Tracheostomy Care
advertisement

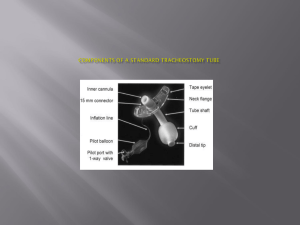
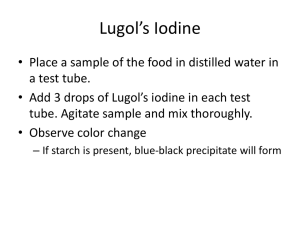
Tracheostomy Care Adapted from various resources (see reference slide) by Ambercare Education Department April 14, 2014 Tracheostomy Facts Tracheotomy is a surgical procedure that creates an opening in the cervical trachea (windpipe) allowing direct access to the breathing tube – rarely done as an emergency – secondary to oral or nasal intubation which is must faster and less complicated when managing respiratory arrest Why is a Tracheostomy performed? To bypass obstruction To maintain an open airway To remove secretions more easily To oxygenate and/or provide mechanical ventilation on a long-term basis Types of patients requiring tracheostomies A comatose patient A patient with cancer of the larynx or neck Blockage of airway Inability to swallow or cough A burn patient with inhalation damage A COPD patient on mechanical ventilation A pediatric patient with a congenital airway obstruction ALS patients Plegic patients To name a few…. Tracheostomy Anatomy Tracheostomy Anatomy Landmarks Definition of Terms Decannulation: Removal of a tracheostomy tube HME: Heat, moisture exchange (have pictorial) Humidification: the mechanical process of increasing the water vapor content of an inspired gas Stoma: a permanent opening between the surface of the body and an underlying organ (trachea and anterior surface of neck) Tracheal suctioning: a means to clear the airway of secretions or mucus through the application of a negative pressure via a suction catheter Temporary Tracheostomy versus Permanent Laryngectomy Appearance may be the same Temporary: THE UPPER AIRWAY WILL REMAIN PATENT IF THE TRACH TUBE WERE TO BE DISLODGED Permanent: THE LARYNX IS REMOVED AND AN ARTIFICAL TRACHEOSTOMY IS CREATED – NO CONNECTION BETWEEN THE PATIENT’S UPPER AIRWAY AND THE TRACHEA ITSELF! Risks / PCs Medication reaction Uncontrollable bleeding Respiratory problems Possibility of cardiac arrest Pneumothorax SC and/or mediastinal emphysema Tracheo-oesophageal fistula (development of a small connection between trachea and esophagus) Infection Potential Complications with Longterm Tracheostomy: Thinning (erosion) of the trachea (trachemalacia) Development of granulation of tissue (bump formation in trachea Narrowing or collapse of the airway above the site of tracheostomy Once tracheostomy tube is removed, the opening may not close on its own Dysphagia; airway obstruction from secretions; Tracheal ischemia and necrosis Assessment / SE after tracheostomy placement Respiratory secretions will often temporarily increase Observe for s/sx of impaired gas exchange (mucus plugs for example) – encourage patient to breathe deep and cough – ensure adequate humidification and NS fluid bullets to loosen secretions if needed (suctioning) A small amount of bleeding from the stoma is expected for a few days after trach placement – constant oozing, is abnormal – may need intervention ( a blood vessels may need surgical litigation) Slight inflammation at site (redness, pain, drainage for the first few days) Continued Assessment/SE after tracheostomy placement Subcutaneous emphysema (SCE) around stoma – air escapes into the tracheostomy incision creating SCE; generally of no clinical consequence – but can be palpated around the stoma site Excessive manipulation of the trach tube during coughing or suctioning can break improperly secured ties and dislodge the tube – (within the first 48 hours the freshly created stoma has a potential to close shut, constituting a medical emergency) – to minimize this risk, trach ties are not usually changed for 24 hours – First tube change is generally done by a physician after approximately one week (should have detailed Dr’s orders to always have a spare trach tube on hand – size should be indicated Endotracheal Tube Verses Tracheostomy Tube Cuffed Tracheostomy Tube Consists of three parts: • Outer cannula with an inflatable cuff and pilot tube • An inner cannula • An obturator Cuffless tubes Rarely used in acute care settings More suitable for long term ventilation Cuffless tube is usually double-lumen – patient must have effective cough and gag reflex to prevent aspiration risk Fenestrated Tube Have an opening on the posterior wall of outer cannula – allows for air flow through the upper airway and trach opening; Allows patient to speak and produce a more productive cough Often used during weaning process Identifying Tracheostomy Parts Identifying Trach Parts Identifying Trach Parts Communication and Tracheostomies Some trach tubes are designed to allow patients to speak Patients being weaned off trach tubes may have either a cuffless, fenestrated tube or a trach button that does not extend into the trachea enough to restrict airflow past the larynx For long-term Trach patients Speaking is possible with these options: A fenestrated inner cannula inside a cuffed outer cannula – allows for speech when cuff is deflated (some tubes expand on inspiration and deflate on expiration versus manually deflated cuffs) A tracheostomy speaking valve is a device that attaches to the trach tube – it contains a diaphragm that opens on inspiration and closes on expiration so that air is exhaled through the vocal cords and upper airway – the cuff must be COMPLETELY deflated during speaking valve to allow for exhalation through