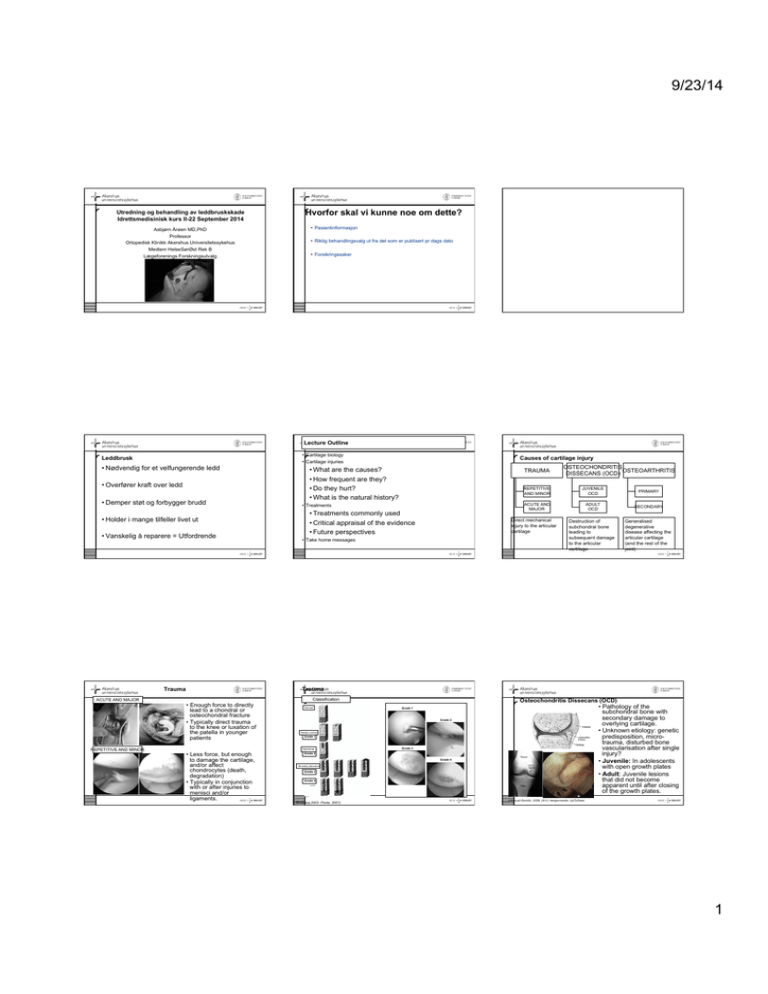
9/23/14
Utredning og behandling av leddbruskskade
Idrettsmedisinisk kurs II-22 September 2014
Hvorfor skal vi kunne noe om dette?
• Pasientinformasjon
Asbjørn Årøen MD,PhD
Professor
Ortopedisk Klinikk Akershus Universitetssykehus
Medlem HelseSørØst Rek B
Lægeforenings Forskningsutvalg
• Riktig behandlingsvalg ut fra det som er publisert pr dags dato
• Forsikringssaker
Lecture Outline
• Cartilage biology
• Cartilage injuries
Leddbrusk
• Nødvendig for et velfungerende ledd
• Overfører kraft over ledd
• Demper støt og forbygger brudd
• Treatments
• Treatments commonly used
• Critical appraisal of the evidence
• Future perspectives
• Holder i mange tilfeller livet ut
• Vanskelig å reparere = Utfordrende
Causes of cartilage injury
• What are the causes?
• How frequent are they?
• Do they hurt?
• What is the natural history?
TRAUMA
OSTEOCHONDRITIS
OSTEOARTHRITIS
DISSECANS (OCD)
REPETITIVE
AND MINOR
JUVENILE
OCD
PRIMARY
ACUTE AND
MAJOR
ADULT
OCD
SECONDARY
Destruction of
subchondral bone
leading to
subsequent damage
to the articular
cartilage
Generalised
degenerative
disease affecting the
articular cartilage
(and the rest of the
joint)
Direct mechanical
injury to the articular
cartilage
• Take home messages
Orthopedics
Trauma
Trauma
THE JOUR NAL
ACUTE AND MAJOR
REPETITIVE AND MINOR
BONE & JOINT SURGER Y · JBJS.ORG
VO L U M E 85-A · S U P P L E M E N T 2 · 2003
OF
Classification
• Enough force to directly
lead to a chondral or
osteochondral fracture
• Typically direct trauma
to the knee or luxation of
the patella in younger
patients
Normal
but a lesion with extensive cavitation into the bone may require bone-grafting.
Grade 1
OCD Lesion Classification
steochondritis dissecans is an osteochondral disease that
can be diagnosed with radiographs, which can be used to
Grade 2
determine the extent of osseous involvement and the depth
of the lesion. However, an arthroscopic description of the
osteochondral fragmentation is needed, and the ICRS has
suggested the following classification system (Fig. 5). Stable
lesions with a continuous but softened area covered by intact
cartilage are classified as ICRS OCD I, lesions with partial discontinuity that are stable when probed are classified as ICRS
OCD II, lesions with a complete discontinuity that are not yet
dislocated (“dead in situ”) are classified as ICRS OCD III, and
empty defects as well as defects with a dislocated fragment or
Grade
3 classified as ICRS OCD
a loose fragment within the
bed are
IV. Subgroups ICRS OCD I-IVB are defects that are >10 mm
in depth.
O
Nearly normal
Grade 1
Abnormal
• Less force, but enough
to damage the cartilage,
and/or affect
chondrocytes (death,
degradation)
• Typically in conjunction
with or after injuries to
menisci and/or
ligaments.
EV A L U A T I O N O F C A R T I L A G E
IN JU R I E S A N D RE P A I R
Grade 2
Severely abnormal
Grade 3
Grade 4
Fig. 4
The ICRS cartilage injury classification. (Reprinted from the ICRS Carti-
lage Injury Evaluation
Package2001)
[www.cartilage.org], with permission
(Brittberg,2003.
Poole,
from the International Cartilage Repair Society.)
subchondral bone plate. While débridement of unstable edges
(as is suggested for ICRS-2 lesions) is suitable for ICRS-3 lesions, further treatment is recommended for these more extensive lesions. A simple treatment is to imitate the vascular
tissue inflammatory phase by opening the subchondral space
with use of drilling, intracortical abrasion, or microfracture
techniques. A combination of drilling and perichondral or periosteal grafting is possible. Allografting or autografting with
osteochondral grafts is another treatment option, as is the use
of autologous grafted cultured chondrocytes.
Joint trauma may create cartilage defects that extend
into the subchondral bone. These full-thickness osteochondral injuries are classified as ICRS 4 (severely abnormal). Excluded from this grade are defects that are classified as
osteochondritis dissecans (OCD), which have a classification
system of their own (discussed below). ICRS-4 lesions can be
treated in the same manner as described for ICRS-3 lesions,
Grade 4
Transfer of the ICRS Classifications
into an Imaging Evaluation
ore active research is needed in order to correlate magnetic resonance imaging findings with the ICRS cartilage lesion classification. However, the available clinical and
research data allow some preliminary observations. As in most
magnetic resonance imaging studies with the clinically used
acquisition techniques, very little morphologic alteration in
ICRS-1a lesions have been reported and therefore it is difficult
to differentiate these lesions from normal (ICRS-0) cartilage.
In one study14 involving fat-suppressed fast-spin-echo imaging, areas of softening were detectable as regions of cartilage
signal abnormality without detectable morphologic changes.
dGEMRIC, a magnetic resonance imaging technique that is
beginning to be used in clinical studies, is sensitive to the concentration of glycosaminoglycan within the cartilage matrix
and shows great promise for the detection of cartilage softening and superficial fibrillation (i.e., ICRS-1a lesions)20. Since
ICRS-1b lesions (superficial lacerations and fissures) are
deeper, they should be more easily detected with magnetic
resonance imaging. However, the differentiation of ICRS-1b
lesions from ICRS-1a and ICRS-2 lesions may be difficult.
The spatial resolution of magnetic resonance images is
usually adequate to determine whether a cartilage defect involves >50% of the cartilage thickness (ICRS 3) or <50% of
the cartilage thickness (ICRS 2). However, if the deepest part
of the lesion is very focal and narrow, the grade of the lesion
may be underestimated with magnetic resonance imaging.
The deepest layers of articular cartilage usually appear dark
on magnetic resonance images, similar to the appearance of
the subchondral bone plate. Therefore, at this time, it is unlikely that magnetic resonance imaging will be able to differentiate among ICRS-3a lesions (which do not extend into the
calcified cartilage layer), ICRS-3b lesions (which extend down
to the calcified layer), and ICRS-3c lesions (which extend
down to but not through the subchondral bone plate). Blis-
microfracture the patient undergoing fragment
removal is highly individualized, with considerations of defect location, defect containment, the
condition of the bone, and the size and depth of the
lesion. Given the rehabilitation required following
microfracture, the decision is not taken lightly.
Even beyond the initial period of protected weight
bearing and continuous passive motion, if one
truly follows the existing recommendations about
return to sport for these patients, they would not be
allowed to return to high-level activities for at least
6–8 months. Thus, it can be challenging to hold
an active patient back when all that might have
been required was fragment removal to render them
symptom free.
We only microfracture the bed (of a recently
removed fragment) if it includes the ideal defect
characteristics, assuming the patient understands
and consents to the postoperative program (Figs 4
and 5). Although this decision-making is somewhat
intuitive, it is not supported by any literature that
demonstrates that, with this exact clinical scenario,
the symptoms will be reduced further than fragment
removal alone, that symptom onset will be prevented or delayed, or that the natural history of
the defect will be altered in any way.
FIGURE 5. After fragment removal, microfracture was
performed. Note the lesion is ideal for microfracture, with
chondral defect with good cartilage shoulders.
Miniaci and Tytherleigh-Strong [23] and remains
a consideration for a defect that has an intact,
relatively stable fragment within the defect bed.
Gudas et al. [22] reported a prospective, randomized
study comparing microfracture with osteochondral
autologous transplantation in OCD and found that
both groups demonstrated substantial improvement initially in clinical symptoms and in their
International Cartilage Repair Society scores, but
the microfracture group deteriorated over time,
with 41% failing (based on pain and joint swelling
necessitating a second-look surgery) at 4 years
compared with none in the transplant group.
Osteochondritis Dissecans (OCD)
Osteoarticular transfer system
• Pathology of the
subchondral bone with
secondary damage to
overlying
cartilage.
Autologous chondrocyte implantation
Autologous chondrocyte
transplantation
may be
• Unknown
etiology:
genetic
a good choice for large defects. Bentley et al. [24]
predisposition,
microreported good to excellent
outcomes in 88% of the
cohort from a large patient population undergoing
trauma,
disturbed bone
ACI for OCD lesions [24]. Kon et al. [25 ] recently
published second-generation
ACI,
together with
vascularisation
after
single
a bone graft in patients with OCD. Interestingly,
injury?
female sex and older age were related to the worst
prognosis.
• Juvenile: In adolescents
allograft
withOsteochondral
open growth
plates
Osteochondral allograft transplantation should be
considered as a salvage procedure and should rarely
• Adult:
lesions
be usedJuvenile
as first-line treatment.
