Connective Tissue
advertisement

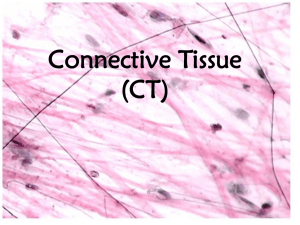
Connective Tissue HKIN 473 Group Members: Amy Chu Jesse Godwin Hale Loofbourrow Scott Apperley Greg Kirk Ken Anderson Overview Introduction to Connective Tissue Tendons Ligaments Cartilage Conclusion Introduction Connective tissues are situated around the body and play numerous roles Components common to connective tissue – Collagen Fibers Most abundant (parallel in arrangement) Stronger than steel – Reticular Fibers Criss-cross – Elastic Fibers Slightly elastic Tendons Tendons: Function Primary Function – Attach muscle to bone thereby transmitting tensile loads from muscle to bone to produce movement. Secondary Function – Allows the muscle belly to be at an optimal distance from the joint upon which it acts. Tendons: Anatomy 86% collagen fibers making them very strong The connective tissue that runs the length of the muscle joins together into a bundle of connective tissue, forming the tendon Tendons: Physiology Biomechanical Properties of Tendons – 4 regions of the graph (1) concave or “toe,” region. Results form change in the wavy pattern of relaxed collagen fibers which become straighter as the load progresses. Little force is required to elongate tissue initially. (2) linear region. The fibers straighten out and stiffness of the specimen increases rapidly. Tendons: Physiology (con’t) (3) End of linear relation. When the linear region is surpassed major failure of the fiber bundles occurs. Small force reductions in the curve represent early sequential failure of a few greatly stretched fiber bundles. (4) Maximum load, expressing the ultimate tensile strength of the tissue. Complete failure of the tissue to resist load. Tendons: Injury The amount of force that the muscle, which the tendon is attached to, can generate and the cross sectional area of the tendon are the major factors in predicting injury. When subjected to loading that exceeds the physiological range, micro-failure takes place even before the yield point is reached. If muscle contracted, the stress on the tendon can be greatly increased with a rapid eccentric contraction. Tendons: Viscoelastic Behavior Display rate-dependent behavior under loading (mechanical properties change with different rates of loading). The linear portion of the stress strain curve becomes steeper with increased loading rates. (ie, there is a higher level of stiffness at higher strain rates) With these higher strain rates, tendons can store more energy, require more force to rupture, and undergo greater elongation. Tendons: Adaptations Factors that affect the mechanical properties of tendon include: a) Maturation and Aging directly related to quality and number of collagen cross links b) Pregnancy tendons and pubic symphysis c) Mobilization and Immobilization d) NSAID’s short term administration after injury thought to increase rate of biomechanical restoration of tissue. Ligaments Ligaments: Function Tough, white, fibrous, slightly elastic tissues Connect bone to bone Supporting and strengthening joints Restrict range of motion to prevent excessive movement that could cause dislocation and spraining Ligaments: Anatomy Ligaments and tendons are regular dense collagen bundles – The collagen fibers are closely packed and arranged in parallel to give higher tensile strength – Ligaments are strongest with forces parallel to the fiber arrangement (along axis of the fibers) Highly avascular – Heal slowly Very similar to tendons Ligaments: Examples Ligaments: Sprains Can be caused by the severe stretching or tearing or a ligament Often caused by twisting or wrenching movement Symptoms: pain, swelling, and sometimes bruising Treatment: immediate cold compress and elevation, long term bandaging and/or splinting – In rare cases, surgery my be a useful alternative Full recovery may take up to 5 weeks Cartilage Cartilage: Anatomy • Dense network of collagen and elastin fibers • Fibers are embedded in a ground substance of chrondroitin sulfate • Collagen provides strength • Elastin provides elasticity • Cartilage is an avascular tissue Cartilage: Types Three primary types based on proportion of chondrocytes, elastin fibers and collagen fibers 1. Fibrocartilage 2. Elastic Cartilage 3. Hyaline Cartilage 1. Firbrocartilage Large proportion of collagen fibers Provides strength and support Found in the pubic symphysis, intervertebral discs, menisci of the knee Source: Polychondritis Educational Society, Ltd 2. Elastic Cartilage Chondrocytes reside in a “threadlike network” provided by elastic fibers Provides strength and elasticity while maintaining shape Found in the epiglottis and external ear Source: Polychondritis Educational Society, Ltd 3. Hyaline Cartilage Most abundant cartilage composed of fine collagen fibres with many chondrocytes Provides flexibility and support Found in the nose, larynx, bronchi, trachea and on the anterior ends of ribs Source: Polychondritis Educational Society, Ltd Cartilage: Endochondral Ossification A further function of Hyaline Cartilage is in the formation of long bones Starting in the fetus, cartilage calcifies until full bone growth has been achieved, typically at the age of 25 Tortora & Grabowski, 2000 Articular Cartilage Hyaline or Fibrocartilage found in joints on the articulating surfaces of bones Provides a smooth, slippery surface that reduces friction and absorbs shock in joints Tortora & Grabowski, 2000 Cartilage: Osteoarthritis Painful condition in which the articular cartilage between bones degenerates 11% of people older than 64 years old experience symptoms of osteoarthritis Glucosamine and chondroitin sulfate have been found to relieve some pain symptoms Cartilage: Knee Menisci The medial and lateral menisci are wedge-like cushions of fibrocartilage found in the knee joint between the tibia and femur Knee menisci provide stability, support in carrying weight and allow movement in many directions American Academy of Orthopaedic Surgeons, 2001 Cartilage: Meniscal Tears Damage to the menisci can occur in decelerating, twisting, cutting or pivoting Meniscal tears may cause loss of range of motion, pain, stiffness and knee locking Meniscal injuries are hard to heal because of the absence of blood supply Meniscal injuries may require surgical treatment Thank You