ADMINISTRATION OF OXYGEN
advertisement

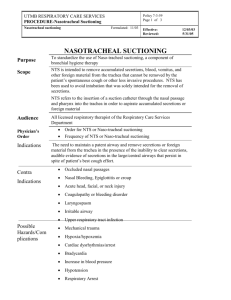
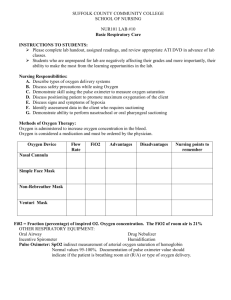
ADMINISTRATION OF OXYGEN SHARON HARVEY LEARNING OUTCOMES THE STUDENT SHOULD BE ABLE TO: REVIEW THE PHYSIOLOGICAL REQUIREMENTS OF THE BODY FOR OXYGEN. IDENTIFY WHEN OXYGEN THERAPY MAY BE NEEDED FOR AN ADULT AND CHILD DEMONSTRATE HOW OXYGEN THERAPY SHOULD BE PRESCRIBED USING A PRESCRIPTION/MEDICATION CHART LEARNING OUTCOMES DISCUSS THE SAFE AND EFFECTIVE DELIVERY OF OXYGEN THERAPY WITH PARTICULAR REFERENCE TO: USE OF COMMON DELIVERY APPARATUS (FACEMASKS, NASAL CANNULA) FOR ADULT AND CHILD SAFETY CONSIDERATIONS (THE CORRECT FLOW RATE, AVOIDANCE OF NAKED FLAME) STORAGE AND DELIVERY OF OXYGEN IN CLINICAL AREAS LEARNING OUTCOMES DISCUSS THE PATIENT’S EXPERIENCE WHEN UNDERGOING OXYGEN THERAPY IDENTIFY EFFECTIVE NURSING INTERVENTIONS TO SUPPORT THE PATIENT, E.G. ORAL HYGIENCE, ADEQUATE FLUID INTAKE, CORRECT POSITIONING TO ACHIEVE MAXIMUM VENTILATION OF LUNGS DISCUSS THE INDICATIONS AND CONTRAINDICATIONS FOR A CHILD AND ADULT: NASOPHARYNGEAL AND OROPHARYNGEAL SUCTIONING LOWER AIRWAY SUCTIONING SUCTIONING OF THE TRACHEOSTOMY OXYGENATION OXYGEN – A PRESCRIBED DRUG MUST BE WRITTEN LEGIBLY BY THE DOCTOR PRESCRIPTION SHOULD BE DATED BY THE DOCTOR DOCTOR MUST INDICATE DURATION OF O2 THERAPY THE O2 % CONCENTRATION MUST BE PRESCRIBED THE FLOW RATE MUST BE PRESCRIBED INDICATION FOR OXYGEN THERAPY ACUTE RESPIRATORY FAILURE ACUTE MYOCARDIAL INFARCTION CARDIAC FAILURE SHOCK HYPERMETABOLIC STATE INDUCED BY TRAUMA, BURNS OR SEPSIS ANAEMIA CYANIDE POISONING DURING CPR DURING ANAESTHESIA FOR SURGERY OXYGEN DELIVERY SYSTEMS BASIC COMPONENTS OF A OXYGEN DELIVERY SYSTEM PIPED OR PORTABLE CYLINDER OXYGEN SUPPLY A REDUCTION GAUGE FLOW METER (LITRES/MIN) BASIC COMPONENTS OF A OXYGEN DELIVERY SYSTEM DISPOSABLE TUBING OF VARYING DIAMETER AND WIDTH MECHANISM FOR DELIVERY (MASK OR CANNULA) HUMIDIFIER (TO WARM AND MOISTEN THE O2 METHODS OF ADMINISTERING OXYGEN SIMPLE SEMI-RIGID MASKS NASAL CANNULA FIXED PERFORMACE MASKS OR HIGH-FLOW MASKS (VENTURI) T-PIECE CIRCUIT PAEDIATRIC CIRCUITS - HEADBOX OR HOOD - O2 TENT/COT TRACHEOSTOMY MASK MECHANICAL VENTILATION CONTINUOUS POSITIVE AIRWAY PRESSURE (CPAP) HUMIDIFICATION OF OXYGEN NORMAL AIR TRAVELLING THROUGH THE AIRWAYS IS