Garrett [26] reported
outcomes
at a mean follow-up of 3 years
thatsuccessful
did
not
become
in 94% of the patients. McCulloch et al. [27] studied
the clinical outcomes
in 25 patients
who underwent
apparent
until after
closing
prolonged fresh osteochondral allograft (these
of the
grafts growth
are harvested plates.
and are typically maintained
This technique is ideal in those case scenarios
wherein the underlying subchondral bone integrity
has been significantly compromised. It could be
considered as a second-line treatment after a failed
microfracture or as a first-line treatment of highdemand patients with small chondral lesions.
A novel technique of using an osteochondral autograft plug as a biologic splint has been reported by
&
M
(Pascual-Garrido, 2009, 2013. Hergenroeder, UpToDate).
FIGURE 4. Typical osteochondritis dissecans lesion located
on the medial femoral condyle with loose body.
50
www.co-pediatrics.com
refrigerated at 48C for up to 28 days). Six of these
patients were diagnosed with OCD. They reported
84% patient satisfaction and 88% radiographic
incorporation of prolonged fresh allografts to the
Volume 25 ! Number 1 ! February 2013
Copyright © Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
1
9/23/14
Epidemiology – cartilage injuries
•
Osteoarthritis (OA)
•
•
•
•
Degeneration of cartilage
(with effects on the whole
joint)
Limited inflammation
Changes periarticular and
in subchondral bone
Major cause of disability
(Guccione, 1994)
Prevalence: Age > 60 y: 47
% (Leyland, 2012)
• Of 993 consecutive arthroscopies (Årøen,
2004):
• 66 % with cartilage changes incl. OA
changes
• 20 % had localised cartilage lesions
without OA (mostly younger patients)
• Most frequent on the medial femoral
condyle
B
• Frequent concomitant injuries to
menisci and ligaments A
• Corresponding results in prospective
and retrospective studies (Hjelle, 2002
PRIMARY
SECONDARY
• Trauma
Diagnostic criteria (Altman, 1986)
Knee pain + at least 3 of 6:
Age > 50 y
Bony tenderness
Stiffness < 30 min
Bony enlargement
Crepitus
No palpable
warmth
• Knee injury: Relative risk of OA 5.17 (Gelber, 2000)
• ACL injury: OA incidence 51% 12 years after injury (mean
age 31 y) (Lohmander, 2004)
• Cartilage injury (incl. OCD): Affected knees higher
incidence of OA 5-6 years after diagnosis (Loken, 2010. Knutsen,
2007)
• Reconstruction of ACL does not prevent OA (Lohmander,
2004. Von Porat, 2004. Daniel, 1994. Frobell, 2013)
• Unknown if treating cartilage injuries prevents early OA.
• Other risk factors: Congenital joint disorders,
malalignment, obesity, diabetes, hemophilia ++
(n=1000). Curl, 1997 (n=31,516). Widuchowski, 2007
(n=25,124))
• ACL-reconstructions: 17-27 % of
patients grade 1 or higher cartilage
lesion (Granan, 2009. Røtterud, 2011)
Diagnosis and symptoms
9%
44%
• Acute onset of symptoms in conjunction
with trauma
• Sub-acute onset (or lack of
improvement) with or without known
past trauma
• Symptoms
47%
• Knee pain, swelling, (pseudo-)locking,
catching
• Clinical exam
Grade III-IV
Vol. 32, No. 1, 2004
• Idiopathic
• Multifactorial incl. genetic and
acquired risk factors
• History
OCD
Grade I-II
Articular Cartilage Lesions in Knee Arthroscopies
213
• Effusion, evidence of ligament or
meniscal injury
4%
• Imaging
11 %
• X-ray: osteochondral fracture, large
OCDs, malalignment, OA
• MRI: chondral fractures (ligament/
menisci). NB! small lesions may not
show
43 %
C
• Diagnostic arthroscopy
• Rarely, normally only if ligament or
meniscal surgery is indicated
23 %
Figure 2. Different types of localized cartilage lesions (n =
203) of the knee. A, Localized partial-thickness cartilage
lesions 44%; B, Osteochondritis dissecans lesions 9%; C,
Localized full-thickness cartilage lesions 47%.
6%
9%
Chicago, Illinois). All percentages are given without any
decimals.
Figure 3. Anatomical distribution of the localized full-thickness cartilage defects of the knees (n = 203).
RESULTS
most frequent (Fig. 4). An x-ray examination was performed in 93% of the knees, and radiographic degenerative
changes were noted in 13% of all the knees.
Previous arthroscopic procedures had been performed in
28% of the knees, most commonly a meniscal resection or
an ACL reconstruction. Median time period from injury to
the current arthroscopic procedure was 296 days. The performed arthroscopic procedures are shown in Figure 5.
Pain was reported with a median value of 40 on a Visual
Analog Scale in which 0 was no pain at all and 100 represented the worst pain the patient could imagine. Seventythree percent of all the patients reported to be preoperatively very restricted by activity pain. Compared to their
healthy contralateral knee, half of the patients assessed
the function to be more than 60% reduced. Still, 82% of the
patients were preoperatively regularly doing exercise once
or twice weekly (Table 1).
Table 2 shows the different diagnosis groups and the
number of cases with concomitant localized cartilage
lesion. Patellar dislocation had the highest frequency of
associated cartilage lesion (57%) followed by older anterior cruciate ligament ruptures (29%) and partial anterior
cruciate ruptures (27%).
Most of the patients with localized cartilage lesions were
in younger age groups (median age 30 years), as illustrated in Figure 6. In the patients younger than 45 years of
age, the finding of articular cartilage changes as a total
was 54%, but the percentage of knees with localized (partial and full thickness) cartilage defects was 27%.
Articular cartilage changes were noted in 66% of the
knees. A localized cartilage lesion in combination with
degenerative changes was diagnosed in 5% (n = 47) of
knees. Localized cartilage lesions without degenerative
lesions were observed in 20% (n = 203) of all knees.
Localized cartilage lesions on opposing articular surfaces,
so-called “kissing lesions,” were diagnosed in 5 of these
203 knees. Figure 2 illustrates the different types of
lesions of the localized knee cartilage injuries (n = 203
knees). Full-thickness cartilage lesions were found in 11%
(n = 113) of the knees. The most serious cartilage injuries,
grade 3 and 4, were most commonly located at the medial
femoral condyle followed by patella, as illustrated in
Figure 3.
A full-thickness cartilage defect with a square area of
more than 2 cm2 was observed in 6% (n = 62) of all the
knees. Thirty-one of these 62 patients had a cartilage
lesion as their only pathology. Fifty percent of these larger
lesions (grade 3 to 4 and > 2 cm2) were localized at the
medial femoral condyle, and 13% were localized in femoral
trochlea. Ten cartilage lesions were classified as osteochondritis dissecans.
Of all patients (N = 993), an acute traumatic onset of the
knee symptoms was reported in 59% and a more gradual
nontraumatic onset in 41%. Sports participation was the
most commonly associated activity (49%), with team
sports such as soccer and European team handball as the
Downloaded from ajs.sagepub.com at Universitet I Oslo on February 4, 2010
Natural history
Symptomatic
?
Asymptomatic
Symptoms or no symptoms?
• Equal impact on quality of • 8 out of 10 endurance
life to patients waiting for a
runners had cartilage
total knee replacement (Heir, defects on MRI (Stahl, 2008)
2010)
• 50 % of asymptomatic knees
• Poorer self-reported
in 40 NBA players had
function in patients with
cartilage lesions (Kaplan, 2005.
reconstructed ACLs and full- Walczak, 2005)
thickness lesions 2-5 years
post surgery (Røtterud, 2011)
• Cartilage abnormalities in 8
% of asymptomatic
triathletes without prior knee
• Less return to sports if
concomitant cartilage injury injury and 31 % with prior
(Steinwachs, 2011)
injury (Shellock, 2003)
Idrettsutøver med bruskskade i kneet-hva trenger vi
• Anamnese
– Smertedebut
– Skader
– Idrett-funksjonsnivå-ambisjon
– Lysholm score
– Alder !!
• Of 28 athletes (severe lesions and minimal surgical intervention) 12
patients had no evidence of OA after 14 years. 22 patients had excellent or
good knee function (Messner, 1996)
• At mean 15.3-year follow-up there was no difference in presence of OA
between injured and uninjured knee in patients with a untreated single
isolated grade IV lesion (Widuchowski, 2011)
• Osteochondral injuries may heal with (fibrous) cartilage and clinical relief of
symptoms
• Not all chondral injuries progress into (early) OA
Klinisk undersøkelse
– Bevegelseutslag
– Knestabilitet
• Lachmann
• Skuffe test
• Patella stabilitet
– Patella Grinding test
– Hvor kjennes ujevnheten
– Palpasjonsømhet
– Kjenner du et fritt legeme?
Hva trengs for samtale om behandlingsalternativer
• Bilder
– Stående bilder, helst Synaflex
– MR- kan miste bruskskade
– Tvil om akser-bestille HKA
– Vurdere CT artrografi ved OCD
2
9/23/14
Hva må være på plass før behandling kan diskuteres
Behandling
Behandlingsalternativene
• Ikke artrose kne
• Aldri bruskkirurgi “by the way”
• Pasientinformasjon
• OSLO CARE (Cartilage Active Rehabilitation and Education)
Treatment
Treatment options
THE ULTIMATE GOAL
CONSERVATIVE
MEDICATIONS
Training
SURGICAL
FIXATION OF
LOOSE FRAGMENT
• Immobilisation leads to cartilage thinning, but increased loading on normal
cartilage does not lead to thicker cartilage (Eckstein, 2006)
• Patients with knee pain often have poor quadriceps strength and control.
• Preoperative training has proven very beneficial in ACL reconstruction surgery
(Eitzen, 2009)
[
DEBRIDEMENT
To reconstitute cartilage defects
with repair tissue with identical
properties to normal cartilage, with
perfect integration to surrounding
tissues, and with no changes to
subchondral bone!
MODIFICATION
OF ACTIVITY
TRAINING
BONE MARROW
STIMULATION
OSTEOCHONDRAL
TRANSPLANTATION
CELL BASED
IMPLANTATION
]
RESEARCH REPORT
300
100
Strength, Nm
• Pasient med tid og ressurser til å gjennomføre behandlingen
• Mikrofractur
• ACI
• Mosaikkartroplastikk
• Scaffold
90
BARBARA WONDRASCH, PT, MSc1 • ASBJØRN ÅRØEN, MD, PhD2,3 • JAN HARALD RØTTERUD, MD2,3
TURID HØYSVEEN, PT, MSc4 • KRISTIN BØLSTAD, MSc5 • MAY ARNA RISBERG, PT, PhD1
80
The Feasibility of a 3-Month Active
Rehabilitation Program for Patients With
Knee Full-Thickness Articular Cartilage
Lesions: The Oslo Cartilage Active
Rehabilitation and Education Study
60
250
+29.9%
+2.5%
Injured
Noninjured
200
150
100
50
70
0
Preintervention
Postintervention
50
40
FIGURE 6. Average ! SD isokinetic quadriceps
muscle strength for the injured and uninjured limbs
preintervention and postintervention (n = 44).
30
20
10
200
0
Pain
Symptoms
ADL
Preintervention
Sport
QL
Postintervention
Strength, Nm
• Ikke major malalignment
– Grundig gjennomgang av alternativene
– Hva som kreves av dem ved bruskkirurgi
– Hva som kan forventes til slutt
– Hvor lang tid det tar; 12-18 måneder
KOOS (0-100)
• Ikke instabilitet i kneet
150
+31.3%
+13.1%
100
50
0
! STUDY DESIGN: Prospective cohort study.
