. Q1-3 2.90 1.95 – 4.32 <0.0001 QTc ≥ 450 ms vs. <450ms 1.09 0.71 – 1.671 0.71 Male<13 years old 1.40 0.88 - 2.24 0.16 Female >14 years old 1.87 0.96 – 3.64 0.07 Time dependent β-blocker 0.45 0.22 – 0.95 0.04 *Multivariate analysis was carried out using Cox proportional hazards regression modelling; separate models were developed for parts A and B of the Table, adjusting for the covariates in each part. QTc = QT interval corrected for heart rate; TRP = simulated pseudo-transmural ECG prolongation Supplementary Figure 1 - Conductance INaL and IKs of function of wall depth. The maximal conductance is plotted as function percentage of wall depth for late Na current (INaL, upper trace) and the slow component of the delayed rectifier current (I Ks, lower trace). The upper and lower bounds correspond to the values specified in the FlaimGiles-McCulloch (FGM) reconstruction of the canine cardiac cell 33. The FGM specifies only three standard cell types (Epi, Endo, and M cells). However, 1-D cable model in this study uses a linear interpolation of INaL and IKs that produces a more graded APD profile than that of a similar model constructed from only the three standard cell models in which parameters are changed in step-like manner. A B C Supplementary Figure 2 - Repolarization and depolarization timing profiles of function of wall depth. The simulated APD (A), the activation time (B) and the repolarization times (B) are shown as function of number in the 192 cell 1-D array. The endocardial side is shown the left and epicardial side to the right. The fixed slope of the activation time as function of cell number indicates the conduction velocity is essentially constant. The repolarization time (RT) is APD added to the depolarization time. Similar timing profiles are seen in experiment data 7. Supplementary Figure 3 – Repolarization and depolarization timing profiles as function of wall depth without and with the padding of extra cells. A. The simulated APD for a 192 identical epicardial cell array without extra padding on either end of the array. The effects of electrical coupling and the left to right direction of propagation cause an artifact in that the initial cells have increased APDs and the final cells have decreased APDs. Note that all cells have the exact same ionic current properties so that the observed APD differences emerge from the propagation pattern and not from intrinsic cell differences. For the first cell in the array, the activation travels to the right so that the neighbors to the right will provide a depolarizing current source to prolong the APD, and there is not a cell to the left to be a current sink. For the last cell, the opposite occurs, in that the cell to the left is a current sink that decreases APD, and there is no current source cell to the right. For the central cells, the coupling current to the left is balanced by the coupling current to the right to produce a neutral case with no prolongation. The gradual transition of APDs from the first to the central to the end cells produces the horizontal-S-shaped profile as shown. B. The corresponding repolarization times show similar skewing because of the edge effects. C. The simulated APD for a 192 identical epicardial cell array (shown) with 48 extra identical cells padding either end of the array (not shown). The boundary effects are greatly diminished for the 192 cells and the APD is almost constant as one expects for identical cells. D. Likewise, the corresponding repolarization times show almost no skewing from edge effects. E. The corresponding transmural ECG is shown for 192 identical epicardial cell array. Because the repolarization of the cells travels in a left to right direction, the T-wave is inverted (the presence of different cell types in the normal case, causes repolarization to travel from right to left). Supplementary Figure 4: Rate of cardiac event during follow up. Cumulative probability of the first cardiac event (syncope, aborted cardiac arest or death) during follow up dichotomized by patients with each of the quartile TRP (Q1-Q4). A B Supplementary figure 5: Mean mutation-specific QTc correlation to individual patient QTc and TRP. (A) Correlation of individual QTc determined for all subjects included in the study and the mean QTc obtained as an average of all QTc for patients with each mutation. (B) Correlation of the mean QTc obtained as an average of all QTc for patients with the same mutation with TRP determined from simulation. Data is plotted as mean ± standard deviation of the mean. Note that for most mutations average mean QTc values are not significantly different. Supplementary figure 6: Variability of individual patient QTc. Each data point represents QTc obtained for individual patients at different times (age indicated). Mutation for each patient is indicated. Reference List (1) Brennan T.P., Fink M., Stokeley D., Rodriguez B., Tarassenk L. Modelling Effects of Sotalol on Twave Morphology 1988. Computers in Cardiology 2007;249-52. (2) Narayan SM, Bayer JD, Lalani G, Trayanova NA. Action potential dynamics explain arrhythmic vulnerability in human heart failure: a clinical and modeling study implicating abnormal calcium handling. J Am Coll Cardiol 2008 November 25;52(22):1782-92. (3) Weiss DL, Seemann G, Keller DUJ, Farina D, Sache FB, Dossel O. Modeling of heterogeneous electrophysiology in the human heart with respect to ECG genesis 5. 2007 p. 49-52. (4) Viswanathan PC, Rudy Y. Cellular arrhythmogenic effects of congenital and acquired long-QT syndrome in the heterogeneous myocardium. Circulation 2000 March 14;101(10):1192-8. (5) Yan GX, Antzelevitch C. Cellular basis for the normal T wave and the electrocardiographic manifestations of the long-QT syndrome. Circulation 1998 November 3;98(18):1928-36. (6) Akar FG, Yan GX, Antzelevitch C, Rosenbaum DS. Unique topographical distribution of M cells underlies reentrant mechanism of torsade de pointes in the long-QT syndrome. Circulation 2002 March 12;105(10):1247-53. (7) Yan GX, Shimizu W, Antzelevitch C. Characteristics and distribution of M cells in arterially perfused canine left ventricular wedge preparations. Circulation 1998 November 3;98(18):19217. (8) Flaim SN, Giles WR, McCulloch AD. Arrhythmogenic consequences of Na+ channel mutations in the transmurally heterogeneous mammalian left ventricle: analysis of the I1768V SCN5A mutation. Heart Rhythm 2007 June;4(6):768-78. (9) Yan GX, Antzelevitch C. Cellular basis for the normal T wave and the electrocardiographic manifestations of the long-QT syndrome. Circulation 1998 November 3;98(18):1928-36. (10) Zhu TG, Patel C, Martin S, Quan X, Wu Y, Burke JF, Chernick M, Kowey PR, Yan GX. Ventricular transmural repolarization sequence: its relationship with ventricular relaxation and role in ventricular diastolic function. Eur Heart J 2009 February;30(3):372-80.