Gotta Go? Gotta Go!
Gotta GO!!!
Discussion of Urinary and Fecal
Urgency, Frequency, and
Incontinence
Elizabeth Babin, MD
Female Pelvic Medicine and Reconstructive Surgeon
Director, Athena Women’s Institute for Pelvic Health
Professor Drexel University Department of
Urogynecology
Select the most appropriate
subtitle for this talk
A: Bladders gone wild!
B: There’s no such thing as bad bladders, they
just do bad things…
C: Your system software has been corrupted.
Do you have the right driver installed for that
bladder?
D: I’m going to go crazy if I have to find another
potty
Learning Objectives
Review
definition, causes, and treatments
for:
urinary urgency, frequency, and urinary
incontinence
recurrent urinary tract infections
fecal incontinence
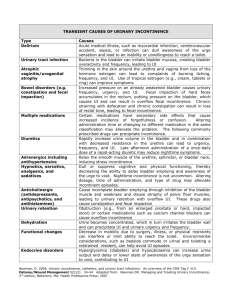
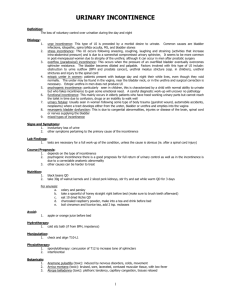
General Definitions
Urgency: sudden compelling sensation to pass urine or
feces which is difficult to defer
“Gotta Go”
Primary symptom of overactive bladder or bowel
Frequency: excessive number of voids or movements
over a 24 hour period
Urinary Incontinence: involuntary loss of urine
Fecal Incontinence: involuntary loss of gas or feces
Recurrent Urinary Tract Infections (UTIs): >2 bladder
infections proven by urine culture in a 6 months period
Incontinence is a
Common Problem
1:3 women over age 45
Which is over 13 million women
1:2 women over age 65
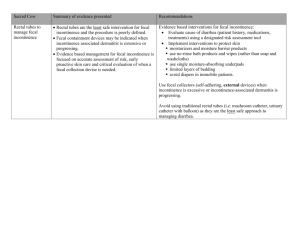
Anatomy Review
Bladder:
stores
urine
Urethra: tube that
allows urine to pass
Urethral sphincter:
muscle surrounding
the urethra that hold
the urine
Brain signals are
key to coordinating
the function of these
anatomical
structures
Anatomy Review
What is Overactive Bladder?
It is a combination of symptoms that may or
may not include involuntary loss of urine that
are the result of the brain miscommunicating
with the bladder (nerve inputs leading to
abnormal sensations and/or muscle reactions)
Urgency
Frequency
Leakage
“I get an urge to urinate that causes me to frequently
search for the bathroom and sometimes I don’t make
it!” Gotta go!!
OAB Treatments
Behavioral
Modification
Lifestyle changes, dietary avoidance, timed
voiding
Biofeedback/Pelvic
Medications
Neural
Botox
stimulation
Floor Rehabilitation
Interstim Nerve Stimulator
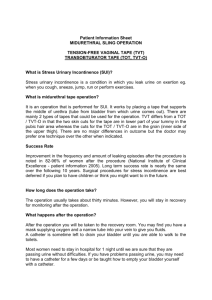
What is Stress Incontinence?
Loss of urine with
anything that increases
the pressure on the
bladder that overcomes
the urethral sphincter
Cough
Sneeze
Exercise
Laugh
What Causes Female SUI
Hypermobile urethra –
descent
Inadequate urethral
sphincter
These are resulting from
Birth, trauma, surgery,
radiation, hormonal
changes, muscle
deterioration
SUI Treatments
Goal:
To strengthen or support the
damaged pelvic floor muscles
Pelvic
floor excercises
Pessaries or Urethral Plugs
Bulking agents
Minimally Invasive Surgery
*There
are no medications at this point
FemSoft Insert Function
Disposable, Single-Use
Device
Placed in a Woman’s Urethra
to Prevent Accidental
Leakage
Soft Sleeve Conforms to the
Urethra and Bladder Neck
Bulking Agents
Slings
90% success rate
Minimally invasive
Outpatient
Quick recovery 3-4
days
What is Mixed Incontinence?
The
combination of both stress and urge
incontinence.
Therapy
focuses on the most bothersome
symptom and usually requires both
nonsurgical and surgical treatment.
Recurrent UTIs
20%
of women who have a UTI will have
another
30% if you have had 2
80% if you have had >2
Defined
as at least 2 culture documented
infections in 6 months or 3 in 12 months
Why do I always get bladder
infections?
Hormone deficiency
Diabetes
Incomplete bladder emptying either from weak
bladder muscle or partial obstruction from
prolapse
Bladder stones or masses
Incomplete initial treatment or bacterial
resistance
Intercourse
How do I get rid of the darn
things?
Always
get a urine culture and antibiotic
sensitivity when symptoms occur
Have a physical exam and cystoscopy to
ensure no anatomical reasons
Treatments:
Low dose daily antibiotic for at least 6 months
Single antibiotic dose with each intercourse
Hormone supplementation
Recurrent UTI prevention
Drink plenty of water to avoid concentrating any
small bacteria in urine
Wipe front to back to avoid anal bacterial
contamination
Take showers instead of baths
Cleanse genital area after intercourse
Avoid douches and feminine hygiene spray
Drink Cranberry Juice
Fecal Incontinence
Inability
to control your bowels
Either leakage with urge or unexpected
6.5
million Americans
Not a normal part of Aging
Anatomy Rectum and Anus
What causes Fecal
Incontinence?
Childbirth/trauma/surg
ery may damage the
sphincter or the nerve
innervation
Loss of storage
capacity in the rectum
Diarrhea or loss of
bulking
Pelvic floor
dysfunction
Non-surgical management
Dietary changes
Fiber supplementation
Drink lots of water
Avoid foods which exacerbate IBS or diarrhea states
• Caffeine, spice, cured meat, grease, artificial
sweetners
Bowel management
Planned defectation (timing, use of gastrocolic reflex)
Enemas
Non-surgical management
Pharmacologic interventions
Steroids and sulfasalazine for UC
Steroid enemas for radiation proctitis
Cholestyramine for diarrhea from malabsorption
of bile salts
Motility agents:
Loperamide (Imodium)
Lomotil (atropine/diphenoxylate)
Non-surgical management
Perineal exercises to strengthen muscles
Anal Plug
Biofeedback
Sensory training
Muscle training
Cure or improvement in 70-80%
Results tend to be long-lasting
Surgical Procedures
Sphincteroplasty
Prolapse Repair
Artificial Anal
Sphincter
Bulking agent
Radio-Frequency
Sacral Nerve
Stimulation
Colostomy
Conclusion
Bladder
and Fecal Incontinence can rob
you of your life. Let us help you get your
LIFE BACK!!