! OBJECTIVES: To evaluate the feasibility of an
active rehabilitation program for patients with knee
full-thickness articular cartilage lesions.
! RESULTS: The average adherence rate to the
rehabilitation program was 83%. Four patients
(9%) showed adverse events, as they could not
perform the exercises due to pain and effusion.
Significant and clinically meaningful improvement
was found, based on changes on the International
Knee Documentation Committee Subjective Knee
Evaluation Form 2000, the Knee injury and Osteoarthritis Outcome Score quality of life subscale,
isokinetic muscle strength, and hop performance
(P<.05), with small to large effect sizes (standardized response mean, 0.3-1.22).
K
FIGURE 5. Average ! SD KOOS scores preintervention and postintervention (n = 44). Abbreviations: ADL, activities
nee articular cartilage of daily living; KOOS, Knee injury and Osteoarthritis Outcome Score; QL, quality of life.
lesions occur frequently
and are a major clinical ed. The reason for implementing both program, and 54% for an 18-month
challenge in orthopaedic the online survey and the training dia- program) as the intervention becomes
and sports medicine, as well as ries was to gain more information about longer.24,54
in physical therapy.2,59 Patients adherence to the rehabilitation program.
The high adherence rate in our study
• 65 % of the patients enrolled opted to postpone
surgery
! BACKGROUND: No studies have yet evaluated
the effect of active rehabilitation in patients with
knee full-thickness articular cartilage lesions or
compared the effects of active rehabilitation to
those of surgical interventions. As an initial step, the
feasibility of such a program needs to be described.
! METHODS: Forty-eight patients with a knee full-
thickness articular cartilage lesion and a Lysholm
score below 75 participated in a 3-month active
rehabilitation program consisting of cardiovascular
training, knee and hip progressive resistance training, and neuromuscular training. Feasibility was determined by monitoring adherence to the program,
clinical changes in knee function, load progression,
and adverse events. Patients were tested before
and after completing the rehabilitation program by
using patient-reported outcomes (Knee injury and
Osteoarthritis Outcome Score, International Knee
Documentation Committee Subjective Knee Evaluation Form 2000) and isokinetic muscle strength
and hop tests. To monitor adherence, load progression, and adverse events, patients responded to an
online survey and kept training diaries.
! CONCLUSION: The combination of a high
adherence rate, clinically meaningful changes, and
positive load progression and the occurrence of
only a few adverse events support the potential
usefulness of this program for patients with knee
full-thickness cartilage lesions. This study was
registered with the public trial registry Clinical
Trials.gov (NCT00885729).
! LEVEL OF EVIDENCE: Therapy, level 2b.
J Orthop Sports Phys Ther 2013;43(5):310-324.
Epub 13 March 2013. doi:10.2519/jospt.2013.4354
! KEY WORDS: chondral injury, neuromuscular
exercises, strength exercises, tibiofemoral joint
often experience restrictions of daily,
recreational, and sports activities due to
functional impairments and disabilities.
Clinically, patients often present with
pain and effusion,31,33 as well as muscle
weakness, poor neuromuscular control,
and low self-reported knee function.40,45
Joint effusion reduces range of motion,
alters proprioceptive input, and potentially leads to muscle reflex inhibition.4,8,25
Knee function has been shown to be significantly worse in patients with articular cartilage lesions compared to patients
with anterior cruciate ligament (ACL) injury. Furthermore, quality of life has been
shown to be affected to the same extent
in patients with articular cartilage lesions
as in those with knee osteoarthritis (OA)
Norwegian Research Center for Active Rehabilitation, Department of Sports Medicine, Norwegian School of Sport Sciences, Oslo, Norway. 2Department of Orthopaedics,
Akershus University Hospital, Lørenskog, Norway. 3Oslo Sports Trauma Research Center, Department of Sports Medicine, Norwegian School of Sport Sciences, Oslo, Norway.
4
Ullernklinikken, Oslo, Norway. 5Norwegian Research Center for Active Rehabilitation, Department of Orthopaedic Surgery, Oslo University Hospital, Oslo, Norway. The study
protocol was approved by The Regional Ethical Committee for South-Eastern Norway. The authors certify that they have no affiliations with or financial involvement in any
organization or entity with a direct financial interest in the subject matter or materials discussed in the manuscript. Address correspondence to Dr May Arna Risberg, Department
of Sports Medicine, Norwegian School of Sport Sciences, PB 4014 Ullevaal Stadion, 0806 Oslo, Norway. E-mail: m.a.risberg@nih.no ! Copyright ©2013 Journal of Orthopaedic
& Sports Physical Therapy
1
310 | may 2013 | volume 43 | number 5 | journal of orthopaedic & sports physical therapy
Most patients reported that the training diaries were easy to complete, and
that the online survey would likely not
be needed to monitor adherence during
such a program.
The total adherence to the rehabilitation and return-to-activity phases was
83%, which is comparable to a previously reported24,54 adherence rate of 85%
for a 3-month exercise program for patients with knee OA. Adherence to rehabilitation has been shown to be crucial to
preserving physical performance, self-reported knee function, and pain reduction
in patients with knee OA.50 Adherence to
a rehabilitation program also influences
pain, quality of life, and physical performance in patients with knee OA.50,62 Few
studies have been designed to investigate
factors that influence adherence to a
program.50 One major factor seems to be
the duration of the program, with a progressive decline in adherence (85% for a
3-month program, 70% for a 9-month
may also be attributed to the study’s focus on patient education, which has previously been shown to be an important
factor to increase adherence in patients
with knee and hip OA.50 Qualitative studies have also demonstrated that some
patients express doubt as to whether exercise will be beneficial or detrimental to
their injury. Such doubt could reduce patients’ willingness to exercise.11,63
Clinically significant improvements in
both quadriceps (41.3 ! 33.8 Nm) and
hamstrings (23.3 ! 21.5 Nm) muscle
strength were found in this study. The
MDCs for quadriceps and hamstrings
strength have been reported to be 22.76
and 15.44 Nm, respectively.45 To our
knowledge, no previous studies have
reported changes in isokinetic muscle
strength after exercise interventions in
patients with articular cartilage lesions
in general or in those with full-thickness
articular cartilage lesions in particular.
However, studies evaluating the effect of
Injured
Noninjured
Preintervention
Postintervention
FIGURE 7. Average ! SD isokinetic hamstrings
muscle strength in the injured and uninjured limbs
preintervention and postintervention (n = 44).
resistance training have been reported in
patients with knee OA.40,42 King et al42
evaluated the effects of a 12-week, highintensity muscle strength program for patients with medial knee OA. They found
an improvement in isokinetic quadriceps strength (60°/s) of 33.6 Nm and in
hamstrings strength of 23.5 Nm after 12
weeks of resistance training.42 Another
study40 compared the clinical effects of
high- and low-resistance training for patients with knee OA. The high-resistance
training group demonstrated an increase
in isokinetic quadriceps strength (60°/s)
of 6.7 Nm and hamstrings strength of
14.4 Nm. The low-resistance group had
an improvement in quadriceps strength
of 11.5 Nm and hamstrings strength of
14.2 Nm.40 Our patients with full-thickness articular cartilage lesions had a
larger improvement in both quadriceps
and hamstrings muscle strength after a
3-month exercise program compared to
these patients with knee OA.
journal of orthopaedic & sports physical therapy | volume 43 | number 5 | may 2013 | 317
Fixation of loose fragment(s)
• Typical:
• Younger patient
• Patella luxation or other
trauma (could be judged as
relatively minor) or OCD
• Lack of clincial improvement
• Locking or pseudolocking
Debridement
• What it is:
• Removing loose cartilage bits
• Cleaning up the defect to get stable
edges
• Indications:
• May be the sole treatment for very
small lesions
• Usually the first step of more
invasive or more comprehensive
treatments
• Often done “en passant” on chance
findings
• Treatment
• Fixation with screws or
anchors combined with
microfracture
• What it does and does not do:
• Symptom relief in localised grade
3-4 lesions (reduces pain, locking
and swelling) (Hubbard, 1996)
• No stimulation or introduction of
repair tissue in the defect.
• NB! Does not really provide
anything more than placebo surgery
in OA (Moseley, 2002)
• Good prognosis if
diagnosed early
• The patients´ own cartilage
is much more likely to
constitute a good repair
Bone-marrow stimulation
• Rationale:
• Osteochondral injuries heal
because of bleeding and
cells from the bone marrow
• Allowing access from the
bone marrow into chondral
defects could promote
healing
• Blood clot
• Allows for a “normal” repair
process
• Stem and blood cells
(release of cytokines –
inflammation)
• Fibrin
www.shoulderkneedoc.com
3
9/23/14
Treatment of articular cartilage defects in athletes: An analysis of functio...
Field T Blevins; J Richard Steadman; Juan J Rodrigo; Jim Silliman
Orthopedics; Jul 1998; 21, 7; ProQuest Medical Library
pg. 761
Microfracture
• Rationale:
Bone-marrow stimulation
Bone-marrow stimulation
• Osteochondral injuries heal
because of bleeding and
cells from the bone marrow
• Allowing access from the
bone marrow into chondral
defects could promote
healing
Pain
• Developed by Pridie in the
1950s – drilling (Pridie, 1959)
• Questions about heat
necrosis of subchondral
bone
• 38 high-level and 140 recreational
athletes
• Full-thickness injuries (down to
bone), many with associated
ligament/meniscal injuries
• Re-thought and
popularised by Steadman
in the 1980s/90s –
microfracture (Blevins, 1998.
• Blood clot
• Allows for a “normal” repair
process
• Fibrin
• Stem and blood cells
• Release of cytokines –
inflammation
Steadman, 1998)
• The most commonly used
treatment option
Reproduced with permission of the copyright owner. Further reproduction prohibited without permission.
Reproduced with permission of the copyright owner. Further reproduction prohibited without permission.
Microfracture
Pro:
Contra:
– Repair tissue is fibrous,
not hyaline cartilage
– Long track record
– Easy and arthroscopic
surgery
– One step surgery
– Inexpensive
– Relatively fast recovery
Autologous osteochondral mosaicplasty for the treatment of full-thickness def...
Laszlo Hangody; Peter Fules
Journal of Bone and Joint Surgery; 2003; 85, ProQuest Medical Library
pg. 25
Osteochondral transplantation
• Circular osteochondral
plugs transferred from
uninjured parts of the knee
to the defect
• Developed by Matsusue
and Hangody in 1990s
(OATS, mosaicplasty)
(Matsusue, 1993. Hangody, 1997)
(Knutsen, 2004. Saris, 2008)
– Increase in failures over
time? (Mithoefer, 2009)
– Changes subchondral
bone (sclerosis)
(interference with later
treatments?) (Arøen, 2006.
• Similar method used for
large osteochondral defects
(complete condyle) with
allografts (Mankin, 1976)
– Deceased donors, grafts fresh
or cryopreserved
– Rarely used in Scandinavia
Minas, 2009. Pestka, 2012)
Osteochondral autografts
• Review of 831 mosaicplasties at one institution
• 92 % good-excellent results
• 3 % donor site morbidity
• Donor sites filled with fibrocartilage
• 69 out of 93 patients with second look arthroscopy
showed congruent joints
Reproduced with permission of the copyright owner. Further reproduction prohibited without permission.
