Best Practices in Communication and Resolution Programs
advertisement

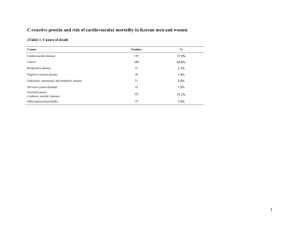
Best Practices in Communication and Resolution Programs Thomas H. Gallagher, MD Professor of Medicine, Bioethics & Humanities Director, UW Medicine Center for Scholarship in Patient Care Quality & Safety Director, Program in Hospital Medicine University of Washington Change Readiness Assessment Investigation and Process Improvement Resolution Gap Analysis Reporting Communication Caring for the Caregiver AHRQ CRP Toolkit Content: Modules • Change Readiness Assessment • Gap Analysis • Incident Reporting • Investigation and Process Improvement • Communication • Caring for the Caregiver • Measurement and Evaluation 3 Example: HealthPact DRP Study Event (SE) • Care team responds to immediate patient needs and provides information then known • Involved staff reports SE to Risk Manager Study Event (SE) Action by Facility Risk Manager • Initiates QI investigation using Just Culture approach • Initiates support services for patient/family • Initiates disclosure coaching and other support services for healthcare team • Contacts other Partners to explain SE and steps taken and initiates collaboration Physicians Insurance Study Event (SE) Action by Facility Risk Manager Facility Insurer Other Insurer Partners collaborate on approach to evaluation and resolution Physicians Insurance Study Event (SE) Action by Facility Risk Manager Facility Insurer Other Insurer Expedited Care Assessment and Review of Event (CARE) Partners and involved providers decide on effective approach and timeline for CARE, including internal and/or external expert review to determine: • Whether care was reasonable • Whether system improvements are needed to prevent recurrence • Whether other actions are warranted Physicians Insurance Study Event (SE) Action by Facility Risk Manager Facility Insurer Other Insurer Expedited Care Assessment and Review of Event (CARE) Joint Approach to Resolution Partners agree on approach to resolution: • What are the patient’s/family’s needs? • Will monetary compensation or other remedies be offered? • What will be disclosed to patient/family? • How will identified system improvements be pursued? Physicians Insurance Study Event (SE) Action by Facility Risk Manager Facility Insurer Other Insurer Expedited Care Assessment and Review of Event (CARE) Joint Approach to Resolution Patient/family is notified of findings and approach to resolution: • Full explanation of what happened • Apology as appropriate • Offer of compensation and/or other remedies, or explanation of why no offer is being made • Information about any safety improvements Patient/Family Communication Importance of having a “Just Culture” Epistemological Problems • The plural of “anecdote” is not “data” • Time-horizon problem • Small-numbers problem • Potential confounding, especially regarding safety improvement • Variations in program design and implementation across sites University of Michigan Health System (Pre/post analysis, 1995-2000 vs. 2001-2007) • Average monthly rate of new claims: 7.03 4.52 per 100,000 patient encounters (p<0.05) • Average monthly rate of new lawsuits: 2.13 0.75 (p<0.01) • Average rate of claims not resulting in lawsuit: No sig. change • Median time from claim reporting to resolution: 1.36 0.95 years (p<0.01) Source: Kachalia et al., Ann Intern Med 2010 University of Michigan, continued • Liability costs (mean and median) decreased significantly • Patient compensation costs decreased significantly for lawsuits and overall • Average payout per lawsuit: $405,921 vs. $228,208 (p<0.01) • Costs did not change significantly for non-lawsuit claims • Legal expenses decreased significantly overall (p<0.01) • Compare: in 2001-2007, other Michigan insurers had: • Lower proportion of paid claims (24% vs. 43%) • Increasing legal costs • Flat compensation costs Source: Kachalia et al., Ann Intern Med 2010 Seven Pillars Program • University of Illinois Chicago reports: • Increase in patient safety event reporting from 1,500 to 7,500 per year • 50% reduction in new claims • Reduction in median time to resolution from 55 to 12 months Source: UIC communication to AHRQ, 2012. PEARL Program • Stanford University Medical Indemnity and Trust reports: • 36% drop in claim frequency in first 3 ½ years of program compared with 2 previous years • $3.2 million (32%) average annual reduction in premiums paid for the retained layer of losses (the largest component of total premiums) Source: Independent actuary’s analysis of 2007-2007 data on 50 PEARL cases, reported in Institute for Healthcare Improvement, Respectful Management of Serious Clinical Adverse Events (2011). Implementation Experiences • Washington • New York • Massachusetts Meeting Stakeholders Where They Are • Fears and concerns of different stakeholders • Vary considerably • May not be explicitly articulated • Potential of catastrophic outcome can loom large • Reflect past and current challenges with dysfunctional liability system • Form a semi-coherent narrative for that stakeholder about how world works • Most stakeholders recognize current system