stridor2 - WordPress.com
advertisement

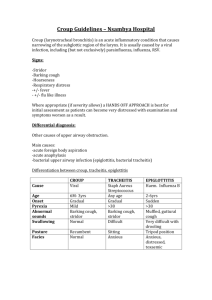
Acute Stridor By Yehia Abo Arida Ward 7 Stridor It is a harsh, high-pitched respiratory sound, which is usually inspiratory but it can be biphasic and is produced by turbulent airflow; it is not a diagnosis but a sign of upper airway obstruction . Causes of acute stridor Laryngotracheobronchitis ( croup) . Epiglottitis . Bacterial tracheitis . Foreig body Angioedema . Hypocalcemic tetany . Edema after endotracheal intubation . Assessment of severity of stridor Timing : – The prominent phase of respiratory noise should be inspiratory – Expiratory stridor ----- more severe , or intrathoracic obstruction . Work of breathing : – Increased RR . – Sternal ( supra – sub ) recession . How effective is the breathing : – Chest expansion . – Breath sounds for air entery . Is there adequate oxygenation : – – – – Is HR increased . Pallor , cyanosis . O2 saturation . Activity level . Worrying signs in children with stridor High fever or signs of toxicity Rapid onset . Drooling & dysphagia . Muffled voice & quiet stridor . Angioedema . Age less than 4 mths . Skin cavernous hemangioma . Previous ventilation as a neonate . Croup Is derived from an old scottish word , roup , which means to cry out in a hoarse voice . Viral croup ( ALTB ) Viral croup is the most common cause of acute stridor in children . Most patients with croup are between ages of 3 mths and 5 yrs , with the peak around 1-2 yrs . Common pathogens include parainfluenza viruses ( 1,2 & 3 ) account for 75% of cases; others include influenza ( A&B ) , RSV & measles V . Mycoplasma pneumoniae has rarely been isolated from children with croup . The term laryngotracheobronchitis refers to viral infection of the glottic and subglottic regions . Some clinicians use the term laryngotracheitis for the most common & most typical form of croup and reserve the term LTB for more severe form . Inflammation & partial obstruction of the upper airways result in a barkelike or brassy cough& inspiratory stridor & may be associated with hoarseness & RD . Small children are at higher risk because of the relative small size of their upper airways. . . Unlike relatively rare conditions as epiglottitis & bacterial tracheitis , croup has : – a more insidious onset over a few days . – systemic toxicity & fever are considerably less . – have typical barking cough , often associated with hoarse voice , stridor & low grade fever . As in many respiratory conditions , symptoms are often worse at night . Assessment & evaluation Mild: – well , active child . – barking cough . – stridor with agitation – minimal sings of increased WOB . MODERATE : – stridor at rest . – some signs of increased WOB . SEVERE : – stridor at rest + expiratory component . – marked increased WOB . – increased RR & HR – agitation & pallor . – as AW obstruction became very serious stridor became quieter . – agitation turn to exhaustion . Acute spasmodic croup Some children develop recurrent short lived episodes of croup without preceding coryzal prodrome that is seen in classical viral croup. children are afebrile & awake suddenly with acute stridor during night . recurrence occurs on subsequent 2-3 nights . it occurs in children of the same age group , during same season & sometimes same virus can isolated . children with recurrent spasmodic croup often have a strong atopic or asthmatic family background . Radiographs Croup is a clinical diagnosis and does not require a radiograph of the neck . It may show the typical subglottic narrowing or ( steeple sign ) on AP view , which may be present as a normal variation or in epiglottitis & may be absent in patient with croup . Should be considered in patient with atypical presentation . May be helpful to distinguish severe LTB & epiglottitis , but airway management should always take priority . Steeple sign (croup \ normal \ epiglottitis ) due to subglottic narrowing . Treatment Majority of cases will have a mild illness that can be managed at home . Those with significant RD and stridor at rest will require treatment & reassessment . Those showed significant improvement following treatment may be considered for discharge home . There should be a low threshold for admission in : – children under age of 12 mths . – all children with marked RD . – those with oxygen requirement on presentation. – those with parents remain anxious about discharge . Parents of children not requiring admission should receive clear instructions when to return : – chest wall recession . – tachypnoea . – color changes . – inability to feed . – decreased level of consciousness . Therapies may be effective Simple measures : – in all cases it is very important to keep the child and parents calm . – direct inspection of the throat can be dangerous and result in complete obstruction of the airway. – neck x ray is no longer useful and carry the risk of further upset and deterioration . Humidification : – steam inhalation for croup is widely used but of little proven benefits . – the percieved benefits ( placebo effect ) may be due to presence in a warm calming environment . – a steamy bathroom with hot water tap running and plug opened is accepted , but use of kettle and boilers should discouraged , because it carry the risk of scalding . Adrenaline ( epinephrine ) : – nebulized adrenaline is very effective in severe croup . – duration of action between 20 minutes and 3 hours . – it is used in most cases when intubation is considered. – weaning effect of adrenaline result in return to pretreatment baseline rather than a true rebound . – for children with severe croup , the period of improvement on adrenaline is long enough to allow the steroid to start working . Steroids : – Corticosteroids improve clinical parametrs . – Decrease the admission rate . – decrease duration of hospital stay . – Decrease the need for repeated nebulized adrenaline in children with croup . – nebulized budesonide or oral dexamethazone showed equal effect in treating children with croup . – approximately 1-5 % of croup cases require ETT before introduction of steroid therapy . Intubation : – a small numbers of children will still require ET for severe croup . – The decision to intubate should be based on worsening airway obstruction , signs of exhaustion or impending respiratory