اندیکاسیون سزارین از دیدگاه پروکتولوژیست
دکتر رسول عزیزی
جراح کولورکتال ،دانشیار گروه جراحی
دانشکده پزشکی دانشگاه علوم پزشکی ایران
مجتمع رسول اکرم ،بخش جراحی
E-mail:razizimd@hotmail.com
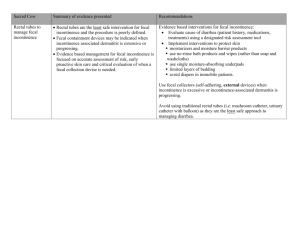
Anatomy & physiology of continence
introduction
The ability
to retain a bodily discharge voluntarily”. The
word has its origins from the Latin continere or
tenere, which means “to hold”. The anorectum is the
caudal end of the gastrointestinal tract, and is
responsible for fecal continence and defecation. In
humans, defecation is a viscero somatic reflex that is
often preceded by several attempts to preserve
continence
Mechanisms of Continence and Defecation
Risk Factors in Fecal Incontinence
Obstetric Events
*Sphincteric Injury
*Pudental Nerve Injury
*Secondary Rectal Sensorimotor
Dysfunction
There is now clear recognition, supported
by a considerable body of evidence, that
Obstetric trauma is, by far, the major risk
factor for the development
of acquired fecal incontinence in women
KAMM MA (1994) OBSTETRIC DAMAGE AND FECAL INCONTINENCE.
LANCET 344:730
BHARUCHA AE (2003) FECAL INCONTINENCE. GASTROENTEROLOGY
124:1672-1685
In a frequently
referenced study by Sultan and
colleagues in 1993,ultasound at 6 weeks
postpartum revealed sphincter injuries
in 35% of primiparous women and 44%
of multiparous women.
Sultan AH, Kamm MA, Hudson CN et al
(1993) Anal sphincter
disruption during vaginal delivery. N Eng J
Med 329:1905–1911
1-Chaliha C, Kalia V, Stanton SL et al (1999) Antenata
prediction of postpartum urinary and fecal incontinence
Obstet Gynecol 94:689-694
MacArthur C, Glazener CM, Wilson PD, et al(2001) Obstetric practice and faecal
incontinence three months after delivery. BJOG 108:678-683
MacArthur C, Bick DE, Keighley MR (1997) Faecal
–incontinence after childbirth. Br J Obstet Gynaeco104:46-50
THE PREVALENCE OF
SYMPTOMS OF FECAL INCONTINENCE POSTPARTUM IN
STUDIES INVOLVING >130 SUBJECTS AND SHOWS THAT
GREATER THAN 10% OF WOMEN WILL COMPLAIN OF
BOWEL
SYMPTOMS IN THE FIRST FEW MONTHS FOLLOWING
CHILDBIRTH
Oberwalder and colleagues performed a meta-analysis
of 717 vaginal deliveries has three
notable results: First, the incidence of anal sphincter
defects in primiparous women was 26.9%. Second,
multiparous women had an 8.5% incidence of new
sphincter defects. Third, the calculated probability
that postpartum fecal incontinence was due to a
sphincter defect was 76.8–82.8%.
Oberwalder M, Connor J, Wexner SD (2003)
Metaanalysis
to determine the incidence of obstetric anal
sphincter damage. Br J Surg 90:1333–1337
Episiotomy was at one time believed to be protective
to the perineum during childbirth and was used
to prevent the occurrence of third- and fourth-degree
tears . There is now evidence that episiotomy not
only fails to protect the perineum but has been
associated with increased tearing and anal sphincter
injury
1-Thacker SB, Banta HD (1983) Benefits and risks of episiotomy:
an interpretive review of the English language literature. Obstet Gynecol Surv
38:322–338
2-Klein MC, Gauthier RJ, Robbins JM et al (1994) Relationship of episiotomy to
perineal trauma and morbidity, sexual dysfunction, and pelvic floor relaxation.
Am J Obstet Gynecol 171:591–598
Many papers have been published
regarding
obstetric lesions as they relate to
incontinence. However,
it is difficult to accurately quantify the
prevalence
of obstetric injury and its effect on the
incidence
of incontinence.
In addition to direct trauma to the sphincter muscle,
pudendal neuropathy is another consequence of
vaginal delivery, which contributes to fecal
incontinence.
The pudendal nerve is believed to be damaged
by the fetal head, which compresses the nerve,
causing
ischemia or stretching its branches
repeated pregnancies and deliveries add
to the damage, the neuropathy progresses as the
woman ages, and the worsening over time causes significant
fecal incontinence that presents between 50
and 60 years of age
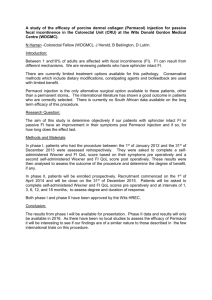
Cesarean section has been advocated as an option
to protect the pelvic floor and reduce the incidence of
postpartum fecal incontinence; however, this issue is
controversial. Cesarean section performed after
cervical dilation, especially if performed late in the
second stage of labor, is not entirely protective
against direct sphincter trauma or pudendal
neuropathy
At this time, the best practice seems to be evaluation of a
woman’s risk factors, informed consent regarding
her risk of pelvic floor trauma from vaginal delivery,
proper recognition of injury at the time of delivery
, and effective postpartum evaluation
Nelson et al. covering 15 studies encompassing
3,010 Caesarean section and 11,440 vaginal deliveries
showed no difference between the rate of either fecal or
flatus incontinence between the two different modes of
delivery. The implication of both of these studies is that it is
pregnancy itself, perhaps in relation to connective tissue
properties or perhaps an inherited susceptibility, that can
lead to pelvic floor disorders.
Nelson RL, Westercamp M, Furner SE (2006)A
systematic review of the efficacy of Cesarean
section in the preservation of anal continence. Dis
Colon Rectum49:1587-1595
Risk Factors
Anorectal Anomalies •
Spina Bifida •
Isolated Sacral Agenesis •
Hirschprung’s Disease •
Cerebrovascular Accidents •
Parkinson's Disease •
Multiple Sclerosis •
Spinal Cord Injury •
Diabetes Mellitus •
Ageing •
Inflammatory Bowel •
Disease
Irritable Bowel Syndrome •
Anal Surgery •
Rectal Resection •
Rectal Evacuatory •
Disorder
Rectal prolapse •