Ventilator Modes of Operation

ENTC 4350
Modern Ventilators
Modern Ventillators
Ventilation assistance is provided under either of two conditions:
(1) breathing initiated by a timing mechanism or
(2) patient-initiated breathing.
Automatically timed breathing is usually provided for patients who cannot breathe on their own.
•
It provides inspiration and expiration at fixed rates and durations except for periodic sigh; a sigh is a rest period for the patient.
Patient-initiated breathing may be given to one who has difficulty breathing due to high airway resistance.
•
The patient’s effort to inhale triggers the respirator unit to deliver air at the positive pressure prescribed.
Ventilator Modes of Operation
The following definitions are commonly used to describe respirator/ventilator operation:
•
CMV Continuous mandatory ventilation: Once initiated by either the ventilator operator or the patient, the breath is driven to the patient.
•
CPAP Continuous positive airway pressure: Breaths are spontaneous, unless the operator intervenes. The spontaneous breaths are determined entirely by patient effort.
However, the air/oxygen mixture is set by the ventilator.
SIMV
PEEP
Synchronized intermittent mandatory ventilation: These breaths are initiated by either the machine, the operator, or the patient. The breaths may be either spontaneous or mandatory. That is, if the patient does not breathe within a preset time period, the ventilator will deliver a breath.
Positive end-expiratory pressure: The pressure maintained by the ventilator that the patient must exhale against.
•
Apena The patient has stopped breathing.
•
Sigh A breath delivered by the ventilator that differs in duration and pressure from a nominal breath.
•
Nebulizer A device for producing a fine spray of liquid or medication into the patient’s air.
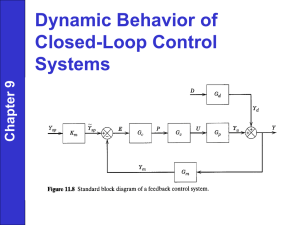
The block diagram shows the external flexible tubing and the ventilator unit.
Air from the ventilator during patient inspiration passes through a bacterial filter and humidifier.
•
A nebulizer may spray medication into the air.
This air then forces valve 1 up to close off the spirometer and deliver air to the patient.
After the inspiration air is turned off by the ventilator, valve 1 drops and the patient exhales into the bellows, which has its outlet valve held closed pneumatically by the ventilator unit.
•
During the subsequent patient inspiration cycle, that valve will open, causing the bellows to fall and empty.
During patient expiration, the direction of the air in the pneumatic system is determined by the main solenoid, which is switched appropriately by the system electronics.
•
Room air is drawn from the air inlet filter by the main compressor and is directed through the main solenoid to hold closed the upper outlet valve of the bellows located inside the unit.
Next, the weight of the bellows causes the bottom bellows chamber outlet valve to open, as the main solenoid directs air to close the inlet bellows chamber valve.
•
The weight of the falling bellows draws oxygen-enriched air into it in preparation for the patient-inspiration part of the cycle.
The oxygen content of the air flowing into the bellows is controlled by a percentage control valve, which regulates the resistance to room air and oxygen appropriately.
At the end of patient expiration, the system electronics trip the main solenoid, thereby initiating the patientinspiration part of he cycle.
During patient inspiration, the compressor draws room air through an air filter and then through the main solenoid.
•
It forces the bottom inlet valve of the internal bellows chamber open and forces the bottom bellows chamber outlet valve closed.
The high pressure in the bellows chamber compresses the bellows, forcing open the upper outlet valve set free by the main solenoid.
•
This allows the oxygen-enriched air to pass through the main bacteria filter into the external tubes and then to the patient lungs.
A sensitivity control monitors the negative pressure necessary to initiate inspiration when the respirator is used in the patient-initiated breathing mode called the assist mode.
•
A nebulizer compressor may draw air from the bellows and force it through an aspirator to mix medication into the patient-inspired air.
•
When inspiration is complete, the main solenoid switches the direction of the pneumatic air to repeat the expiration cycle, and so on.
The black bag at the end of the tubing simulates a compliant lung.
•
This respirator may be operated using compressed air from the hospital air supply.
In that mode, the ventilator can be removed from its internal compressor, thereby decreasing it in size; turning off the compressor also reduces problems in instrument noise control.
To aid patient respiration, hospital air and oxygen enter the pneumatic compartment, where it is filtered.
•
A check valve reduces the pressure to a nominal 10 psi.
A proportional solenoid valve assembly allows the air/oxygen mix to be controlled by the system electronics.
•
A check valve directs air to the patient during the inspiration cycle.
During the
subsequent expiration phase, the system electronics opens the check valve, CV5, to provide a vent for the patient exhalation air.
•
In this case, the pneumatically operated valves of older ventilators have been replaced by valves controlled with microprocessorbased electronics.
A small positive-pressure ventilator is illustrated with both front and back views.
PNEUMOTACHOGRAPH AIRFLOW
MEASUREMENT
Patient airflow may be measured by changes in resistance of a thermistor in the airstream due to the cooling effect of flowing air.
•
But it must be calibrated to compensate for changing ambient temperature.