WARMED, MOISTENED AND FILTERED BY EPITHELIAL CELLS OF THE NASOPHARYNX THE AIR ENTERING THE TRACHEA WILL HAVE A RELATIVE HUMITY OF 90% AND A TEMPERATURE OF BETWEEN 32-36 C OXYGENATION WILL CAUSE DEHYDRATION OF THE MUCUS MEMBRANES AND PULMONARY SECRETIONS HUMIDITY IS ESSENTIAL FOR PATIENTS WHO HAVE AN ENDOTRACHEAL OR TRACHEOSTOMY TUBE HUMIDIFICATION REQUIREMENTS HUMIDIFICATION AND TEMPERATURE SHOULD NOT BE AFFECTED BY THE FLOW RATE SAFETY ALARMS SHOULD GUARD AGAINST OVERHEATING, OVER HYDRATION AND ELECTRIC SHOCK NO INCREASED RESISTENCE TO RESPIRATION WIDE BORE TUBING (ELEPHANT) SHOULD BE USED TO ALLOW SUFFICIENT FORMATION OF WATER VAPOUR HEALTH AND SAFETY ISSUES WITH O2 MEDICAL GAS CYLINDERS HAVE TO CONFORM TO COLOUR CODING CURRENTLY OXYGEN CYLINDERS ARE BLACK WITH WHITE SHOULDERS. HEALTH AND SAFETY ISSUES WITH OXYGEN OXYGEN IS COMBUSTIBLE OIL AND GREASE AROUND CONNECTIONS SHOULD BE AVOIDED ALCOHOL, ETHER AND INFLAMMATORY LIQUIDS SHOULD BE KEPT SEPARATE FROM O2 NO ELECTRICAL DEVICES NEAR 02 TENT NO SMOKING FIRE EXTINGUISHER NEEDS TO BE AVAILABLE CARE WITH USING DEFIBRILLATOR NEAR HIGH OXYGEN CONCENTRATIONS POTENTIAL PROBLEMS CO2 NARCOSIS CO2 LEVELS IN THE BLOOD NORMALLY INFLUENCES RESPIRATION PATIENTS WHO ARE HYPERCAPNIC CO2 E.G. CHRONIC BRONCHITIS, HAVE THEIR BRAIN CHEMORECEPTORS NO LONGER SENSITIVE TO LEVELS CO2 - INSTEAD THE HYPOXIC DRIVE BECOMES THE RESPIRATORY DRIVE I.E. O2 IS THE DRIVE FOR RESPIRATION - HIGH LEVELS OF SUPPLEMENTARY O2 MAY LEAD TO REPIRATORY DEPRESSION/UNCONSCIOUSNESS AND DEATH POTENTIAL PROBLEMS OXYGEN TOXICITY THIS FOLLOWS AFTER PROLONGED O2 THERAPY (>24 HOURS) THERE IS DECREASING LUNG COMPLIANCE FROM HAEMORRHAGIC INTERSITIAL AND INTRAALVEOLAR OEDEMA THIS ULTIMATELY LEADS TO FIBROSIS OF LUNG TISSUE >24 HOURS AND > 50 % O2 THERAPY SHOULD BE AVOIDED PRINCIPLES OF SUCTIONING SHARON HARVEY PRINCIPLES OF SUCTIONING THREE PRIMARY SUCTIONING TECHNIQUES ARE: OROPHARANGEAL/ NASOPHARANGEAL SUCTIONING OROTRACHEAL AND NASOTRACHEAL SUCTIONING SUCTIONING AN ARTIFICAL AIRWAY SIGNS OF A NEED FOR SUCTIONING RESPIRATORY RATE CHANGE IN RESPIRATORY PATTERN NOISY BREATHING DIFFICULTY SUCTIONING REDUCED OR UNEVEN AIR ENTRY INCREASED AIRWAY PRESSURE SURGICAL EMPHYSEMA OR OTHER NECK SWELLING DISTRESSED PATIENT HYPOXIA THE ABILITY TO HEAR THE PATIENT SPEAK WHEN CUFF