the upper airway Tracheostomy Care Kit Trach Care Kit / Portable Suction Machine Trach Care Kit Thermo Trach Tracheostomy Collar connected to ventilator – notice sutures Nursing Care Nursing Care Must conduct a thorough assessment of patient at the start of visit Observe for signs of hypoxia, infection, excessive secretions, pain, etc. Examine trach tube, any attached tubing and equipment, as well as stoma site Observe for redness, purulent drainage, and abnormal bleeding around the stoma – note the amount, color, consistency, and odor of secretions Auscultate breath sounds Ensure that appropriate emergency trach supplies and CPR equipment is at bedside Be aware of when and why the trach was inserted , how it was performed, the type and size of tube inserted Tracheostomy Humidification As mentioned previously, the nose and mouth provide warmth, moisture and filtration for the air we breath. Having a tracheostomy tube, however, by-passes these mechanisms so humidification must be provided to keep secretions thin and to avoid mucus plugs Types of tracheostomy humidification systems Heated humidification (increased heat and water vapor inhaled) – Ambient or cold water humidification Heat and moisture exchangers Stoma protectors Heat moisture exchanger (attached to the outside of a trach tube for long-term trach patients) – looks like a t-tube attachment Humidification examples Heat moisture exchanger Nursing Care: Mobilizing Secretions Many trach patients have acute or chronic disease that predispose to stagnation of secretions Frequent repositioning, deep breathing and coughing, chest physiotherapy, postural drainage, oral and parenteral hydration and supplemental humidification all help to thin and mobilize secretions Tubing from an external moisture source accumulates moisture and will need frequent draining – ensure the tubing is positioned LOWER than the patient to avoid aspiration risk! Nursing Care - Suctioning Necessary for all trach patients to remove secretions and assess for airway patency Acute care patients need to be assessed every two hours (teach family members)… Routinely done 2x / day, but more often if needed – particularly a newly placed tracheostomy or when there is infection present Suctioning activates psychological and physiological reflexes that make the experience both uncomfortable and frightening Indications for Suctioning Dyspnea: Flared nostrils, chest retractions and/or prolonged wheezing Noisy breathing Cyanosis and clammy skin Restlessness and agitation Copious secretions; moist cough Low oxygen saturation Increased peak inspiratory pressure on mechanical ventilator U tube video on suctioning http://www.youtube.com/watch?v=gtKc9pe9HCw (copy and paste URL); 15 minute video on suctioning tracheostomy – excellent example….worth the time to view – particularly those staff members who are not well versed on tracheostomy care Selecting a suction catheter Selection of the appropriate size suction catheter is vital in reducing the risk of trauma during suctioning Divide the internal diameter of the tracheostomy by two, and multiply the answer by three to obtain the French gauge suction catheter: Size 8 tracheostomy tube (patient); (8mm/2) x 3 = 12; therefore, a size 12F gauge catheter is suitable for suctioning Gathering equipment for suctioning – open system PPE – (mask, goggles, gloves) Bottle of normal saline Appropriately sized suction catheter Trach care kit Disposable inner cannula 02 source – connected to patient (suction equipment) regulator set at 80-120 mmHg Ambu bag to ventilate patient prior to suctioning if appropriate I RECOMMEND YOU VIEW THE U TUBE VIDEO TO UNDERSTAND APPROPRIATE SUCTIONING TECHNIQUE AND HOW TO UTILIZE THE EQUIPMENT ABOVE…. Closing suctioning system – ballard suctioning Procedure for suctioning Place patient in semi-fowler’s position Select appropriate sized suction catheter Hyper oxygenate BEFORE each suction pass (exceptions to hyper oxygenation are children and patients with long-term tracheostomies) Insert catheter to a pre-measured depth or (to point of resistance if deep suctioning) Apply suction on withdrawal while slowly removing suction catheter Limit suctioning to 5 seconds for pre-measured depth and 10-15 seconds for deep suctioning Use suction pressure between 80 – 120 mmHg Limit suctioning to 3 passes and discontinue if HR drops by 20; increases by 40, produces arrhythmias, or decreases 02 < 90% Tracheostomy Ties To lower the risk of a new trach tube accidentally dislodging, ties are usually not changed within the first 24 HOURS FOLLOWING INSERTION; thereafter, ties are generally changed daily To lower the risk of accidental decannulation (the trach tube coming out) the tie changes should be performed by two people or with new ties secured BEFORE old ties are removed. Maintenance of the inner cannula The majority of trach tubes have inner cannulas that require cleaning one to three times daily unless they are disposable Use sterile technique to clean the reusable cannula with ½ strength hydrogen peroxide and normal saline or just NS Reinsert and lock back into place within a 15 minute time frame Trach parts… Trach parts – inner cannula example Nursing Care – Trach cuff pressure Cuff pressure (balloon) should be maintained between 20 to 20 mmHg of pressure via a manometer – should be assessed daily; if you don’t have a manometer