Autologous Chondrocyte Implantation (ACI)
Osteochondral transplantation
32S
Cartilage 3(Suppl. 1)
and players who underwent ACI early (<12 months after
injury). In fact, the ability to return to playing football was
4 times higher when ACI was performed within 1 year after
injury (Table 1). No significant association was found
between return to football and gender, defect type, defect
location, defect size, or number of prior surgeries.
Concomitant procedures such as ligament reconstructions
or osteotomies did not decrease the ability to return to football, as 56% of players with osteotomies were able to
return to play football. Interestingly, postoperative participation in athletic activities improved the long-term functional results after first-generation ACI.11 The failure rate
was 13%, with half of the failures resulting from traumatic
delamination of hypertrophic grafts.
1st generation
Evolution of ACI
Pro:
– Fills the defect with hyaline
cartilage (Hangody, 2003)
– Subchondral bone defects
is treated as part of the
procedure
– Inexpensive
– One step procedure
– Smaller lesions may be
done arthroscopically
– Allograft is possible
Contra:
– Donor site morbidity
(Matricali, 2010)
– Limited number of plugs
– If failure the damage to
the subchondral bone
interferes with later
treatment
– Allografts pose (viral)
infection risk (CDC, 2002)
• Autologous chondrocytes
in suspension under a
sutured periosteal flap
• 23 patients with full thickness lesions (16 femoral, 7 patella)
• Mean follow-up 39 months
• 14 of 16 femoral transplants good to excellent
• 2 of 7 patellar transplants good to excellent
• 12 of 23 biopsies showed hyaline like cartilage
– Hypertrophy
– Need to harvest periost
– Sutures
– Leakage of cells?
– Uneven distribution of cells?
(Mithoefer, 2011)
(Cole, 2009)
The New England Journal of Medicine
Downloaded from nejm.org at HELSEBIBLIOTEKET GIR DEG TILGANG TIL NEJM on June 9, 2014. For personal use only. No other uses without permission.
Copyright © 1994 Massachusetts Medical Society. All rights reserved.
Figure 1. Intraoperative image of a football player treated
with first-generation autologous chondrocyte implantation,
demonstrating a full arthrotomy and sutured periosteal patch.
Technical Evolution of ACI
First-Generation Technique
With this original ACI technique, cartilage harvesting was
performed in a primary procedure, followed by cell isolation
and expansion in vitro. Implantation of the cultured chondrocytes was then performed in a second open procedure
under a periosteal patch acquired from the proximal tibia
and sutured to the surrounding stable cartilage margins with
the cambium layer facing toward the defect.7 The periosteal
rim was sealed with fibrin glue, and the cultured chondrocytes were then injected under the periosteal flap covering
the articular cartilage defect. This procedure often required
a large incision for access to the defect and periosteal harvest (Fig. 1). The results of this first-generation technique
have been described specifically for football players.9 Good
and excellent results were reported in 72% overall, in 85%
of players with single cartilage lesions, and in 93% of single
defects located on the medial femoral condyle. Postoperative
Tegner activity scores improved in 82% from an average
3.6 ± 0.2 points preoperatively to 6.1 ± 0.5 points at last
follow-up (P < 0.001). While overall rate to return to football was 33%, return rate was significantly better for competitive players at 83% compared to 16% in recreational
players (P < 0.001). Best return rates were observed in adolescent athletes with a return rate of 96%.10 Eighty percent
of returning players returned to the preinjury skill level.
Average time to return to football was 18 months (range,
12-24 months) for first-generation ACI. Time to return was
shorter in high-level soccer players (14 months) than in
recreational players (22 months) (P < 0.001). Of the returning players, 87% continued to play 52 months after ACI.
Return to football was significantly better in players with
single cartilage lesions of the femur, younger age (≤25 years),
Characterized Chondrocyte Implantation
The in vitro culture and expansion of human chondrocytes
for ACI have been shown to result in a dedifferentiation of
the cultured cells with a shift from a predominantly type II
collagen-containing hyaline matrix to a fibrocartilage-like
type I collagen-rich repair cartilage.12,13 To address this aspect,
characterized chondrocyte implantation (CCI) has been
developed to improve hyaline articular cartilage regeneration through the identification and selective expansion of
specific chondrocyte subpopulations capable of producing
more hyaline-like repair cartilage tissue. CCI uses the firstgeneration ACI surgical technique with a periosteal patch.
Prospective, randomized, controlled clinical comparison
of CCI with microfracture has shown superior structural
repair and histomorphometry with CCI at 12 months.12
Clinical results at 36 months have shown significantly
increased Knee injury and Osteoarthritis Outcome Score
(KOOS) sports and recreation subscores that were higher
than after microfracture.13 Better KOOS sports subscores
were seen when surgery was performed within 3 years from
injury. Recently discussed results show a persistent good
outcome at 5 years, and prospective cohort data using CCI
with a synthetic membrane clearly demonstrate a reduction
of hypertrophy compared to periosteal coverage.14 The same
authors found significant increases of the Activity Rating
Scale after CCI and that low-level joint-loading activities
after surgery had a beneficial effect on postoperative recovery with both faster return to preinjury activity levels and
significantly better overall knee function. Graft hypertrophy
was observed in 25% after CCI, with a failure rate of 4% at
36 months.13,15
Second-Generation Techniques
To avoid the frequent complication of graft hypertrophy and
the associated risk from delamination or requirement for
surgical chondroplasty of the hypertropic graft, bioabsorbable collagen membrane was developed as an innovative
Downloaded from car.sagepub.com at Oslo universitetssykehus. on June 4, 2014
The New England Journal of Medicine
Downloaded from nejm.org at HELSEBIBLIOTEKET GIR DEG TILGANG TIL NEJM on June 9, 2014. For personal use only. No other uses without permission.
Copyright © 1994 Massachusetts Medical Society. All rights reserved.
4
9/23/14
1788
THE JOURNAL
O F B O N E & J O I N T S U R G E RY J B J S . O R G
V O L U M E 9 1-A N U M B E R 7 J U LY 2 009
SU RGI CAL MA NAGEMEN T
DEFECTS IN THE KNEE
d
d
d
OF
ART I C U L A R CA RT I L AG E
!
TABLE IV Demographic Data and Clinical Outcomes in Studies of Autologous Chondrocyte Implantation
Author(s)
No. of Patients
34
126 with autologous
chondrocyte implant. after
other failed cartilage proc.
(multicenter study)
Zaslav et al.
35
Rosenberger et al.
36
Mandelbaum et al.
7
4.7 (range, 1-15.0)
Range, 16-48
118 with isolated
chondral lesion
Knutsen et al.
4.63
48.6 (range,
45-60); all >45
40
37
Mean Lesion Size (cm )
34.5
56; 50% with
concomitant
osteotomies
Kreuz et al.
2
Mean Age (yr)
4.5
35 (range, 18-50)
40 with autologous
chondrocyte implant.,
40 with microfract.
38
Steinwachs and Kreuz
63
34
*VAS = visual analog scale, SF-36 = Short Form-36, and ICRS = International Cartilage Repair Society.
1st generation
2nd generation
1st generation
• Autologous chondrocytes in
suspension under a sutured
periosteal flap
• Autologous chondrocytes in
suspension under a sutured
periosteal flap
– Less hypertrophy
– No periost harvest
– Still sutures
– Leakage of cells?
– Uneven distribution of cells?
– Hypertrophy
– Need to harvest periost
– Sutures
– Leakage of cells?
– Uneven distribution of cells?
– Hypertrophy
– Need to harvest periost
– Sutures
– Leakage of cells?
– Uneven distribution of cells?
3rd generation
• Autologous chondrocytes cultured
in a scaffold and implanted in the
defect
– No hypertrophy
– No periost harvest
– No or less sutures
– No leakage of cells
– Even distribution
– Possibility of arthroscopic procedure
tightness test is performed with an 18gauge angiocatheter. The chondrocytes
are then delivered through the opening
with use of an angiocatheter. After the
cells have been implanted, the opening
gap is closed with suture and fibrin
glue (Fig. 9, C).
Postoperatively, patients with a
femoral condyle lesion are kept nonweight-bearing and use a continuous-
passive-motion machine. Patients with
a patellofemoral lesion are permitted
full weight-bearing with the knee in
extension. Continuous passive motion
for six to eight hours per day at one
cycle per minute is used for six weeks
after the surgery. A return to normal
activities of daily living and sports
activities is allowed six months after
the surgery.
Autologous Chondrocyte Implantation (ACI)
2nd generation
Evolution of ACI
• Autologous chondrocytes in
suspension under a porcine collagen
type I/III membrane (Chondrogide)
Evolution of ACI
first passed into the patch approximately 2 mm from the edge and then
passed through the cartilage at a depth
of 2 to 3 mm below the cartilage
surface. Sutures should be placed approximately 4 mm apart, and a gap
should be maintained in the upper
edge to allow chondrocyte implantation (Fig. 10). The edges of the patch
are sealed with fibrin glue, and a water-
• Autologous chondrocytes in
suspension under a porcine collagen
type I/III membrane (Chondrogide)
Steinwachs et al.
9
– Less hypertrophy
– No periost harvest
– Still sutures
– Leakage of cells?
– Uneven distribution of cells?
Pro:
– Subchondral bone is left
undisturbed
– Large lesions may be
treated
– Later generations have
made procedure simpler
– Maybe better durability
Autologous chondrocyte implantation. A: A chondral lesion in the patella. B: Preparation of the defect. C: After the chondrocytes are delivered, the gap is
Matrix Assisted
Chondrocyte
Implantation
9
Steinwachs et al.
Hyalograft-C
sutures (hence time of surgery) can be reduced using the
ACT-CS technique. The spacing and number of sutures
should be sufficient to just allow mechanical stability of the
cell-seeded membrane to the defect edges and onto the bottom of the defect. Gaps between the seeded membrane and
adjacent cartilage should be avoided, depending on the
lesion size, and often 6–12 sutures per defect are sufficient
to achieve adequate positioning and stability of the implant.
The authors recommend a monofilament suture material
(i.e., PDS 6-0, Fa. Ethicon, Nordersted, Germany) as monofilament sutures are considered more compatible and less of
an irritant to normal cartilage and membrane. Although the
degradation time for the sutures could play a critical role in
clinical outcome, the authors are unaware of any detailed
studies that have examined this in order to find an optimal
material. Hunziker et al. demonstrated that suturing was
associated with some local degeneration based on a histological evaluation,32 but it remains unclear if these observations are of clinical relevance.
The authors recommend positioning the needle insertion
close to the bottom of the defect, in close proximity to the
subchondral bone. Positioning the membrane on top of the
cartilage should be avoided since this could result in delamination or disintegration to the borders and lifting of the
membrane from the defect with any shear force. An example of the preferred technique is shown in Figures 3 and 4.
There is general agreement that knots can potentially
cause problems, especially in a mechanically active joint.
Placing the knots on the cartilage surface increases local
shear forces and should be avoided. The authors agree that
the best position for knots is beneath the surface of adjacent
cartilage, directly on the transplanted membrane. This position also forces the membrane to the bottom of the defect
directly opposed to the subchondral bone plate. An example
of proper positioning of knots is displayed in Figure 5.
