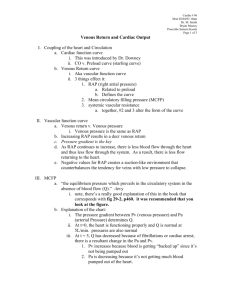
Cardiac Physiology – Control of Cardiac Output
advertisement

Cardiac Physiology – Control of Cardiac Output Factors Controlling CO Four factors control CO; heart rate, myocardial contractility, preload, and afterload. Heart rate and contractility are intrinsic factors, characteristics of cardiac tissues, influenced by neural and humoral mechanisms. Preload and afterload depend on the characteristics of both the heart and the vascular system. Preload and CO relationships can be described in two curves: cardiac function curve and vascular function curve. The cardiac function curve is a characteristic of the heart and is an expression of the Frank-Starling relationship The vascular function curve defines the dependence of the central venous pressure on the CO. The Vascular Function Curve Relates Central Venous Pressure to CO The vascular function curve defines the changes in central venous pressure evoked by changes in CO (CVP is the dependant variable and CO is the independent variable). In contrast, with the cardiac function curve the CVP is the independent variable and the CO is the dependent variable. How to Derive the Vascular Function Curve Assume that the entire heart is a single pump. The high resistance microcirculation is the peripheral resistance (20 mmHg/L/min). Systen compliance is subdivided into the arterial compliance (Ca) and the venous compliance (Cv). Assume that the venous compliance is about 19 times greater than the arterial compliance. Assume Pa = 102 and Pv = 2 mmHg Induce cardiac arrest. Arteriovenous pressure gradient of 100 mmHg will force a flow of 5 L/min through the peripheral resistance of 20 mm Hg/L/min. (I=V/R) Although CO is 0 L/min, the flow through the microcirculation transiently is 5 L/min. Gradually, the blood volume in the arteries progressively declines and the blood volume in the veins progressively increases until the pressure gradient is 0. When the pressure gradient is zero, flow ceases through the microcirculatrion. At zero flow, arterial and venous pressure equalizes and the final pressure depends on the relative compliance of these vessels. Had the arterial and venous compliance been equal, the decline in Pa would have been equal to the rise in Pv. However, the veins are much more compliant than the arteries and the transfer of blood from arteries to veins at equilibrium would induce a fall in arterial pressure that is 19 X as great as the concomitant rise in venous pressure. The final pressure in the circulatory system in the absence of flow is the mean circulatory pressure. From this, two important points on the vascular function curve have been derived. Figure A represents the normal operating system (CO 5 L/min, Pv 2 mmHg). Then when flow was stopped (CO=0), Pv became 7 mmHg. Next, the arrested heart is suddenly restarted, and begins pumping at 1 L/min. Blood is being moved from the veins at a rate of 1 L/min and the arterial volume is increasing at the same rate. Hence Pv begins to fall and Pa begins to rise. Because of the difference in compliance, Pa will rise 19 times faster than Pv will fall. This will continue until the pressure gradient becomes 20 mmHg. This gradient will force a flow of 1 L/min through a resistance of 20 mmHg/L/min. (V=IR) You may have noticed the straight line on the curve. At some critical maximal value of CO, sufficient fluid will be translocated from the venous to the arterial side of the circuit to reduce Pv below the ambient pressure. The vessels will collapse when the intravascular pressure falls below the extravascular pressure and obstruct venous return. Hence, in this case, there is a limit on the maximal value of CO to 7 L/min. Effect of Blood Volume on the Vascular Function Curve The vascular function curve shifts to the right and left (no change in slope) with increases and decreases in blood volume. The maximal value of CO becomes progressively more limited as the total blood volume is reduced. This is why you can’t drive up CO in a dry patient with pressors. Effect of Peripheral Resistance on the Vascular Function Curve Increases or decreases in arteriolar tone do not significantly alter the mean circulatory pressure. Increased resistance moves more blood from the venous to arterial side and decreases the CVP for the same CO. The opposite occurs in vasodilation. The Heart and Vasculature are Coupled Functionally The intersection bewteen the vascular and cardiac function curve is homeostasis. It is the point that the system will return to after any perturbations. Consider a rise in Pv from the equilibrium point to point A. The elevated Pv would increase CO (A to B) during the next systole (Frank Starling). The increased CO results in the transfer of blood from the venous to the arterial side of the circuit, with a consequent reduction in Pv (B to C). Because of this reduction in Pv, the CO during the next beat diminishes (C to D) by an amount dictated by the function curve. Because point D is still above the intersection point, the heart will pump blood from the veins to the arteries at a rate greater than that at which the blood will flow across the peripheral resistance from arteries to vein. This process will continue, in diminishing steps with each heartbeat, until the point of intersection is reached. Myocardial Contractility – Consider the equilibrium values for CO and Pv are designated by point A. – Cardiac sympathetic nerve stimulation would abruptly raise CO to point B before Pv would change appreciably. – However, this high CO would increase the net transfer of blood from the venous to the arterial side of the circuit. – Consequently, Pv would begin to fall (point C). – CO would continue to fall until a new equilibrium point (D) was reached. Peripheral Resistance – Predictions concerning the effects of changes in peripheral resistance are complex because both the cardiac and vascular function curves shift. – With increased peripheral resistance, the vascular function curve is moves counterclockwise. – The cardiac function curve is also shifted downward because (1) as peripheral resistance increases, arterial pressure tends to rise; and (2) at any given Pv, the heart is able to pump less blood against a greater afterload. – Whether point B will fall directly below point A or will lie to the right or left of point A depends on the magnitude of the shift in each curve. Questions???