failure . – Children with epiglottitis and bacterial tracheitis require specialist care , with input from senior ENT & anethetic stuff . – IV antibiotics & intubation are often required . – steroid & adrenaline have minimal effect on these condition . Mild croup Reassurance . May worse by night ( advice to return ) . Dexamethazone PO (0.3- 0.6 mg\kg \ dose). Moderate croup Cardio respiratory monitor Dexamethazone PO&\or nebulized budesonide (pulmicort) 2 mg stat . Reassess in 2 hours – If improved ------- discharge . – If no improvement : Consider nebulized adrenaline 1: 1000 – 2.5 ml for those younger than 1 year . – 2.5 - 5 ml for older than 1 year . – If improved -----observe for 4 hrs & discharge . Severe croup Cardio respiratory monitor . Oxygen to maintain O2 sat ( 92% or more ) . Nebulized adrenaline ( 1\1000) Q 1-4 hrs . IV dexamethazone ( 0.3-0.6 mg\kg\dose ) . Or Nebulized budesonide ( pulmicort ) 2mg . IF no improvement consider BGA , ICU . Intubation & ventillation may be required . Bacterial traheitis Bacterial infection of upper airway , does not involve the epiglottis but, like epiglottitis and croup , is capable of causing life-threatening airway obstruction . Staph aureus is the most commonly isolated organism . Most patients were below 3 yrs , but in recent case series the mean age has been between 5-7 yrs . I t may be considered as bacterial complication of disease , rather than a primary bacterial illness . Clinical manifestations Typically child has a brassy cough , apparently as a part of LTB . High fever and toxicity with RD immediately or after few days of apparent improvement . Patient can lie flat , does not drool , and does not have dysphagia associated with epiglottitis . the usual treatment for croup is ineffective , intubation or tracheostomy may be necessary . The major pathologic feature is mucosal swelling at level of ciricoid cartilage , complicated by copious thick purulent secretions sometimes causing pseudomembrane . Diagnosis Diagnosis is based on evidence of bacterial upper airway disease (high fever – purulent airway secretions & absent classic finding of epiglottitis ) . XR not needed , but may show classic findings (pseudomembrane detachment in the trachea ) . Purulent material is noted below the cords during ET intubation . Black arrow points tracheal pseudomemerane (bacterial tracheitis \ diphtheria ) Treatment Antimicrobial therapy , which usually includes antistaph agents , should be instituted in any patient whose course suggest bacterial traheitis . When diagnosed by direct laryngoscopy , or suspected on clinical background , an artificial airway should be strongly considered . Supplemental oxygen may be necessary . Complications CXR showed : – Patchy infiltrates & show focal densities. – Subglottic narrowing . Cardio respiratory arrest can occur if airway management is not optimal . Toxic shock syndrome has been associated with staph tracheitis . Prognosis oxygen therapy continued . For most of patients is excellent . Patient become afebrile within 2-3 days of institution of antimicrobial therapy , but prolonged hospitalization may be necessary. After extubation the patient should be observed carefully while antibiotics and O2 continued . Epiglottitis Dramatic potentially lethal condition characterized by an acute , potentially fulminating course of high fever , sore throat , dyspnea & rapidly progressing respiratory obstruction . Degree of RD at presentation is variable. Often the otherwise healthy child develops sore throat and fever within a matter of 4-6 hrs .Child appear toxic ,swallowing is difficult and saliva drooling . He sitting upright and assume tripod position( leaning forward ,chin up, bracing on the arm ) . A brief period of air hunger with restlessness may be followed by cyanosis and coma . Stridor is a late and suggest near complete airway obstruction. If no treatment provided complete obstruction of airway and death . barking cough typical of croup is rare . Diagnosis laryngoscopy : – Showed large( cherry red) , swollen epiglottis – Other supraglottic structures especially aryepiglottic fold , occasionally more involved . – It should be performed in a controlled environment as OR or ICU . Lateral radiograph of upper airway : – Showed the classical ( thumb sign ) . Red arrow points ( normal & swollen epiglottis) known as thumb sign or thumb print . Intial management of suspected epiglottitis Do not : – Examine the throat . – Put the child flat . – Order a lateral XR of the neck . – Upset the child by trying to gain iv access or place an O2 mask . Do : – Call airway team . – Stay with the child and parents . – Allow the child to sit on knee of his mother . – Measure O2 sat if possible . – Give O2 therapy if absolutely needed and well tolerated . Treatment Immediate treatment with artificial airway placed in OT or ICU . All cases should receive oxygen unless the mask causes excessive agitation . Racemic epinephrine & corticosteroids are ineffective . Blood & epiglottic surface C&S and in selected cases CSF should be collected after stabilization of airway. Cefotriaxone, cefotaxime , or combination of ampicillin and salbactum should be given parenterally, pending C&S reports . Antibiotics should be continued for 7-10 days . Chemoprophylaxis Not routine for household , child-care or nursery contacts of patient with invasive HIb infection , but observation & medical evaluation is mandatory when exposed child develop febrile illness . Indication for rifampin prophylaxis : – Any contact less than 1y & incompletely immunized . – Any contacts less than 2 yrs of age who has not received the primary vaccination series . – An immunocompromised child in the household . – Dose : (20 mg \kg \d ) once , for 4 days , maximum dose is 600 mg \ day . Prognosis Length of hospitalization and mortality rate increase as infection spread to involve a greater portion of respiratory tract , except in epiglottitis in which local infection may prove to be fatal . Causes of death in croup are : – Laryngeal obstruction . – Complications of tracheostomy . – rarely , fatal out-of-hospital arrest due to viral LTB have been reported . Untreated epiglottitis has mortality rate of 6% but if treatment initiated the prognosis is excellent . The outcome of LTB ,and spasmodic croup is also excellent .