Reproductive System
Anatomy & Physiology
Be Mature
• Use proper anatomical terms
• Joe Ask meaningful and RELAVANT questions
Reproductive FXN
• Only body system not responsible for homeostasis
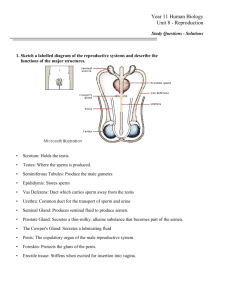
Male Reproductive Anatomy
Testes: produce male sperm and testosterone)
Sperm: male reproductive cells that contribute X and Y chromosomes
Seminiferous tubules: produce sperm
Scrotum: pouch of skin that holds the testes. Scrotal skin lengthens
and shrinks to maintain sperm temperature
Vas deferens: tubes that transport sperm from the testes to the
ejaculatory ducts; site where vasectomy (sterilization) occurs
Semen: fluid ejaculated during sexual arousal. Made up of sperm
(from testes), fluid for sperm nutrition (from seminal vesicle), and
“milky white” fluid for semen odor and texture (from Prostate
gland)
Male Reproductive Anatomy
Urethra: tube that passes urine and semen out of the
body. Also the entry point in males for STDs.
Note: semen and urine do not pass through the urethra at
the same time.
Glans penis: sensitive tissue on the head of the penis with
purpose for sexual stimulation.
Epididymis: superior to each testis; tubular (5-6 m);
maturate sperm (takes 20 days for sperm to travel
through)
Male Reproductive Anatomy
Seminal Vesicles: posterior to the urinary bladder;
secrete yellowish viscous alkaline fluid containing
fructose, vitamin C, and coagulating enzymes
Prostate Gland: inferior to the urinary bladder; produces
milky white fluid which activates sperm
Bulbourethral gland: inferior to the prostate gland; thick
clear ejaculate fluid which neutralizes traces of acidic
urine in the urethra
Testicles location in the
scrotum
• To keep sperm 2-3˚C for their survival; loaded
with melanin for U.V. protection
• Cremaster muscle contracts to raise the
scrotum closer to the body when cold, muscle
relaxes scrotum when warm
• Leydig cells: produce testosterone
Penis
• Copulatory organ found anterior and
external to the abdominopelvic cavity
• Corpora cavernosa engorge with blood
during an erection
• Corpora spongiosum surrounds the urethra
and expands distally to form the glans
(head of penis)
• Prepuce (Foreskin); can be removed
(Circumcision)
Spermatogenesis
How an erection forms
• Nitric oxide (NO) is released by the
parasympathetic nervous system during
arousal causing vasodilation; Blood becomes
engorged as the erection compresses
drainage blood vessels, thereby retarding
the outward flow of blood
Ejaculate
• The seminal vesicles, prostate gland, and
bulbourethral gland produce semen which transports
and protects sperm optimally to the female vagina
• Semen provides sugar for sperm and a base media to
protect against an acidic environment in the male
urethra and female vagina
• Sperm are produced at a rate of 1 000 every second
• Acrosome at the tip of the head releases enzyme to
enter the oocyte
Female Reproductive Anatomy
Ovary: produce female eggs/ovum as well as
estrogen & progesterone
Ovum (Egg): female reproductive cells that
contribute X chromosomes.
Fallopian tubes (Oviducts): tubes that transport
ovum to the uterus; passageway where
fertilization occurs; site of ectopic pregnancy;
site where tubal ligation (sterilization) occurs.
Female Reproductive Anatomy
Uterus: also known as the “womb” when an egg is
fertilized and implants in the lining of the uterus;
when no fertilized egg is present the lining of the
uterus sheds for the menstrual cycle.
Cervix: lower end of the uterus; an opening between
the uterus and vagina that passes sperm,
menstrual fluid, and a fetus.
Vagina: pathway for menstrual flow, birth canal,
sperm, and STDs. Opening for sexual intercourse
and contains vaginal secretions/lubrication.
Female Reproductive Anatomy
Urethra: opening for urine.
Clitoris: sensitive tissue with sole purpose
for sexual stimulation.
The maturation of a follicle
Primary follicle becomes a secondary follicle when
a fluid filled cavity forms.
A secondary follicle becomes a Graafian follicle
when the oocyte sits on a stalk.
Ovulation occurs and the oocyte is ejected from
the follicle. The follicle post ovulation becomes
the corpus luteum* (Yellow body) which
degenerates.
*The corpus luteum secretes progesterone which
thickens the uterus lining in preparation of the
fertilized egg
Fimbriae
The cilia of the fimbriae beat and
create a current in peritoneal fluid.
