Hemodynamics, Blood pressure and
advertisement

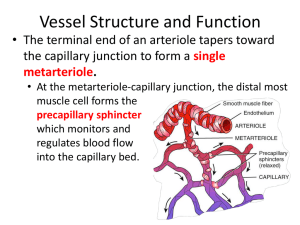
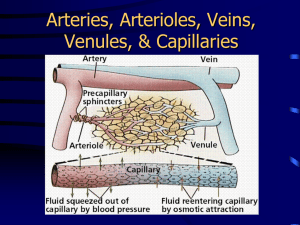
Hemodynamics, Blood pressure and Microcirculation Dr. Meg-angela Christi Amores The Circulation • Functions: – to transport nutrients to the body tissues – to transport waste products away – to conduct hormones from one part of the body to another – rate of blood flow through most tissues is controlled in response to tissue need for nutrients Physical Characteristics • Arteries • transport blood under high pressure to the tissues • have strong vascular walls, high blood flow rate • Arterioles • last small branches of the arterial system • act as control conduits through which blood is released into the capillaries • capability of vastly altering blood flow in each tissue bed in response to the need of the tissue Physical Characteristics • Capillaries • exchange fluid, nutrients, electrolytes, hormones, and other substances between the blood and the interstitial fluid • very thin and have numerous minute capillary pores permeable to water • Venules • collect blood from the capillaries, and they gradually coalesce into progressively larger veins • Veins • conduits for transport of blood from the venules back to the heart • Thin walled, muscular enough to expand or contract The circulation • If all the systemic vessels of each type were put side by side, their approximate total cross-sectional areas for the average human being would be as follows: Vessel Cross-sectional area (cm2) Aorta 2.5 Small arteries 20 Arterioles 40 Capillaries 2500 Venules 250 Small veins 80 Venae cavae 8 • Note larger cross sectional area of veins than arteries, explains large storage of blood in the venous system • velocity of blood flow is inversely proportional to vascular cross-sectional area • velocity averages about 33 cm/sec in the aorta but only 1/1000 as rapidly in the capillaries, about 0.3 mm/sec Basic theory of Circulatory Function 1. The rate of blood flow to each tissue of the body is almost always precisely controlled in relation to the tissue need 2. The cardiac output is controlled mainly by the sum of all the local tissue flows 3. In general the arterial pressure is controlled independently of either local blood flow control or cardiac output control. • Blood flow - the quantity of blood that passes a given point in the circulation in a given period of time – expressed in milliliters per minute or liters per minute • overall blood flow in the total circulation of an adult person at rest is about 5000 ml/min Factors affecting blood flow • pressure difference of the blood between the two ends of the vessel – pressure gradient • the force that pushes the blood through the vessel • the impediment to blood flow through the vessel – vascular resistance • Ohm’s law: – blood flow is directly proportional to the pressure difference but inversely proportional to the resistance • Ohm’s Law: F= P R F – blood flow P – pressure difference R - resistance Laminar vs. Turbulent blood flow • Laminar flow – blood flows at a steady rate through a long, smooth blood vessel – flows in streamlines – each layer of blood remaining the same distance from the vessel wall – the central most portion of the blood stays in the center of the vessel Laminar vs. Turbulent blood flow • Turbulent flow – blood flowing in all directions in the vessel and continually mixing within the vessel – When the rate of blood flow becomes too great – when it passes by an obstruction in a vessel – when it makes a sharp turn – when it passes over a rough surface – Increased resistance to blood flow Laminar vs. Turbulent blood flow Resistance to blood flow • Resistance - the impediment to blood flow in a vessel, but it cannot be measured by any direct means • Conductance - measure of the blood flow through a vessel for a given pressure difference – Slight changes in the diameter of a vessel cause tremendous changes in conductance Conductance = Diameter4 Resistance to blood flow • Poiseuille’s Law – the rate of blood flow is directly proportional to the fourth power of the radius of the vessel – the diameter of a blood vessel (which is equal to twice the radius) plays by far the greatest role of all factors in determining the rate of blood flow through a vessel F= π Pr4 8ήl • In large diameter vessels, with laminar flow, the velocity is different in concentric rings • the blood that is near the wall of the vessel flows extremely slowly, whereas that in the middle of the vessel flows extremely rapidly Effects of pressure • Increase in arterial pressure: • increases the force that pushes blood through the vessels • distends the vessels at the same time, which decreases vascular resistance Vascular Distensibility • all blood vessels are distensible • the distensible nature of the arteries allows them to accommodate the pulsatile output of the heart and to average out the pressure pulsations • most distensible by far of all the vessels are the veins, providing a reservoir function for storing large quantities of extra blood Arterial Pulse Pulsations • Because of vascular distensibility, blood flow is continuous, with systole and diastole • Blood does not flow instantaneously in the peripheral circulation all at once • Pressure pulsations: – Systolic pressure – 120mmHg – pressure at top of each pulse – Diastolic pressure - 80mmHg – at the lowest point of each pulse – Pulse pressure – difference between SP and DP Methods in determining BP • Direct method: – direct catheter measurement from inside the arteries – Most accurate – impractical Methods in determining BP • Auscultatory method – Stethoscope over antecubital area – BP cuff