Nashita Patel
advertisement
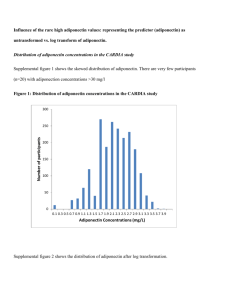
* Dr. Nashita Patel On behalf of the UPBEAT Consortium Clinical Research Fellow to Professor Lucilla Poston * * Long term risk • T2DM • Maternal and childhood obesity • Abnormal offspring glucose homeostasis Neonatal • SGA/LGA • >NICU admission • Birth injuries Obstetric • Infection • > CS • PPH • VTE Maternal • PET • PIH • GDM * Strong association between maternal BMI and healthcare costs Mean costs 23% higher among overweight women Mean costs 37% higher among obese women UK: normal weight £3546; overweight £4244; obese £4717 * * * * Re the IOM GUIDELINES * ‘The recommendations were not validated by intervention studies. Without evidence from large-scale trials, it is not clear whether or not adhering to the recommended ranges lowers the risk of adverse outcomes for mothers and their babies.’ * Background Adipose tissue Leptin IL-2, IL-12, IFN-γ Adiponectin TNF-α, IL-6 GDM Glucose, Lipids, insulin Macrosomia IL-4, IL-5, IL-10, IL-13 Fetal hypothalamus Fetal Metabolic memory IL-2, IL-12, IFN-γ Fetal hypothalamic neuro-peptides Offspring obesity Offspring insulin resistance * 20 PNS 15 P=0.04 10 5 0 Upper arm Subscapular Biceps skin circ skin fold fold Total fat 2 year old Children of Diabetic Women Treated with Metformin Metformin Have Higher Skin Folds Thickness than Insulin Children of Mothers Treated with Insulin * LIMIT trial; Dodd et al (BMJ 2014) • The first lifestyle RCT powered for clinical outcomes • 2152 Overweight and obese women • Primary outcome: LGA Results: • No significant difference in primary outcome • Significant reduction (20%) in BW>4kg • No reduction in GWG * IG POP study • Pilot trial of a slow digesting low GI supplement on blood glucose during an obese pregnancy • Inform the design of a nutritional intervention RCT of dietary advice with LGI supplement in an obese pregnancy * 1. Significant reduction in post prandial glycaemia at breakfast & dinner 2. Significant reduction in overall daytime glucose vs. control and habitual diet 3. Significant reduction in nocturnal glucose vs. habitual diet *Complex intervention in 1546 obese women *Diet; Low Glycemic load, reduce saturated fat and free sugars *Exercise; Mild to moderate exercise *Primary Outcome: * Maternal: OGTT 28 weeks. (IADPSG criteria) * Neonatal; Delivery of Large for Gestational Age infant * (LGA >90th Customised Centile ) *Secondary Outcomes: * Childhood adiposity at 6mths and 3 years Recruitment BMI >30kg/m2 Randomisation 15+0-17+6 weeks’ gestation All women Baseline Physical Activity (PA), Diet Intervention arm 1:1 Health Trainer Interview Handbook Exercise DVD 8 weekly sessions (SMART goals) 28 weeks’ gestation OGTT, PA, Diet 36 weeks’ gestation PA, Diet Pregnancy outcome 18 Childhood follow up PILOT (183 Obese Pregnant Women) Influence of Intervention on Diet (Poston et al, BMC Pregnancy Childbirth 2013) Control Total Energy Intake (MJ/d) Dietary Glycemic Load (g/d) Total fat (%E) Saturated FA (%E) Intervention Baseline 7.53 (2.2) 7.26 (2.29) 28 weeks 7.71 (2.30) 6.75(2.57) Baseline 133 (48) 129 (41) 28 weeks 146 (55) 111 (39) Baseline 36.0(8.2) 34.9(9.3) 28weeks 35.9(7.7) 32.5 (7.4) Baseline 12.7 (3.9) 28weeks 12.9 (3.9) Difference (95% CI) -0.94 (-1.72 to -0.18) p 0.016 −33 (−47 to −20) <0.001 −3.2 (−5.6 to −0.8) 0.010 −1.6 (−2.8 to −0.3) 0.015 12.0 (4.3) 11.1 (3.8) PILOT Influence of Intervention on Dietary Patterns Control Intervention p Western Diet Score 0.42 (-0.49 to 1.47) -0.40 (-1.13 to 0.58) 0.001 Meat and Rice Diet Score 0.10 (-0.74 to 0.59) -0.10 (-0.78 to 0.29) 0.497 Healthyunhealthy choices diet score 0.50 (-0.62 to 1.42) -0.47 (-1.51 to 0.37) <0.001 PILOT Influence of Intervention on Plasma Cholesterol Control Control Intervention 7 Intervention 4 3.5 LDL (mmol/L) Cholesterol (mmol/L) 6.5 6 3 5.5 2.5 5 15-17+6 27-28+6 34-36+6 Gestational age 15-17+6 27-28+6 34-36+6 Gestational age PILOT Assessment of physical activity 1. Using accelerometer 2. RPAQ self report questionnaire NO change Minor increase as reported by questionnaire PILOT Only intervene in obese women at risk of GDM? PILOT Prediction of GDM at 15-18 weeks’ gestation in obese women; a preliminary study Significant clinical variables: age, parity, ethnicity, BP, triceps & sum of skinfolds Clinical risk factors alone AUC=0.7955 basic model + Adiponectin AUC= 0.8571 Basic model + Adiponectin + AST (aspartate aminotransferase) AUC=0.8660 Maitland et al, Diabetic Medicine 2014; 8:963 PILOT Microalbuminuria as a predictor of GDM in obese pregnant women? UPBEAT pilot trial. Clinical risk factors alone Clinical risk factors alone + ACR * Summer 2014: Recruitment target reached (n=1556) End November 2014: All maternal and neonatal outcome data available January 2015: UPBEAT MAIN TRIAL RESULTS *