To eliminate this disadvantage, a strain-gauge wire mesh is often used.
The airflow in either direction puts a strain on the screen and changes the resistance of its strain gauge.
The strain gauge is a component of a
Wheatstone bridge.
Here the change in resistance,
D
R , is proportional to the airflow, F, past the wire mesh.
F
k
D
R
V
A
V
BB
V
B
V
BB
R
R
R
D
R
R
2 R
Voltage divider rule
V
AB
V
A
V
A
R
R
D
R
R
R
2 R
V
BB
Getting a common denominator
V
AB
2 R
2 R
R
2 R
D
R
2 R
D
R
2 R
D
R
R
2 R
V
BB
V
AB
4 R
2
2 R
2
2 R
D
R
4
2 R
2
R
2
R
D
R
2 R
D
R
V
BB
V
AB
D
R
4 R
2
D
R
V
BB
If R »
D
R
V
AB
R
4 R
V
BB
For the diff amplifier with a gain of A
D
,
V
F
A
D
V
BB
D
R
4 R
A
D
V
BB
F
4 kR for
D
R
F k
Integrator Circuit
For the integrator circuit,
V out
1
C t
0 t i
C dt
C
1
t t
0 v in
R dt
V out
1
RC
t t
0
A
D
V
BB
D
R dt
4 R
Note that the term inside the integral is a constant,
V out
A
D
V
BB
D
R
4 R
2
C t
0 t dt
A
D
V
BB
4 R
2
D
R
C t
kt
Pneumotachograph Volume
Measurement
A volume exhaled by a patient is measured with the pneumotachograph by first closing and then opening the reset switch.
•
This sets the initial charge on the capacitor to zero and fixes V out at zero.
The patient is then asked to exhale through the pneumotach mouthpiece.
•
The resulting change in
D
R creates a voltage V
F as a function of time in proportion to flow.
The air volume expired by the patient, beginning at t = 0, when the reset is activated, equals the area under the flow vs. time curve.
•
Mathematically, this area is computed by integration.
The output voltage, V out
,is proportional to the volume of air expired from time t =
0 to the time, t, desired.
•
The flow, F, is a function of time that may increase, decrease, or stay constant, so long as it goes in one direction.
V out
1
RC
t t
0
A
D
V
BB
F dt
4 kR
V out
A
D
V
BB
4 kRR
1
C
t t
0
F dt
t t
0
F dt
Total lung volum e
VOL
V o u t
A
D
V
BB
4 kRR
1
C
VOL
k
VOL
This implies that V out is proportional to the total volume of air that is passed through the pneumotach for the time of observation
.
THE PLETHYSMOGRAPH
The pneumotachograph can be used to measure the rate of airflow during respiration and the vital air capacity of the lung VC .
•
It cannot, however, measure the total lung capacity, TLC.
The reason for this is that the pneumotachograph can only measure the amount of air a person can exchange in respiration, and cannot detect the residual volume of air, RV, left in the lung after a forced exhaling.
•
To measure the TLC, a body plethysmograph may be used.
The plethysmograph consists of an airtight chamber the patient can enter and sit in.
The principle of operation of the plethysmograph depends directly on the gas law for an ideal gas of volume V and pressure
P, namely Boyle’s Law
PV
k
1
T
•
where k
1 is a constant and T is the absolute temperature (K). In the chamber, the temperature remains constant.
To measure TLC, the patient enters the chamber.
•
The door is sealed, and the valve on the mouthpiece is closed.
Since the patient cannot breathe with the valve closed, the air pressure in the mouthpiece equals that in the lung, P
T
.
•
That is, when the flow of air is zero, the pressure drop from mouthpiece to lung is also zero.
With the valve closed, a formula for the thoracic volume is derived as follows.
•
The gas equation for constant temperature holds inside the lung dP dV
P
V
Using the previous equation, the TLC can be written as: dTLC dP
T
TLC
P
T
Boyle’s Law also holds in the chamber, so that dVol
C dP
C
Vol
C
P
C
•
Here VOL
C is the chamber volume and P
C the chamber pressure.
is
Because the chamber is closed, any increase in the thoracic volume introduced by breathing motions causes a decrease in the chamber volume of air.
•
That is dVol
C
dTLC
Combining the equations dTLC dP
T
TLC
P
T dVol
C dP
C
Vol
C
P
C
• with the previous fact: dVol
C
dTLC
This yields: dVol
C
Vol
C
P
C dP
C
dTLC
TLC
P
T dP
T
TLC dP
T
P
T
Vol
C
P
C dP
C
During the test P
T
= P
C approximately, since the changes in pressure induced by breathing motions are small when the patient is resting.
•
Thus,
TLC
Vol
C dP
C dP
T
This equation gives the means for measuring the lung volume, TLC, by the following steps:
1. Close the mouthpiece valve on the patient sealed in the chamber.
2. Ask the patient to make breathing motions.
3. Read the change in pressure dP
T on meter 1.
4. Read the change in pressure dP
C on meter 2.
in the chamber
5. Since the chamber volume VOL
C is a known specification of the plethysmograph, use the result in steps 3 and 4 to compute TLC.