Contra:
Fig. 9
Figure 3. Cell-seeded membrane is placed on the bottom of
the prepared defect, cell-loaded side of the membrane directed
toward and in direct contact with the subchondral bone plate
Figure 4. PDS 6-0 is recommended as a suture material to fix
the cell/membrane construct into the adjacent cartilage. A strict
position of the needle close to the subchondral bone needs to
be regarded in order to provide a close contact of cells and
subchondral bone
10
Figure 3. Cell-seeded membrane is placed on the bottom of
the prepared defect, cell-loaded side of the membrane directed
toward and in direct contact with the subchondral bone plate
Cartilage 3(1)
Until preparation of the present manuscript, the authors
(M.S., P.V., and P.N.) have conducted approximately 250
autologous chondrocyte transplantations using the ACT-CS
technique. Clinical 2-year results of the first 59 patients
treated with ACT-CS have been reported recently,23 demonstrating
a success
(ICRS “A”asand
“B” atmaterial
24 months)
Figure 4. PDS
6-0 israte
recommended
a suture
to fix
the89%
cell/membrane
the adjacent
cartilage. Ainstrict
of
and a rateconstruct
of 94 % into
improved
knee function
the
position of of
the patients
needle close
to the
subchondral
needs to
subgroup
with
single
defects.bone
Three-year
be regarded
in order to
a close contact
of cells and
results
are upcoming.
Noprovide
technique-related
complications
adjacent cartilage should be avoided, depending on the
subchondral bone
were observed during the application of ACT-CS so far.
lesion size, and often 6–12 sutures per defect are sufficient
ACT-CS appears to be safe and reproducible. Nevertheless,
to achieve adequate positioning and stability of the implant.
using fibrin glue (see Fig. 6). The cell compatibility of
long-term follow-ups are not yet available and results of
The authors recommend a monofilament suture material
fibrin glue and the ability of fibrin to support chondrogenic
ACT-CS used for the treatment for larger defects are still
(i.e., PDS 6-0, Fa. Ethicon, Nordersted, Germany) as monophenotype has been reported in various studies.33-37 This
elusive.
filament sutures are considered more compatible and less of
has also been demonstrated for the combination of fibrin
an irritant to normal cartilage and membrane. Although the
glue and the Chondro-Gide® membrane.38 Any fibrin glue
degradation time for the sutures could play a critical role in
Conclusion
used in ACT-CS should have demonstrated compatibility
clinical outcome, the authors are unaware of any detailed
with chondrocytes and the collagen membrane used.
In conclusion, although the clinical evidence is limited, the
studies that have examined this in order to find an optimal
TissuCol (Baxter, Unterschleißheim, Germany) has been
present paper provides concrete guidelines to surgeons on a
material. Hunziker et al. demonstrated that suturing was
shown to have good chondrocyte compatibility,37 and this
standardized methodology for using the ACT-CS technique
associated with some local degeneration based on a histotype of 6.fibrin
also been usedat inthetheinterface
ACT-CS
for the treatment of symptomatic full-thickness cartilage
Figure
Fibringlue
glue
is carefully
of
32 has
logical evaluation,
but
it remainsplaced
unclear if these observaFigure 5.
are typically placed
of the
study.23 The
fibrin glue
should
bethis
limited.
There
defects.
AllKnots
recommendations
were under
basedthe
on surface
a consensus
membrane
andamount
adjacentof
cartilage
in order
to seal
intersection.
tionsamount
are of of
clinical
relevance.
adjacent cartilage in order to avoid any irritation of the adjacent
The
fibrinon
glue
be limited
in order
to reach
an
is also
consensus
theshould
fact that
the entire
defect
should
meeting
of the authors of the present article. The recomcartilage
The authors recommend positioning the needle insertion
appropriate
not be filledsealing
or covered with fibrin glue.
mended procedures for ACT-CS are based on the authors’
close to the bottom of the defect, in close proximity to the
clinical experience in treating more than 200 patients with
subchondral bone. Positioning the membrane on top of the
ACT-CS over the past 5 years. A standardized methodology
cartilageExperience
should be avoided
since this could result in delamusing fibrin glue (see Fig. 6). The cell compatibility of
Sealing and Use of Fibrin Glue
Clinical
with ACT-CS
Geistlich) and represents an adoption of the initially
provides a framework for further comparative studies
ination or disintegration to the borders and lifting of the
fibrin glue and the ability of fibrin to support chondrogenic
After fixation of the cell-seeded membrane by sutures, the
ACT-CS as
described
in athe
paperinjected
uses a beneath
porcine
described
technique
using
cellpresent
suspension
between various techniques to identify optimal treatment
membrane from the defect
phenotype has been reported in various studies.33-37 This
14,15with any shear force. An examauthors recommend an additional sealing of the border
collagen
type
I/III membrane
(Chondro-Gide®,
Fa.
the
identical
membrane.
This technique
has been intromodalities, especially with evolving innovative regenerative
ple of the preferred technique is shown in17Figures 3 and 4.
has also been demonstrated for the combination of fibrin
duced as the “second-generation” ACT. For this techmedicine products.
There is general agreement that knots can potentially
glue and the Chondro-Gide® membrane.38 Any fibrin glue
nique and for the MACI technique, which also represents
cause problems, especially in a mechanically active joint.
used in ACT-CS should
have demonstrated compatibility
Acknowledgment
and Funding
an adoption using the identical biomaterial,25 various studDownloaded from car.sagepub.com at Universitet I Oslo on June 9, 2014
Placing the knots on the cartilage surface increases local
with chondrocytes and the collagen membrane used.
ies report safety, and midterm clinical outcome has been
Figures 2-6 have been produced with financial support of Tigenix,
shear forces and should be avoided. The authors agree that
TissuCol (Baxter, Unterschleißheim, Germany) has been
Leuven, Belgium.
reported in several case series in the treatment of cartilage
the best position for knots is beneath the surface of adjacent
shown to have good chondrocyte compatibility,37 and this
defects and osteochondritis dissecans.4,11,14-16,25 All these
cartilage, directly on the transplanted membrane. This positype of fibrinofglue
has also Interests
been used in the ACT-CS
Declaration
Conflicting
studies do not report any specific side effects and adverse
tion also forces the membrane to the bottom of the defect
study.23 The amount of fibrin glue should be limited. There
events in context with the application of the collagen memAll authors have received grants for limited educational purposes
directly opposed to the subchondral bone plate. An example
is also consensus on the fact that the entire defect should
by Tigenix, Leuven, Belgium.
brane. In addition clinical outcome seems promising and
of proper positioning of knots is displayed in Figure 5.
not be filled or covered with fibrin glue.
success rates vary between 82% and 95%. Using the colReferences
lagen membrane seems to further reduce the incidence of
graft
hypertrophy
demonstrated
1. Brittberg
M, Lindahlwith
A, Nilsson
A, Ohlsson C, Isaksson O,
Sealing
and Use as
of Fibrin
Glue in a prospective ranClinical
Experience
ACT-CS
Peterson L. Treatment of deep cartilage defects in the knee
domized trial versus periosteum-covered ACT11 as well as
After fixation of the cell-seeded membrane by sutures, the
ACT-CS as described in the present paper uses a porcine
with autologous chondrocyte transplantation. N Engl J Med.
in large retrospective studies including more than 400 patients
authors recommend an additional sealing of the border
collagen type I/III membrane (Chondro-Gide®, Fa.
1994;331(14):889-95.
with ACT.13 Compared with conventional periosteum2. Peterson L, Brittberg M, Kiviranta I, Akerlund EL, Lindahl
covered ACT, as a possible disadvantage a higher rate of
A. Autologous chondrocyte transplantation. Biomechanics
malfusion of the regenerative tissue into the adjacent cartiDownloaded
from car.sagepub.com
Oslo on
June 9, 2014 durability. Am J Sports Med. 2002;30(1):2-12.
long-term
lage has been reported, but this observation
does
not seem at Universitet Iand
3. Peterson L, Minas T, Brittberg M, Lindahl A. Treatment of
to be specific for the collagen membrane, and it has also
osteochondritis dissecans of the knee with autologous chonbeen observed in other artificial biomaterials.13
drocyte transplantation: results at two to ten years. J Bone Joint
ACT-CS represents an adoption of the initial technique
Surg Am. 2003;85-A(Suppl 2):17-24.
using the collagen membrane for ACT. The first patients
4. Krishnan SP, Skinner JA, Carrington RW, Flanagan AM,
were treated using the ACT-CS technique in October 2005,
Briggs TW, Bentley G. Collagen-covered autologous
and the principles of the technique were described in 2009.22
sutures (hence time of surgery) can be reduced using the
ACT-CS technique. The spacing and number of sutures
should be sufficient to just allow mechanical stability of the
Figure 5. Knots are typically placed under the surface of the
cell-seeded membrane to the defect edges and onto the botadjacent cartilage in order to avoid any irritation of the adjacent
tom of the defect. Gaps between the seeded membrane and
cartilage
– Donor site morbidity
closed with suture and fibrin glue.
(Whittaker, 2005)
– Expensive
– Two surgeries
– Not exclusively hyaline
cartilage (long maturation
process?) (Knutsen, 2004.
(Vanlauwe, 2011)
– Maybe more hyaline like
tissue (Saris, 2008. Roberts,
Saris, 2008. Roberts, 2009)
2009)
(Cole, 2009)
Downloaded from car.sagepub.com at Universitet I Oslo on June 9, 2014
Future perspectives with ACI
The best evidence – RCTs
• Better cells?
What to choose? A critical appraisal!
• Characterised chondrocytes
(Saris, 2008, 2009, 2014. Vanlauwe, 2011)
• Stem cells instead of
chondrocytes (Wakitani, 2002, 2004.
Kuroda, 2007. Nejadnik, 2010)
Autologous Bone Marrow–Derived
Mesenchymal Stem Cells Versus
Autologous Chondrocyte Implantation
Conclusion: BM-MSC were just
as good as chondrocytes
An Observational Cohort Study
Hossein Nejadnik,* MD, James H. Hui,*y MBBS, FRCS, FAMS, Erica Pei Feng Choong,z
Bee-Choo Tai,§ PhD, and Eng Hin Lee,* MD, FRCS
From the *Department of Orthopedic Surgery, Yong Loo Lin School of Medicine, National
University of Singapore, Singapore, zNational University Hospital, National University Health
System, Singapore, and the §Department of Epidemiology and Public Health, Yong Loo Lin
School of Medicine, National University of Singapore, Singapore
• New scaffolds?
COPYRIGHT © 2005
• Injectable hydrogels?
• Cartipatch, NovoCart3D, NeoCart, ++
Purpose: This study was conducted to compare the clinical outcomes of patients treated with first-generation autologous chondrocyte implantation to patients treated with autologous bone marrow–derived mesenchymal stem cells (BMSCs).
Study Design: Cohort study; Level of evidence, 3.
Results: There was significant improvement in the patients’ quality of life (physical and mental components of the Short
Form-36 questionnaire included in the ICRS package) after cartilage repair in both groups (autologous chondrocyte implantation and BMSCs). However, there was no difference between the BMSC and the autologous chondrocyte implantation
group in terms of clinical outcomes except for Physical Role Functioning, with a greater improvement over time in the
BMSC group (P 5 .044 for interaction effect). The IKDC subjective knee evaluation (P 5 .861), Lysholm (P 5 .627), and Tegner
(P 5 .200) scores did not show any significant difference between groups over time. However, in general, men showed
significantly better improvements than women. Patients younger than 45 years of age scored significantly better than patients
older than 45 years in the autologous chondrocyte implantation group, but age did not make a difference in outcomes in the
BMSC group.
