Red blood cells medical powerpoint template
advertisement

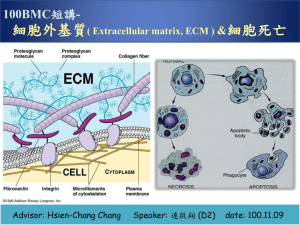
ARTICULAR CARTILAGE STRUCTURE, INJURY & HEALING Nadhaporn Saengpetch Division of Sports Medicine, Department of Orthopaedics, Faculty of Medicine Ramathibodi Hospital, Mahidol University COMPOSITION • Extracellular matrix and sparse cells • No blood vessel, lymphatic vessel and nerve • limit response to any metabolic response • Frictionless CHONDROCTYE • Endoplasmic reticulum and Golgi apparatus (matrix synthesis) • Intracytoplasmic filament, lipid, glycogen, secretary vesicles (maintenance of matrix structure) CHONDROCYTE: DIFFERENT BY LAYERS • Surface layer: elongated and resemble fibroblasts • Transitional layer: round and actively for chemistry • Deeper layer: cells in radial pattern • Tidemark: non-functional cells COLLAGEN FIBRILS CHONDROCYTE: FUNCTION • NOT participate in water distribution • Maintenance and structural competence • Producing and replacing appropriate macromolecules (degradation, mechanical demand placed on the surface, synthesizing) • Assembling as an highly ordered framework CARTILAGE ZONES EXTRACELLULAR MATRIX (ECM) • 2 components 1. Tissue fluid 2. Framework of structural macromolecule • Interaction -> stiffness and resilience ECM • Water 80% by weight • Gel forming = lubrication system • Large aggregation of Proteoglycans (maintain fluid within the matrix and e’lyte concentration) ECM MOVEMENT Na+ Cl Cl - Na+ - STRUCTURAL MACROMOLECULES STRUCTURAL MACROMOLECULES • Collagens • Proteoglycans • Noncollagenous proteins 20-40% wet wt. Glycoprotein 15% Proteoglycan 25% Collagen 60% COLLAGEN • • • • 60% of dry weight of cartilage Collagen-rich superficial zone Types: II*, VI, IX, X and XI Type II, IX and XI form the cross-band fibrils TIGHT MESHWORK Collagen fibrils organization Large proteoglycans entrapment Tensile stiffness & cartilage strength Cohesiveness of tissue TYPE II COLLAGEN • 90-95% of cartilage collagen • The primary component of cross-banded fibrils TYPE VI COLLAGEN • Forms an important part of surrounding chondrocytes • Helps chondrocyte attach to matrix TYPE IX COLLAGEN • Bind covalently to superficial layers of cross-banded fibrils • Project into the matrix to bind with other Type IX Collagen and Proteoglycans TYPE X COLLAGEN TYPE XI COLLAGEN • Found only near • Bind covalently to cartilage calcified Type II zone and • May form part of hypertrophic zone interior structure of of growth plate cross-banded fibrils (start to mineralize) • Cartilage mineralization PROTEOGLYCANS • A protein core & Glycosaminoglycans (GAG) chains (unbranched polysaccharide) • GAG: Hyaluronic acid, chondroitin sulfate, glucosamine sulfate, dermatan sulfate ARTICULAR PROTEOGLYCAN Aggrecans* (large) Decorin Biglycan Fibromodulin (small) AGGRECANS • • • • Mostly fill in the interfibrillar space of matrix 90% of Pg mass Noncovalently bind with HA & monomer Help anchor Pg in the matrix, prevent displacement during deformation, organize and stabilize Pg & collagen DECORINS • One dermatan sulfate chain BIGLYCAN & FIBROMODULIN Biglycan • Two dermatan sulfate chains Fibromodulin • Several dermatan sulfate chains ARTICULAR PROTEOGLYCAN Aggrecans* (large) - Healing + Degradative enzymes Transforming growth factor β Decorin Biglycan Fibromodulin (small) HYALURONIC ACID • Backbone for matrix aggregation • Bind aggrecans non-covalently and link proteins • This aggregation helps anchor Pg within the matrix • Prevent displacement during deformation • Stabilize relationships of Pg and collagen meshwork NONCOLLAGENOUS PROTEINS & GLYCOPROTEINS • Stabilize the matrix framework • Help chondrocytes bind to the macromolecules of matrix • Anchorin CII collagen-binding chondrocytes surface protein (anchor) • Cartilage oligomeric protein (COMP) is in chondrocyte territorial matrix, have capacity to bind to chondrocyte ZONES OF ARTICULAR CARTILAGE SUPERFICIAL ZONE • Thinnest zone • Two sub layers: – sheet of fine fibrils (acellular) – flattened ellipsoid-shape chondrocyte + fibroblast • Collagen is lying parallel to the joint surface (resist compressive force)-> OA • High collagen, low Pg • “cartilage skin” TRANSITIONAL ZONE • Large volume • cells: synthetic organelles (ER, Golgi) spheroidal shape • Lower collagen & water concentration • Higher Pg concentration MIDDLE(RADIAL/DEEP) ZONE • Chondrocytes align in columns perpendicular to the joint surface (resist shear stress) • Largest diameter collagen • Highest Pg • Lowest water • Collagen fibers pass into the tidemark CALCIFIED CARTILAGE ZONE • Thin calcified cartilage • “calcific sepulchers” • Extremely low level of metabolic activity • No nutrients traverse this zone MATRIX REGIONS • Pericellular • Territorial • Bind cell membranes to matrix macromolecules • Protect deformation force • Transmit mechanical signals to chondrocytes • Interterritorial >>> • Provide the mechanical properties of tissue CHONDROCYTE-MATRIX INTERACTIONS • Matrix protects chondrocytes from mechanical damage and maintain shape and phenotype • Matrix : metabolic products/cytokines and growth factors • Insulin-dependent growth factor I (IGF-I) & Transforming growth factor β (TGF β) + matrix synthesis & cell proliferation CHONDROCYTE-MATRIX INTERACTIONS + IGF-I TGF β BIOMECHANICS Tension Compression Shear • Wide range of static & dynamic mechanical loads • Compressive, tensile & shear forces α composition & structure of ECM TENSILE & SHEAR FORCE • These forces are resisted by ropelike collagen fibrils COMPRESSIVE FORCE • Resisted by highly charged GAG such as aggrecan molecules LOADING vs IMMOBILIZATION Induced wide range of metabolic response Decreased in matrix synthesis CARTILAGE REGENERATION Static compression Cyclical compressive Reversibly inhibit cartilage matrix synthesis Stimulate aggrecan core protein & protein synthesis DEGENERATION AND OSTEOARTHRITIS • Osteoarthritis >> degenerative joint disease, degenerative arthritis, hypertrophic arthritis HOW THEY CHANGE? OA: 3 OVERLAPPING PROCESSES 1. Cartilage matrix damage 2. Chondrocyte response to tissue damage 3. Decline of the chondrocyte synthetic response STAGE 1 MATRIX DAMAGE Water Aggrecan & GAG length Permeability & Matrix stiffness Other causes: inflammation, tissue’s metabolic changes that interferes matrix maintenance STAGE 2 CHONDROCYTE RESPONSE • Chondrocytes detect tissue damage Catabolic enzymes (proteases) Anabolic & mitogenic growth factors + chondrocyte proliferation & ECM Reversible - Spontaneous - Intervention STAGE 3 DECLINE CELL SYNTHESIS • Failure to restore the tissue • Progressive loss of cartilage • Down regulation of chondrocyte response to anabolic cytokine JOINT INJURY & POSTTRAUMATIC OA • Ligament reconstruction (ex. ACL-R) can restore mechanical stability but not greatly reduce the risk for OA development because…. The initial traumatic event may have irreversible effects on the joint tissues and residents cells Good Luck