Without this current the oocyte could
be lost into the peritoneal cavity
(The fallopian tubes do not directly
connect to the ovaries)
Ectopic pregnancy
Occur when the oocyte is fertilized and it
doesn’t enter the fallopian tube, but enters
the peritoneal cavity.
Dangerous because it often leads to severe
bleeding (from the aborted fetus) and
peritoneal infection. PID could result from
this infection and could lead to sterility
(Compression of the oviducts) and possibly
death from peritonitis.
Uterus
• A hollow, thick walled organ which
receives, retains, and nourishes a zygote.
• The fundus is superior to the uterus and
the cervix (Cervical canal) is inferior to
the uterus.
• The function of the uterus is to receive
and implant the zygote
External Genitalia: Vulva (Pudendum)
Lies external to the vagina and includes the mons pubis,
labia, clitoris, and vestibular structures
• Mons pubis – round, fatty area overlying the pubic
symphysis
• Labia majora – elongated, hair-covered, fatty skin folds
homologous to the male scrotum
• Labia minora – hair-free skin folds lying within the labia
major: homologous to the ventral penis
External Genitalia: Vulva (Pudendum)
Greater vestibular glands
• Pea-size glands flanking the vagina
• Homologous to the bulbourethral glands
• Keep the vestibule moist and lubricated
Clitoris
• Erectile tissue hooded by the prepuce
• Homologous to the penis
Mammary Glands
• Modified sweat glands consisting of 15-25 lobes
that radiate around and open at the nipple
• Areola – pigmented skin surrounding the nipple
• Suspensory ligaments attach the breast to
underlying muscle fascia
• Lobes contain glandular alveoli that produce milk
in lactating women
• Compound alveolar glands pass milk to lactiferous
ducts, which open to the outside
Menses
• If fertilization does not occur, progesterone levels
fall, depriving the endometrium of hormonal support
• Spiral arteries kink and go into spasms and
endometrial cells begin to die
• The functional layer begins to digest itself
• Spiral arteries constrict one final time then suddenly
relax and open wide
• The rush of blood fragments weakened capillary
beds and the functional layer sloughs
Uterine (Menstrual) Cycle
Series of cyclic changes that the uterine
endometrium goes through each month in
response to ovarian hormones in the blood
•
Days 1-5: Menstrual phase – uterus sheds all
but the deepest part of the endometrium
•
Days 6-14: Proliferative phase –
endometrium rebuilds itself
•
Days 15-28: Secretory phase – Endometrium
prepares for implantation of the embryo
Female Sexual Response
The clitoris, vaginal mucosa, and breasts engorge with
blood
Vestibular glands lubricate the vestibule and facilitates
entry of the penis
Orgasm – accompanied by muscle tension, increase in
pulse rate and blood pressure, and rhythmical
contractions of the uterus
Females do not have a refractory period after orgasm
and can experience multiple orgasms in a single sexual
experience**Orgasm is not essential for conception
Sexually Transmitted
Diseases
Gonorrhea
Bacterial infection spread by contact with genital, anal,
and pharyngeal mucosal surfaces
Signs and symptoms:
• In males – painful urination, discharge of pus from the
penis
• In females – none (20%), abdominal discomfort, vaginal
discharge, abnormal uterine bleeding
• Left untreated, can result in pelvic inflammatory
disease
•
Treatment: antibiotics, but resistant strains are
becoming more prevalent
Sexually Transmitted Diseases
Syphilis
•
•
•
•
•
•
Bacterial infection transmitted sexually or
contracted congenitally
Infected fetuses are stillborn or die shortly after
birth
A painless chancre appears at the site of infection
and disappears in a few weeks
Secondary syphilis shows signs of pink skin rash,
fever, and joint pain
A latent period follows, which may progress to
tertiary syphilis characterized by gummas (CNS, blood
vessel, bone, and skin lesions)
Treatment: penicillin
Sexually Transmitted
Diseases
Chlamydia
•
•
Most common STD in the U.S.
Responsible for 25–50% of all diagnosed cases
of pelvic inflammatory disease
•
Symptoms include urethritis; penile and vaginal
discharges; abdominal, rectal, or testicular pain;
painful intercourse; and irregular menses
•
Can cause arthritis and urinary tract infections
in men, and sterility in women
•
Treatment is with tetracycline
Sexually Transmitted
Diseases
Viral Infections
Genital warts – caused by human papillomaviruses (HPV);
infections increase the risk of penile, vaginal, anal, and
cervical cancers
Genital herpes – caused by Epstein-Barr virus type 2 and
characterized by latent periods and flare-ups
• Congenital herpes can cause malformations of a fetus
• Has been implicated with cervical cancer
• Treatment: acyclovir and other antiviral drugs