Conclusion: Using BMSCs in cartilage repair is as effective as chondrocytes for articular cartilage repair. In addition, it required 1
less knee surgery, reduced costs, and minimized donor-site morbidity.
Keywords: chondrocyte; autologous chondrocyte implantation (ACI); bone marrow–derived mesenchymal stem cell
Full-thickness, focal cartilage defects cause knee symptoms
such as pain, popping, and swelling42 and affect patients’
quality of life and career. Recent large arthroscopic studies
have indicated that the prevalence of cartilage defects is
between 11% and 63%.1,9,14 Treatment of articular cartilage
defects remains challenging8,21,26 because cartilage tissue
has a limited capacity for repair.16,27,28 One of the most
promising treatments for cartilage defects is autologous
chondrocyte implantation (ACI),3,6,10,31 which provides
y
Address correspondence to James H. Hui, MBBS, FRCS, FAMS,
Department of Orthopaedic Surgery, Yong Loo Lin School of Medicine,
National University of Singapore, Singapore (e-mail: jameshui@nus
.edu.sg).
The authors declared that they had no conflicts of interests in their
authorship and publication of this contribution.
The American Journal of Sports Medicine, Vol. 38, No. 6
DOI: 10.1177/0363546509359067
! 2010 The Author(s)
THE JOURNAL
OF
BONE
AND JOINT
SURGERY, INCORPORATED
An Analysis of the Quality of
Cartilage Repair Studies
Background: First-generation autologous chondrocyte implantation has limitations, and introducing new effective cell sources
can improve cartilage repair.
Methods: Seventy-two matched (lesion site and age) patients underwent cartilage repair using chondrocytes (n 5 36) or BMSCs
(n 5 36). Clinical outcomes were measured before operation and 3, 6, 9, 12, 18, and 24 months after operation using the International Cartilage Repair Society (ICRS) Cartilage Injury Evaluation Package, which included questions from the Short-Form
Health Survey, International Knee Documentation Committee (IKDC) subjective knee evaluation form, Lysholm knee scale, and
Tegner activity level scale.
BY
Conclusion: Generally poor
methodology and only 4 RCTs
BY RUNE B. JAKOBSEN, LARS ENGEBRETSEN, MD, PHD, AND JAMES R. SLAUTERBECK, MD, PHD
Author (year)
Compared
Results
Comments
Bentley (2003, 2012)
ACI vs. OATS
ACI better at 2 y and >10 y
More failures in OATS
Horas (2003)
ACI vs. OATS
ACI = OATS at 2 y
Poor follow-up. ACI
slower.
Knutsen (2004, 2007)
ACI vs. MFX
ACI = MFX at 2 y and 5 y
Younger and active did
better. Fibrocartilage in
both groups
Visna (2004)
MACI vs. debridement
MACI better at 1 y
Cells in fibrin glue
Gudas (2005, 2006,
2012)
OATS vs. MFX
OATS better at 2,5 y and 10
y
Bartlett (2005)
ACI vs. MACI
ACI = MACI at 1 y
Mostly fibrocartilage
Dozin (2005)
ACI vs. OATS
ACI = OATS at variable
followup
Low powered. High
degree of improvement
after initial debridement
Gooding (2006)
ACI 1st vs. ACI 2nd
ACI 1st = ACI 2nd
More hypertrophy in ACI
1st
Saris (2008, 2009)
Vanlauwe (2011)
ACI vs. MFX
ACI = MFX at 1 y
ACI better at 3 y
ACI = MFX at 5 y
Characterised
chondrocytes
Better histology in ACI
Basad (2010)
MACI vs. MFX
MACI better at 2 y
Large lesions (4-10 cm2)
Gudas (2013)
OATS vs. MFX vs.
debridement
OATS better at 3 y
In patients with ACL
reconstruction
Saris (2014)
MACI vs. MFX
MACI better at 2 y
Histology was equal
Investigation performed at the Oslo Sports Trauma Research Center and the Orthopaedic Center, Ullevaal University Hospital, Oslo, Norway
Background: Most lesions of articular cartilage do not heal spontaneously and may lead to secondary osteoarthri-
tis. It is not known whether the optimistic reports on the short and long-term results of several different cartilage rewww.ungc.libguides.com
pair techniques are based on sound methodological quality.
Methods: We performed a literature search in MEDLINE, CINAHL, the Cochrane Central Register, and EMBASE and
included studies in which the primary aim of the investigation was to report the outcome after cartilage repair in the
knee with use of microfracture, autologous osteochondral transplantation, autologous periosteal transplantation, or
autologous chondrocyte implantation. We scored the quality of the studies using a modified Coleman Methodology
Score with ten criteria, which results in a final score between 0 and 100. Studies were also assessed with use of the
level-of-evidence rating used in the American Volume of The Journal of Bone and Joint Surgery. We collected data on
the year of publication, the reported postoperative results, and the outcome measures used to assess the results.
Results: Sixty-one studies involving a total of 3987 surgical procedures were included. The average methodology score
was 43.5 of 100. Methodological deficiencies were found with respect to five criteria: the type of study, description of
the rehabilitation protocol, outcome criteria, outcome assessment, and subject selection process. Large variations in
the reported outcome were seen within each treatment modality, and no significant differences were found between
each kind of therapy (p = 0.11). The methodology score correlated positively with the level-of-evidence rating (r = 0.668,
p < 0.0001), but there were large variations in the methodology score within each level. The linear regression analysis
weighted by the number of patients demonstrated a negative yet not significant correlation between the methodology
score and the results reported in nineteen studies with use of the Lysholm Scale (r = –0.29, p = 0.19). A total of twentyseven different clinical outcome measurement scales were used to assess outcome.
Conclusions: The generally low methodological quality found in the studies included in this analysis indicates that
caution is required when interpreting results after surgical cartilage repair. Firm recommendations on which procedure to choose cannot be given at this time on the basis of these studies. More attention should be paid to methodological quality when designing, performing, and reporting clinical studies.
Level of Evidence: Therapeutic Level III. See Instructions to Authors for a complete description of levels of evidence.
S
urgical treatment for articular cartilage injury is of major interest to orthopaedic surgeons because most lesions of articular cartilage do not heal spontaneously
and may predispose the joint to the subsequent development
of secondary osteoarthritis1,2. In a series of 993 knee arthroscopies performed because of pain, substantial cartilage lesions
considered suitable for surgical treatment (those that were >2
cm2 in size and grade 3 or 4, according to the system of the
International Cartilage Repair Society3) were detected in 6%
of the patients4. Treatment for articular cartilage injuries includes the microfracture technique5, autologous periosteal
transplantation6, autologous osteochondral transplantation7,
and autologous chondrocyte implantation8; however, much
controversy surrounds the best treatment option. Numerous
published articles, in which the above treatment options were
used, have described good or excellent results for a majority of
314
patients9,10. However, several authors have pointed out methodological weaknesses in the published studies11-13.
The purpose of this analysis was to determine whether
the optimistic reports in the literature are supported by sound
methodological quality in the studies. Our main hypothesis
was that the majority of the studies have methodological limitations that may limit the value of the reported results. Our
second hypothesis was that studies of lesser methodological
quality describe higher rates of success. We addressed methodological limitations by calculating a modified Coleman
Methodology Score14 and level-of-evidence rating15 and correlated these to the reported results. We also correlated the Coleman Methodology Score with the year of publication to study
trends over time. In addition, we collected the different outcome measurement scales used to assess outcome in order to
determine the diversity in this area.
TABLE 1.
Form of Bias
Selection
Nonresponder
Performance
Cartilage 1(4)
Downloaded from www.ejbjs.org on January 17, 2006
Table 1. Assessment of the Inclusion Criteria of the 8 Articles and Common Inclusion Criteria
9,10
Knutsen et al.
Saris et al.14
Gudas et al.12,13
Bentley et al.11
Bartlett et al.17
Gooding et al.16
Dozin et al.15
Horas et al.18
Common
Transfer
Number
Size, cm2
Age
Localization
Single lesion
Single lesion
Single lesion
Symptomatic lesion
Lesion
Symptomatic lesion
Focal defect
Single lesion
Single, symptomatic lesion
2-10
1-5
1-4
1-12
>1
1-12
>1
(3.2-5.6 as descriptive)
3.2-4
18-45
18-50
<40
16-49
15-50
15-52
16-40
18-45
18-40
Femoral condyle
Femoral condyle
Weight-bearing femoral condyle
Whole knee joint
Whole knee joint
Whole knee joint
Weight-bearing condyle
Weight-bearing femoral condyle
Weight-bearing femoral condyle
% Eligibility
31
37
30
74
77
80
45
7
4
RCTs
Tablevs.
2. The 8clinical
Included RCTs, thepractice
2 Compared Cartilage Repair Procedures for Each Study, and Number of Included Patients
RCT
ACI > OATS (Bentley)
MACI > debridement (Visna)
MACI > MFX (Basad)
MACI > MFX (Saris)
OATS > MFX (Gudas)
OATS > MFX (Gudas)
Equal outcomes
ACI = OATS (Horas)
ACI = OATS (Dozin)
ACI = MFX (Knutsen)
ACI = MFX (Saris)
ACI = MACI (Bartlett)
ACI 1st = ACI 2nd (Gooding)
ACI: Autologous Chondrocyte Implantation. OATS: Mosaicplasty/Osteochondral Autograft Transplantation. MFX:
Microfracture. MACI: Matrix-assisted ACI.
Procedure 1
et al.9,10
Saris et al.14
ACI
CCI
Horas et al.18
ACI
Original Article
Knutsen
Knee
Cartilage
MOAT
Gudas
et al.12,13 Defect Patients
11
ACI
Bentleyin
et al.
Enrolled
Randomized
Controlled
ACI
Bartlett et al.17
Trials
Are Not Representative
ACI (periosteum)
Gooding et al.16
15
of Patients
Orthopedic Practice
ACI
Dozin et al.in
Procedure 2
MF
MF
MF
MP
Matrix-induced ACI
ACI (collagen type I/III)
MP
OCT
Cartilage
1(4) 312–319
© The Author(s) 2010
Reprints and permission:
sagepub.com/journalsPermissions.nav
DOI: 10.1177/1947603510373917
http://cart.sagepub.com
Strategy
Randomization protocol; strict inclusion/exclusion
criteria; control of patient- and surgery-specific
factors
Comprehensive patient follow-up (!80%)
Minimal losses to follow-up
Artifactual findings resulting from errors in diagnostic or
outcome measurement
Publication
Form of reporting bias leading to over-representation of
significant or positive studies in systematic reviews
Study design
Error resulting from failure to identify issues with
internal or external validity
Measurement
Confounding
Systematic error in data collection
Interference from a third variable that distorts the
association between treatment and clinical outcomes
RCTs
Standardized surgical technique and postoperative
protocol; similar surgical experience; surgeon
facile in both surgical treatments
Comprehensive patient follow-up (!80%)
Minimal losses to follow-up
Double-blinded protocol; third-party/independent
observers at follow-up; objective outcome
measures
Publication of well-designed RCTs irrespective of
clinical results; limitations of multiple
publications
Designation of an appropriate control group
Control for open surgical technique or staged
surgical interventions
Use of validated patient outcome measures
Strict inclusion/exclusion criteria; isolated
chondral lesions; limited prior or concomitant
procedures; short preoperative symptom
duration
Number of Included Patients
cartilage. However, given the intrinsic challenges of
this particularSystematic
subject Review
matter, the limitations of patient parameters
and study
consideration
Limitations
and Sources
of Biasdesign
in Clinical
Knee can
be difficult Cartilage
to avoid. Research
Similarly, comparative evaluations can be difficult to assess based on the differences highlighted later. Table 2 defines the biases
Jamie Worthen, M.D., CPT Brian R. Waterman, M.D., MC, USA,
present
eachM.D.,
study,
and H.Table
3 defines
specific
Philip A. in
Davidson,
and James
Lubowitz,
M.D.