is highly dysfunctional and desire change • But worry that things could get worse not better Prepare for “We Already Do This” • Most organizations consider themselves principled • Selective use of CRP concept is the norm • Organization can point to individual case(s) where they used CRP approach • Cases in which CRP approach not used in organization’s mind reflect problem with case itself, not their application of CRP concept • Gentle use of hypothetical cases can help uncover situations in which institution not currently using CRP approach Passive Resistance • Who isn’t in favor of telling patients the truth and compensating them when a serious error has harmed them? • Need to make it easy for concerned stakeholders to share their fears • Passive resistance usually emerges late, as implementation is just starting Bandwidth • Assume all key CandOR implementers are at 120% capacity with current responsibilities • Acknowledge that CandOR will involve additional work • Provide new FTE • If you are adding to individual’s current responsibilities, need to subtract • Ensure that CandOR makes it easier for folks to accomplish existing workload Lessons from the Field • It’s not business as usual • CandOR is quality/safety program, not risk management initiative • Local adaptation is key • Multiple, visible champions • CandOR will rise/fall around clinician engagement More Lessons • Bandwidth challenges must be addressed directly • Culture change is slow, painstaking process • Some, not all, results will be felt immediately • Don’t let difficulty of culture change become excuse for incomplete implementation • Process must be trustworthy • Metrics can help drive implementation • Needs to be principled approach • Especially for those cases that are hard, embarrassing, patient is unaware of CRP Certification Pilot Major CRP Challenge: Provider Fear of Reporting • Providers worry that reporting unanticipated outcome may lead to punitive consequences from institution, regulators • Mandatory reporting to Medical Quality Assurance Commission required when patient receives compensation >$20K in response to medical error • Providing fast, fair financial resolution to patients when care was not reasonable is central tenet of CRP process • Absence of event reporting by providers preventing analysis, learning Most Adverse Events Are Not Caused By Incompetent Providers • Oftentimes, adverse events happen despite high quality care • When adverse events are associated with care that was not reasonable, usually involve competent provider caught in system failure or who made simple human error CRP Certification Goals • Promote learning through early adverse event reporting by providers to their institution/insurer, comprehensive event analysis, and implementation of prevention plans • Enhance patient-centered accountability Stakeholders Involved in CRP Certification Design, Operation • MQAC • Institutions participating in CRP • Physicians Insurance • WSMA, WSHA, FHQC, HealthPact Leadership Group (includes patient advocates, attorneys) What Does the Ideal CRP Event Look Like? • Early event reporting by provider • Careful analysis by institution-was unanticipated outcome caused by medical error? If so, how can recurrences be prevented? • Prompt, compassionate disclosure to patient • Fast, fair resolution for patient • Learning at individual and institutional level CRP Certification Basics • Important exclusions: Gross provider negligence, provider impairment, boundary violations • Certification process based at Foundation for Healthcare Quality • MQAC retains all current authority. • All mandatory reporting requirements remain in effect • Responsibility of institution, insurer • Process is voluntary, open to all Washington physicians • Aiming over time towards integration of other regulatory bodies (NCQAC, , WBP, DOH, other Boards) • CRP Certification group will not perform independent investigations CRP Certification Review • Case reviewed by multi-disciplinary group including patient advocate, risk/claims specialists, attorneys, physician leaders, individual with regulatory experience. • Reviewers can not be affiliated with institution where event occurred • Review addresses whether key elements of CRP were met • Institutions/insurers can resolve CRP deficiencies and resubmit Taking the Next Step: Key Questions for Organizations • What’s motivating you to do this? • Will your insurer be fully on board with the philosophy of the program? • Will your organization’s culture support full disclosure and routine, timely reporting? • Is top leadership at the facility and insurer willing to visibly champion and directly engage in the program? • Can you afford to invest additional resources, knowing the payoff may not come for a few years? Taking the Next Step: Key Questions for Policymakers • Does the state have adequate legal protection for apologies? • How about a prelitigation notice law? • Are the reputation and philosophy of the state licensing agencies compatible with the CRP? • How can families be connected with high-quality legal representation at reasonable cost? Thank you! Questions and comments?