inflated over upper arm – Korotkoff sounds – Mechanism: • When cuff pressure is higher than systolic P, brachial artery remains occluded • As cuff pressure is reduced, blood jets through the artery, hearing tapping sounds from antecubital artery • When cuff pressure is equal diastolic pressure, blood no longer jets through squeezed artery, tapping stops • To be continued..... – Next topic: Control of BP Nervous control of BP • Autonomic nervous system – Sympathetic NS – most important regulator – Leave SC through Thoracic and L1 and L2 spinal nerves – To the sympathetic chain – Innervates all vessels except capillaries, precapillary sphincters and metarterioles – capability to cause rapid increases in arterial pressure Nervous control of BP • 3 major changes: – Almost all arterioles of the systemic circulation are constricted – The veins especially (but the other large vessels of the circulation as well) are strongly constricted. – Finally, the heart itself is directly stimulated by the autonomic nervous system, further enhancing cardiac pumping Nervous control of BP • the most rapid of all our mechanisms for pressure control • often increasing the pressure to two times normal within 5 to 10 seconds Nervous control • During exercise – motor areas of the brain become activated to cause exercise, most of the reticular activating system of the brain stem is also activated – increased stimulation of the vasoconstrictor and cardioacceleratory areas of the vasomotor center • During stress – In extreme fright, the arterial pressure sometimes rises to as high as double – Called alarm reaction Reflex mechanisms for maintaining normal BP • Autonomic nervous system • Mostly Negative feedback reflex mechanisms • Baroreceptor Reflexes • • • • Initiated by stretch receptors in large systemic arteries Inc arterial pressure stretches baroreceptors Sends signals to CNS Negative feedback signals are sent back Baroreceptor reflex • Locations: – Internal Carotid artery bifurcation – carotid sinus – Wall of Aortic Arch – Signals enter tractus solitarius of the medulla – Inhibit vasomotor center and excite vagal parasympathetic center – Effects: vasodilatation of arteries and veins decreased heartrate and heart contraction Baroreceptor reflex • During changes in posture – Upon standing, arterial pressure in head falls, causing loss of consciousness – Prevented by the reflex, causing strong sympathetic discharge throughout the body Long term control of BP • Which organ regulates arterial pressure in the long term? Renal-Body Fluid System for Arterial Pressure Control • two primary determinants – The degree of pressure shift of the renal output curve for water and salt – The level of the water and salt intake line • Role of NaCl – When there is excess salt in the extracellular fluid, the osmolality of the fluid increases stimulates the thirst center in the brain – stimulates the hypothalamic-posterior pituitary gland secretory mechanism to secrete increased quantities of antidiuretic hormone MICROCIRCULATION MICROCIRCULATION • Where the most purposeful function of the circulation occurs • transport of nutrients to the tissues and removal of cell excreta • CAPILLARIES – walls of the capillaries are extremely thin, constructed of single-layer, highly permeable endothelial cells Microcirculation • 10 billion capillaries with a total surface area estimated to be 500 to 700 square meters (about one-eighth the surface area of a football field) • Nutrient artery – arterioles – metarteriole – precapillary sphincter - capillaries Flow of blood through capillaries • Intermittent – turning on and off every few seconds • Phenomenon of VASOMOTION – intermittent contraction of metarterioles and sphincter • Physiologic significance: – most important factor found thus far to affect the degree of opening and closing of the metarterioles and precapillary sphincters is the concentration of oxygen in the tissue. Transcapillary movement • Diffusion • Lipid-Soluble Substances Can Diffuse Directly Through the Cell Membranes of the Capillary Endothelium • Water-Soluble, Non-Lipid-Soluble Substances Diffuse Only Through Intercellular "Pores" in the Capillary Membrane. Transcapillary movement • Effect of Molecular Size on Passage Through the Pores • width of the capillary intercellular cleft-pores, 6 to 7 nanometers, is about 20 times the diameter of the water molecule, which is the smallest molecule that normally passes through the capillary pores • Effect of Concentration Difference on Net Rate of Diffusion Through the Capillary Membrane. EDEMA Lymphatics • What is lymph? – derived from interstitial fluid that flows into the lymphatics – protein concentration in the interstitial fluid of most tissues averages about 2 g/dl – protein concentration in the interstitial fluid of most tissues averages about 2 g/dl, – lymph formed in the intestines has a protein concentration as high as 3 to 4 g/dl • Most of the fluid filtering from the arterial ends of blood capillaries flows among the cells and finally is reabsorbed back into the venous ends of the blood capillaries; but on the average, about 1/10 of the fluid instead enters the lymphatic capillaries and returns to the blood through the lymphatic system rather than through the venous capillaries. Lymphatics • one of the major routes for absorption of nutrients from the gastrointestinal tract, especially for absorption of virtually all fats in food • special lymph channels that drain excess fluid directly from the interstitial spaces • all the lymph vessels from the lower part of the body eventually empty into the thoracic duct • total quantity of all this lymph is normally only 2 to 3 liters each day.