80
118
60
100
91
68
47
40
limitations and challenges highlighted by the authors of each study.
Bartlett et al.2 (2005)
Clinical Study: Bartlett et al.2 compared the results of ACI with a porcine-derived type I/type III
collagen cover versus matrix-induced autologous chon-
RCT, randomized controlled trial; ACI, autologus chondrocyte implantation; MF, microfracture; CCI, characterized chondrocyte implantation; MOAT, mosaic
1
1,2
1,2
C.N. Engen
, L. Engebretsen
, and A. Årøen
osteochondral
autologus transplantation;
MP, mosaicplasty; OCT, osteochondral cylinder transplantation.
Purpose: The purpose of this study was to systematically review the limitations and biases inherent to
surgical trials on the management of knee chondral defects. Methods:ABLE
A literature search of PubMed/
Medline, CINAHL (Cumulative Index to Nursing and Allied Health Literature), EMBASE, and the
Cochrane Central Register of Controlled Trials was conducted in September 2010 and updated in
August 2011 to identify all English-language, Level
I evidence,
randomized
controlled
Bartlett
et prospective,
Basad
et
Bentley et
trials published from 1996 to present. The keyword search
included the following:
“autologous 5
al.2
al.3 “mosaicplasty,”
al.
chondrocyte,” “cartilage graft,” “cartilage repair,” “chondroplasty,”
“microfracture,”
and/or “osteochondral.” Nonoperative studies, nonhuman
studies,vnon-knee studies,
ACI vstudies, ex vivo
MACI
ACI v
and/or studies with follow-up of less than 1 year were excluded. A systematic review was performed
Study
MACI
MFX
MOATS
on all included studies,
and limitations and/or biases
were identified and
quantitated. Results:
Of
15,311 citations, 33 abstracts were reviewed and 11 prospective, randomized controlled trials were
included. We identified 9 major limitations (subject age, subject prior surgery, subject duration of
bias
"procedure selection,#procedure standardiza""
symptoms,Selection
lesion location,
lesion size, lesion number,
tion, and Performance
limited histologic bias
analysis) and 7 common
biases (selection,#
performance, transfer,
NP
NP
nonresponder, detection, publication, and study design). Conclusions: Level I therapeutic studies
investigating
the surgical
management of human knee
Transfer
bias
#cartilage defects have
" substantial identified#
biases and limitations. This review has limitations because other classifications of bias or limitation
Nonresponder
bias defects is controversial,
"
"" research methods"
exist. Optimal
management of cartilage
and future rigorous
could minimize common biases through strict study design and patient selection criteria, larger
Detection bias
"
NP
"
patient enrollment, more extended follow-up, and standardization of clinical treatment pathways.
Level of Evidence:
Level I,bias
systematic review of Level
Publication
# I studies.
#
#
T
Abstract
9-18
Objective: Knee cartilage defects represent a socioeconomic
burden and may cause14lifelong disability. Studies have shown
that cartilage defects are detected in approximately 60% of knee arthroscopies.
In clinical trials, the majority of these patients
18
are excluded. This study investigates whether patients included in randomized controlled trials (RCTs) represent a selected
group compared to general cartilage patients. Design: Published randomized clinical trials on cartilage repair studies were
identified (May 2009) and analyzed to define common inclusion criteria that in turn were applied to all patients submitted
to our cartilage repair center during 2008. Patient-administered Lysholm knee score was used to evaluate functional level
at referral. In addition, previous surgery and size and localization of cartilage defects were recorded. Results: Common
inclusion criteria in the referred patients and patients included in the published RCTs were single femoral condyle lesion,
age range 18 to 40 years, and size of lesion range 3.2 to 4.0 cm2. Six of 137 referred patients matched all the 7 RCTs. Previous cartilage repair and multiple lesions were associated with decreased Lysholm score (P < 0.002). Lysholm score was
independent of age, gender, and time of symptoms from the defect. Conclusion: The heterogeneity of the referred cartilage
patients and the variation in inclusion criteria in the RCTs may question whether RCTs actually represent the general
cartilage patients. The present study suggests that results from published RCTs may not be representative of the gross
cartilage population.
whereasfor
Saris et al. included
than each of the 8referred
RCTs,
• All patients
the most, n = 118, and Horas et al. included 40 patients.
We thereforeevaluation
believe that we have included
cartilage
cartilage
to aenough
tertiary
patients to answer our study hypothesis.
We also performed
a power analysis on behalf of the stauniversity
clinic
tistical analysis. We wanted to simply match the characteristics of included patients with the same characteristics from
• Assessed
with
inclusion
the 8 RCTs. This
resulted
in a minimum ofcriteria
101 included
patients in this study. Figure 1 illustrates the inclusion of the
retrieved
from
8 RCTs
patients in this
present study.
In total, 46 women and 91 men were included, with
their ages ranging from 13 to 58 (median 37). Nine patients
• Of patients
with a verified
had bilateral lesions, 34 had been experiencing symptoms
for less than 10 months, and 75 had not been through either
defect
between
cartilage
repair or anterior7%
cruciateand
ligament80%
(ACL) reconIntroduction
struction previously, whereas 13 had not been through
would
have atbeen
inmaterial,
any intervention
the time ofeligible
inclusion. In this
65 patients had symptoms that could be related to one
each
RCT
specific
incident, and the defects were thereby classified
Keywords
cartilage defect, Lysholm, RCT, cartilage repair
• No clear picture
• No recent meta-analyses or Cochrane-reports
Identified Forms of Bias in Cartilage Research
Definition
Error in patient selection resulting in nonrepresentative or
fundamentally different treatment groups; may include
sampling bias, volunteer bias, and nonresponder bias
Form of selection bias that fails to account for the
outcomes of patients who do not respond or complete
follow-up
Systematic differences in the care provided to the patients
in the comparison groups other than the intervention
under investigation
Bias resulting from differential losses to follow-up
Detection
Eligibility is due to the matching patients from our included patients.
Better
outcomes
The choice?
1317
CLINICAL KNEE CARTILAGE RESEARCH
1110
Downloaded from ajs.sagepub.com at Oslo universitetssykehus. on March 3, 2014
may not represent general cartilage patients. The size of the
defects and the age of the patients may also result in excluPatients with articular cartilage injuries experience decreased
sion of patients in controlled studies. These limitations, which
mobility and pain, although their symptoms differ based on
are necessary to achieve a high internal validity
due to1.
theFlowchart of the inclusion of the patients in the study.
Figure
affected joint. These injuries affect a large number of
study design of RCTs, may naturally interfere with the exterRCT, randomized controlled trial.
patients. Studies have shown cartilage injuries in 66% of
nal validity and clinical applicability of them.
1,2
the patients
The present study was designed to evaluate the difference
as undergoing
acute. an arthroscopy for knee pain. In
evidence-based medicine, randomized controlled trials
between patients included in published RCTs and the total
We performed
an independent-samples
t test
onreferred
thosetowho
(RCTs) are perceived
as the gold standard
for evaluating
number of
patients
a major cartilage clinic. The
treatmentmatched
options. Still,the
onlycommon
3% to 6% of published
articlescriteria
study’s(after
main questions
were the following:
how well
cantotal
the
inclusion
excluding
the
The
number of patients not receiving any surgical
in orthopedics are RCTs.3 Several studies18with the aim to
RCT inclusion criteria be applied to our general cartilage
article of Horas et al. ) and those that
did not match. This
treatment at the end of this study was 7. We obtained
measure the outcome of cartilage repair have been performed
group, and are results from RCTs applicable when advising
yielded
a nonsignificant
P described
value (0.9).
information on cartilage lesion size, International Cartilage
during the
past decade.
Numerous articles have
1
good or excellent results, but the methodological quality has
Oslo Sports Trauma Research Center, Norwegian College
been questioned, as evident in an analysis of cartilage repair
of Sports Science, Oslo, Norway
2
Orthopaedic Centre, Oslo University Hospital, Ullevål and
studies from 2005.4
Faculty of Medicine, University of Oslo, Oslo, Norway
An issue that has been less discussed in the orthopedic
literature is the heterogeneity in etiology and the anatomical
Corresponding Author:
from car.sagepub.com
at Oslo
on June 3, 2014
locations of cartilage lesions. Patients with lesions in only
Cathrine Downloaded
N. Engen, OSTRC/NAR,
Sognsveien 220,
0863universitetssykehus.
Oslo, Norway
Email: c.n.engen@studmed.uio.no
one anatomical location resulting from one specific injury
Study design bias
T
#
2.
"
Presence of Bias in Selected Cartilage Studies
"
Gudas et
al.13,15
MOATS
v MFX
Gudas et
al.14
MOATS
v MFX
Knutsen et
al.20,21
ACI v
MFX
Saris et
al.25,26
CCI v
MFX
Visna et
al.33
OATS v
CP
""
#
#
"
#
#
#
""
#
"
"
"
#
#
""
#
#
#
"
#
"
#
"
"
#
#
"
#
"
"
#
"
"
#
#
NOTE. One plus sign denotes the presence of a particular form of bias within the study, 2 plus signs indicate the presence of a more
dence for evaluation, diverse methodology, inadehe current orthopaedic research in the field of
extensive
form ofHowever,
bias, and minus
sign denotes
the absence
orvarying
marginal presence of bias. ACI and CCI denote second-generation ACI.
cartilage restoration
is extensive.
quate follow-up,
strict government
guidelines,
CP, chondroplasty;
MACI, third-generation
autologous chondrocyte implantation; MFX, microfracture; MOATS,
evidence-based articularAbbreviations:
cartilage research conducted
regulatory environments,
and the numerous inherent
in randomized, controlled
prospective trials has
been
potential
biases faced
by investigators.
mosaicplasty-type
osteochondral
autograft
transfer
surgery;Furthermore,
NP, information required to make determination of bias is not provided; OATS,
limited by difficulties
in enrollment, conflicting
evi-transfer
the presence
of an isolated articular cartilage lesion of
osteochondral
autograft
surgery.
• All RCTs had substantial limitiation and biases
• “Op#mal management of car#lage defects is controversial”
• Very strict FDA-rules may limit the number of future RCTs
performed in the US
From St. Vincent’s Orthopedics (J.W.), Birmingham, Alabama; the Department of Orthopaedic Surgery and Rehabilitation, William
Beaumont Army Medical Center (B.R.W.), El Paso, Texas; Heiden Davidson Orthopedics (P.A.D.), Park City, Utah; and the Taos
Orthopaedic Institute (J.H.L.), Taos, New Mexico, U.S.A.
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Received October 20, 2011; accepted February 21, 2012.
Address correspondence to James H. Lubowitz, M.D., 1219 Gusdorf Rd, Ste A, Taos, NM 87571-6499, U.S.A. E-mail: jlubowitz@kitcarson.net
© 2012 by the Arthroscopy Association of North America. All rights reserved.
