Enterobius vermicularis
Taxonomical position
•
•
•
•
•
•
•
Phylum
:
Class
:
Order
:
Super family :
Family
:
Genus
:
Species
:
Nematoda
Secernentea
Oxyurida
Oxyuroidea
Oxyuridae
Enterobius
vermicularis
Common names:
• Pin worm
• Thread worm
• Seat worm
History:
• ‘Leukart’ – first described the complete life cycle
in 1865
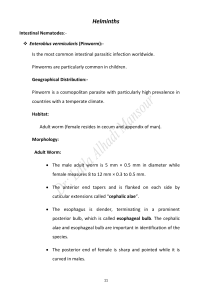
Distribution:
• Cosmopolitan
• More common in temperate and cold climate than warm
climate
Habitat:
LARGE INTESTINE
- Caecum
- Appendix
- Ascending colon
Morphology:
ADULT:
• Short, white, fusiform
• Pointed ends
• Resemble white threads
Cervical Alae:
- At the anterior end
- Three in number
- Wing like cuticular expansions
- Transversely striated
Oesophagus- DOUBLE BULB
MALE WORM:
• Posterior end is curved
• Copulatory spicule
• Length
: 2-5 mm
• Thickness : 0.1- 0.2 mm
• Life span : 7 weeks
FEMALE WORM:
• Thin, pointed, pin like tail
• Reproductive organs
- T shaped
- paired
OVIPAROUS
• Length : 8 - 13 mm
• Thickness: 0.3 - 0.5 mm
• Life span : 5 - 13 weeks
EGG:
• Colourless, non-bile stained
• Shape: Planoconvex
• Shell : Double layered
Transparent
• Sticky outer albuminous layer
o Contains ‘tadpole shaped’,
coiled larva
• Viable up to 2 weeks
LIFE CYCLE
Life cycle:
• Simplest of all the intestinal worms
• Host :
MONOXENOUS- single host – Human
• Infective form: embryonated egg
• Route: Faeco-oral transmission
• Eggs transform in to larvae in 5 weeks in small intestine
• Larva undergo moulting in ileum and finally mature in to
adult in caecum with in 15 to 30 days
• Male dies after fertilization
Conti…
Egg
5 weeks
(small intestine)
Larva
moulting(ileum)
15-30 days
maturation(caecum)
Adult
male
dies after fertilization
female
Conti…
migrate to rectum
come out through anus during night time
Eggs laid on perineal, peri anal skin
Conti…
1 worm
=
5000 – 17000 eggs
Become infective in 6 hrs
Completes life cycle in 2 weeks – 2 months
Pathogenesis:
• Adult worm:
• Egg:
- mucoid secretions – adherence of egg
- irritation
- Characteristic NOCTURNAL PERINEAL / PERIANAL
ITCHING
Clinical manifestations:
• ENTEROBIASIS – Pruritis ani
• Scratching, excoriation of skin
• Disturbed sleep, irritability, nocturnal enuresis, weight
loss, abdominal pain
Severe infection:
• Neurosis
• Nail biting
• Grinding teeth at night
Complications:
•
•
•
•
•
•
Vulvo- vaginitis
Chronic salpingitis
Prostatitis
Urethritis
Endometritis
Granulomata with dead worms, eggs
Epidemiology:
• Group infection: School children
• Prevalent in temperate countries
• USA, European countries
• Source: Infected humans
others like bedding, night clothing, table tops,
door knobs,taps etc.,
• Transmission: Auto infection
contaminated articles / direct contact
inhalation of eggs
Retroinfection
Diagnosis:
• H/O perianal pruritis
LAB DIAGNOSIS:
• Demonstration of Adult worm:
- On the surface of stool sample
- On the perianal skin
- In the stool after an enema
• Demonstration of Eggs:
- As they are seldom excreted in faeces, stool sample
is not useful for diagnosis
1. NIH swab:
2.Scotch tape swab:
• Atleast 3 specimen collected
in 3 consecutive days
3.Dirt from finger nails.
Treatment:
• Single dose:
Pyrantel
- 11mg/kgwt
Mebendazole - 100mg/kgwt
Albendazole - 400mg/kg wt
• Piperazine - 65mg / kg wt – 1 week
• Pyrantel causes spastic
paralysis of the worm
Prophylaxis:
• Health education on personal hygiene
• Group chemotherapy
THANK YOU