measuring device – check with the patient/family – to evaluate how many cc’s of cuff pressure they have been utilizing (generally 5-8 cc) depending on trach size With a stethoscope placed on the neck, inflate the cuff until you no longer hear hissing; deflate the cuff in tiny increments until a slight his returns…. Deflating and inflating the cuff is a way to: Assess and evaluate how the cuff is working Periodically relieve pressure on the trachea Let secretions above the cuff drain down so you can suction them Nursing Care: Changing the Trach tube Trach tubes, (both single cannula type and the outer cannula of a universal type) are changed one to four weeks (check physicians order – consult if needed) Silicon tubes can crack and tear; soft PVC tubes can stiffen with age and metal tubes can develop cracks When a patient has had a tracheostomy for several months, the stoma is well formed and tube changes can be done safely on a monthly basis using a clean technique; the initial tube change is usually performed by MD Nursing care: Trach Site care and Dressing changes Assess the stoma for s/sx of infection and skin breakdown Clean stoma with Q-tip moistened with NS; avoid using hydrogen peroxide unless infection present (as it can impair healing) – Dressings around the stoma are changed when excessive exudate is present – keep CDI Please refer to the following U tube video entitled “home trach care” = 5.08 (time) http://www.youtube.com/watch?v=swTLAokDnq8 Nursing Care: Nutrition and Communication A tracheostomy WILL NOT prevent a patient from eating – although some patients may have concurrent swallowing problems that may need evaluation by an otolaryngologist or speech pathologist Patients may have poor appetite because of disease progression or reaction to copious secretions; suctioning PRIOR to meals is helpful Inability to speak is anxiety-provoking for most patients – you will need to evaluate alternative methods of communication for your patient until long-term speaking solutions are initiated Possible Trach Complications Can arise the first few days or within several weeks; initially, the most common complications are: Inflammation and edema of the trachea Infection and abscess of stoma and/or pulmonary tree Bleeding associated with suctioning If humidity is insufficient, mucous membranes dry out and the irritation of an inserted catheter will cause small amounts of bleeding during routine suctioning Long-term complications from the presence of a trach are due to tracheal scarring and erosion Stenosis, the narrowing of the trachea from scar tissue occurs in 5 to 15% of patients Scarring can occur at the stoma, the cuff site, or at the point where the distal end of the tube presses on the tracheal wall – possible granuloma…. Home Trach Care Patient and family education normally starts in hospital setting Initial care may consist of: Warm compress to the incision site to help relieve discomfort Humidified air Wearing a scarf over trach opening to keep dry and clean Follow up with Dr. for any concerns or changes Patient Instructions Trach patient’s avoid: Deep bathing water Fine particles such as powders, chalk, sand, dust, mold and smoke Loose fibers and fair found on fuzzy toys and pets Persons with contagious illnesses Cold air and wind Portable suction equipment is available for travel and should be tested PRIOR to use GREAT RESOURCE TEACHING SITE: http://www.tracheostomy.com FAQs Can a patient eat with a Tracheostomy: Yes…generally speaking (patient may need an evaluation by a speech pathologist to determine swallowing ability) The primary exception is if the patient wears a tracheostomy speaking valve (Passy Muir Valve) and needs one type of inner cannula when the speaking valve is in place Swallowing is safer with the cuff down and speaking valve on FAQs Why can’t we use the Passey Muir valve with the cuff inflated? The speaking valve is a one-way airflow mechanism. The patient inhales air through the speaking valve but exhales it around the tracheostomy tube and then through the nose or mouth. If the cuff is inflated with a speaking valve, the patient will only be able to inhale air and will not be able to exhale since there will not be any room around the tracheostomy FAQs How often should a tracheostomy tube be changed? Every seven days to remove the dried or old secretions and maintain adequate hygiene of the trach tube and airway FAQs What is the tracheostomy plug? Used for two purposes: Decannulation of the tracheostomy tube Used to plug trach tube for 12 hours the first day and 24 hours the second day – if the patient tolerates plugging, then decannulation can take place It can be used for speech, but not as a speaking valve A speaking valve is a one-way valve unlike a trach plug which completely obstructs the air flow FAQs Why do you need the inner cannula with a tracheostomy: Easier to remove inner cannula for cleaning and to maintain hygiene of the airway If patient develops a mucus plug, the inner cannula can be removed for cleaning or a replaced with a disposable one - the outer cannula would serve as the airway Changing the entire outer cannula is more difficult than managing the airway with an inner cannula Questions? References AMN healthcare education services (rn.com) http://www.rch.org http://www.hopkinsmedicine.org http://my.clevelandclinic.org Various U tube videos as noted