0749-8063/11686/$36.00
doi:10.1016/j.arthro.2012.02.022
Arthroscopy: The Journal of Arthroscopic and Related Surgery, Vol 28, No 9 (September), 2012: pp 1315-1325
1315
Downloaded from car.sagepub.com at Oslo universitetssykehus. on June 3, 2014
5
9/23/14
Eminence- or evidence-based medicine?
1779
• 75 % of patients reach a good clinical results regardless of the type of
T
J
B
&J
S
.
M
A
C
S
9 1-A N
7 J
2 009
D be expected!)
K
treatment (butV a normal
knee
cannot
HE
OURNAL OF
ONE
OINT
OLUME
d
U R G E RY
UMBER
d
d
JBJS ORG
U LY
U RGICAL
A NAGEMEN T O F
EFECTS IN THE
RTICULAR
A RT I L AG E
NEE
But?
Take home messages
The RCT(s) we are missing
CONSERVATIVE
( = training)
versus
SURGICAL
(= ?)
Patients with symptomatic lesions
without prior surgery
Long follow-up!
• Natural history is not clear
• Don´t forget that if early diagnosed
(especially young patients) fixation may be
an option
• No consensus on one treatment as superior
• Still relying on experts subjective
interpretations, but more and more highlevel evidence
• Methodology is improving – more RCTs are
done
• Training is an overlooked option
T. T. T.
Put up in a place
where it's easy to see
the cryptic admonishment
T. T. T.
When you feel how
depressingly
slowly you climb,
it's well to remember that
Things Take Time
Piet Hein
Fig. 1
MFX: microfracture.
OCA: osteochondral allograft. ACI: autologous chondrocyte
Treatment algorithm for focal chondral lesions. Before treatment, it is important to assess the
implantation.
OATS: mosaicplasty/ osteochondral autograft transplantation
presence of correctable lesions. Surgical treatment should be considered for trochlear and patellar
Cole, 2009
lesions only after use of rehabilitation programs has failed. The treatment decision is guided by the
size and location of the defect, the patient’s demands, and whether it is first or second-line treatment.
ACL = anterior cruciate ligament, PCL = posterior cruciate ligament, MFX = microfracture, OATS =
osteochondral autograft transplantation, ACI = autologous chondrocyte implantation, OCA = osteochondral allograft, AMZ = anteromedialization, 11 = best treatment option, and 12 = possible
option depending on patient’s characteristics.
cifically, patients often express concerns
about whether it is safe to remain active
despite symptoms and whether a delay in
surgical intervention precludes certain
treatment options because of disease
progression. In addition, knowledge of the
specific marginal improvements that a
procedure should provide gives the patient a reasonable expectation regarding
the outcome. Unfortunately, the lack of
understanding of the natural history of
these defects makes it difficult to advise
patients, and it is best to carry out careful
discussions on a case-by-case basis.
Patient age, body mass index,
symptom type (weight-bearing pain,
non-weight-bearing pain, swelling, mechanical symptoms, giving-way, and
aggravation of symptoms related to
walking on level ground as opposed to
stair-climbing), occupation and/or
family commitments, risk-aversion
(desire to avoid subsequent surgical
procedures), responsiveness and rehabilitation after previous surgical treatments, and the patient’s specific
concerns related to his or her problem
are all important preoperative considerations. While chronologic age is often
cited as a relative indication or contraindication to cartilage repair, it is really
physiologic age that determines the
patient’s eligibility for a non-arthroplasty
solution. Typically, patients who become symptomatic in the fourth or fifth
decade of life have concomitant chondral and subchondral disease involving
apposing articular surfaces that precludes a biologic treatment option. In
addition, the results of partial and total
knee arthroplasty are predictably gratifying and satisfy most patients, even
those who are relatively young. Finally,
one must carefully search for associated
pathological conditions, such as malalignment, ligament insufficiency, and
concomitant meniscal deficiency, that
may contribute to treatment failure and
should be corrected before or during the
surgery to treat the chondral lesion.
Defect-specific variables include
defect location, number, size, depth,
and geometry; the condition of the subchondral bone and surrounding cartilage;
and the degree of containment. The
condition of the apposing surface, which
is often overlooked, is also an important
variable. Even minor areas of early degeneration make achieving a satisfactory
clinical outcome challenging. Specific
management of each of these defectspecific variables increases the likelihood
of a good clinical outcome.
Fakta om brusk behandling
– Rehablitering kan i mange tilfeller gi like bra
resultat som kirurgi
– Mikrofraktur er ikke bra sammen med ACL
kirurgi
– Store skader behandles best med
Celletransplantasjon
– Chondrale frakturer kan i mange tilfeller
festes tilbake
Aktuelle scenarioer
Svømmer 12 år-fulgt i to år
• Ung idrettsutøver med knesmerter over lang tid
• Økende knesmerter over 3-4 år
• MR viste bilaterale OCD forandringer
• Behandlet med ro og avlastning i tre måneder
• Retur av smertene etter aktivitetsøkning
• Høyre kneet som var værst ble behandlet med arthroscopi og
oppboring
• Kontroll nå, ingen smerter I høyre kne, men av og til litt ubehag i
venstre kneet, bestilt ny MR
• Voksen idrettsutøver med kjent leddbruskskade
• Kombinert med annen kne skade som ligamentskade
ACL,MCL,PCL,MPFL
• Chondral fractur
• Artroseutvikling
A- Fotballspiller-elitenivå
B-Fotballspiller elitenivå
C-Fotballspiller på vei mot elitenivå
• OCD forandring i venstre kne
• Langvarig problem med kneet etter kollisjonsskade
• Økende smerter og ubehag med kneet
• MR viste menisk + bruskskade
• Arthroskopert
• Skopert behandlet meniskskaden og stabilisert bruskskaden
• Fjernet OCD 10 mm stabilisert bruskskade
• Retur til full aktivitet i løpet av få måneder
• Knesmerter over 3-4 år
• MR viste en OCD som innbefatter store deler av mediale
femurcondyle
• Skopert og festet arthroskopisk med Herbert Whippel skruer
• Tilbake og spilte på toppnivå etter 1 år
• Økende plager og ubehag
• Skopert på nytt-desverre viste det seg OCD fragmentet var gått i
oppløsning
• Rehabiliteres
• Skal vurderes i forhold til celletransplantasjon
• Opptrening 9 måneder
• Retur til elitenivå men merker problem med kneet
6
9/23/14
ACL skade og bruskskade
ACL skade og bruskskade
• Aktiv håndballspiller
Patella luksasjon
• Bruskskader i 97 % av de med
gjentatte patellaluksasjoner
• Vridningstraume
• ICRS grad 3-4 I 37 %
• ACL skade med fritt fragment
• Rekonstruksjon av ACL skaden
• Fjernet fritt fragment
• Gitt seg med håndball
• Velfungerende kne
• OsteoChondrale og chondral
frakturer forekommer ofte
sammen med patella luksasjoner
• Mistanke om dette en av de få
indikasjonene for MR i løpet av få
dager
Straume Nesheim et al 2014
Bevare det som er mulig Hvordan fiksere et slikt fragment
Hvordan fiksere et slikt fragment
7
9/23/14
Hvordan fiksere et slikt fragment
Hvordan fiksere et slikt fragment
Praktisk tips
• Aldri metall skruer på
patella/trochlea
Praktisk tips
• Aldri metall skruer på
patella/trochlea
Hvordan kan vi best håndtere disse skadene som idrettslege
• OCD hos pasient i vekst
– Igangsette fullstendig ro og avlastning 3
måneder
• Chondral fragment
Take home message
• Vi kan ikke ennå gjenskape normal brusk
• Et godt resultat ved bruskkirurgi er en Lysholm på 75 poeng, kan
sykle, gå klassisk langrenn, svømme crawl uten problem samt at
det går rimelig bra i dagliglivet
Henvise til brusksenter d.v.s som gjør
bruskcelletransplantasjon
• ACL skadet kne
– Ikke mikrofraktur
• Store lesjoner og stabilt kne
– Henvise til vurdering ACI
8
9/23/14
Brusk i forskning
Bruskkirurgiens tre hovedregler
Hva har vi lært ?
• Stabiliser kneet
• Beinmargsstimulerende prosedyrer som f.eks mikrofraktur gir
permanente forandringer subchondroalt lik begynnende artrose
• Korreksjon av kneakse (HKA maks 5 grader)
• Bruskkirurgi kun med forberedt og fullt rehabilitert pasient
Hva har vi lært ?
Hva har vi lært ?
Hva har vi lært ?
• Beinmargsstimulerende prosedyrer som f.eks mikrofraktur gir
permanente forandringer subchondroalt lik begynnende artrose
• Lokalisasjonen av bruskdefekten er av betydning i
eksperimentelle modeller
• Beinmargsstimulerende prosedyrer som f.eks mikrofraktur gir
permanente forandringer subchondroalt lik begynnende artrose
• Lokalisasjonen av bruskdefekten er av betydning i
eksperimentelle modeller
• Periost-mikrofraktur-mosaikk er like dårlig eller bra
• Beinmargsstimulerende prosedyrer som f.eks mikrofraktur gir
permanente forandringer subchondroalt lik begynnende artrose
• Lokalisasjonen av bruskdefekten er av betydning i
eksperimentelle modeller
• Periost-mikrofraktur-mosaikk er like dårlig eller bra
• Periostlappen sitter kun i to uker
Hva har vi lært ?
Hva har vi lært ?
Hva har vi lært ?
• Beinmargsstimulerende prosedyrer som f.eks
mikrofraktur gir permanente forandringer
subchondroalt lik begynnende artrose
• Lokalisasjonen av bruskdefekten er av
betydning i eksperimentelle modeller
• Periost-mikrofraktur-mosaikk er like dårlig eller
bra
• Periostlappen sitter kun i to uker
• Mesenchymale stamceller er et mulig
alternative for denne type kirurgi
• Beinmargsstimulerende prosedyrer som f.eks
mikrofraktur gir permanente forandringer
subchondroalt lik begynnende artrose
• Lokalisasjonen av bruskdefekten er av betydning i
eksperimentelle modeller
• Periost-mikrofraktur-mosaikk er like dårlig eller bra
• Periostlappen sitter kun i to uker
• Mesenchymale stamceller er et mulig alternative for
denne type kirurgi
• Bruskcellene liker best autologt serum i dyrknings
prosedyren
• Beinmargsstimulerende prosedyrer som f.eks
mikrofraktur gir permanente forandringer
subchondroalt lik begynnende artrose
• Lokalisasjonen av bruskdefekten er av betydning i
eksperimentelle modeller
• Periost-mikrofraktur-mosaikk er like dårlig eller bra
• Periostlappen sitter kun i to uker
• Mesenchymale stamceller er et mulig alternative for
denne type kirurgi
• Bruskcellene liker best autologt serum i dyrknings
prosedyren
• Bruskcellene produserer mer brusksubstanser ved
biomekanisk stimulering
9
9/23/14
Bruskkirurgi krever
• Gode artroskopi ferdigheter/
ligamentkirurgi
• Utmerket bildediagnostikk
• Rehabiliteringsfokus
• Cellelaboratorium
• Bruskpatolog
• Osteotomikunnskaper
• Protesekirurgi
Fremtiden ?
• Samarbeid
– Andre sykehus
– NAV
– Industrien
• Pasientomland
• Tid
10