IS INFLATED PRINCIPLES OF SUCTIONING OROPHARYNGEAL SUCTIONING REMOVES SECRETIONS FROM THE PHARYNX VIA A CATHETER PLACED THROUGH THE MOUTH OR NOSTRILS THIS TYPE OF SUCTIONING IS USED WHEN THE PATIENT S ABLE TO COUGH EFFECTIVELY BUT UNABLE TO CLEAR SECRETIONS BY EXPECTORATING OR SWALLOWING PROCEDURE IS CARRIED OUT AFTER THE PATIENT HAS COUGHED ASSESSMENT PRIOR TO SUCTIONING ABNORMAL BREATHING SOUNDS IRREGULAR RESPIRATORY PATTERN CHANGES IN SECRETIONS INCREASE IN COUGHING INCIDENTS CHANGE IN PATIENT’S APPEARANCE COMPLICATIONS OF SUCTIONING TRAUMA HYPOXIA INFECTION OROPHARYNGEAL SUCTIONING MEASUREMENTS? ALWAYS USE THE SMALLEST DIAMETER SUCTION CATHETER POSSIBLE TO REMOVE THE SECRETIONS FOR ADULTS USE CATHETERS SIZE 12-16 FRENCH GAUGE FOR CHILDREN USE 8-12 CATHETER GAUGE INSERTION DEPTH FOR NASOPHARYNGEAL SUCTIONING: ADULTS INSERT ABOUT 16CM INFANTS AND YOUNG CHILDREN 4-8 CM OROPHARYNGEAL SUCTIONING CAUTION ON PATIENTS WITH: NASOPHARYNGEAL BLEED OR CSF LEAK ANTI COAGULANT THERAPY OROPHARYNGEAL SUCTIONING PROCEDURE REVIEW OXYGEN SATURATIONS AND BREATHING PATTERN EVALUATE ABILITY TO COUGH CHECK HISTORY FOR DEVIATED SEPTUM, NASAL POLYPS, NASAL OBSTRUCTION, TRAUMATIC INJURY, EPISTAXIS OR MUCOSAL SWELLING EXPLAIN PROCEDURE INFORM THAT SUCTIONING MAY CAUSE TRANSIENT COUGHING AND GAGGING MINIMISE ANXIETY POSITION PATIENT IN AN UPRIGHT POSITION TO PROMOTE LUNG EXPANSION OROPHARYNGEAL SUCTIONING TURN ON SUCTION (80-120 MMHG) EXCESSIVE PRESSRE MAY CAUSE TRAUMA OCCLUDE THE END OF CONNECTING TUBE TO CHECK SUCTION PRESSURE ASEPTIC TECHNIQUE USE LUBRICANT IF THE CATHETER IS PASSED THROUGH NASAL PASSAGE OROPHARYNGEAL SUCTION USE YOUR DOMINANT HAND TO CONTROL THE CATHETER USE YOUR OTHER HAND TO CONTROL SUCTION VALVE PATIENT TO COUGH AND BREATH DEEPLY BEFORE SUCTIONING COUGHING HELPS TO LOOSEN SECRETIONS DEEP BREATHING HELPS TO MINIMISE HYPOXIA AND LUNG COLLAPSE OROPHARYNGEAL SUCTIONING SPECIAL CONSIDERATIONS ALTERNATE BETWEEN NASAL PASSAGES TO MINIMISE TRAUMATIC IJURY WHERE REPEATED SUCTIONING IS REQUIRED, A PHARYNGEAL AIRWAY WILL HELP WITH CATHETER INSERTION, REDUCE TRAUMA AND PROMOTE PATENT AIRWAY RESPT PATIENT AFTER SUCTIONING AND OBSERVE OROPHARYNGEAL SUCTIONING COMPLICATIONS DYSNOEA BLOODY ASPIRATE DOCUMENTATION RECORD THE DATE TIME PROCEDURE TECHNIQUE REASON FOR SUCTIONING