Upper Airway Obstruction/Infections
advertisement

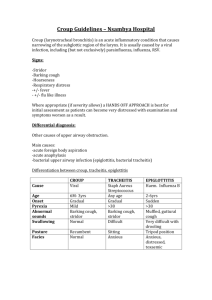
Good Morning! Semantic Qualifiers Symptoms Acute /subacute Chronic Localized Diffuse Single Multiple Static Progressive Constant Intermittent Single Episode Recurrent Abrupt Gradual Severe Mild Painful Nonpainful Bilious Nonbilious Sharp/Stabbing Dull/Vague Problem Characteristics Ill-appearing/ Toxic Well-appearing/ Non-toxic Localized problem Systemic problem Acquired Congenital New problem Recurrence of old problem • Harsh, high-pitched resp sound • Usually inspiratory Stridor – But can be biphasic Site of Pathology Respiratory Rate • Cause by turbulent flow • Sign of upper airway obstruction • NOT a diagnosis Retractions Audible Sounds Extrathoracic airway Stridor Intrathoracic extrapulmonary Wheezing Intrathoracic intrapulmonary Wheezing Alveolar interstitial Grunting Stridor • Viral croup • Foreign body • Noninfectious croup • Retropharyngeal abscess • Epiglottitis • Peritonsillar abscess • Bacterial tracheitis • Angioedema • Extraluminal compression • Caustic ingestion • Intraluminal obstruction from masses • Vocal cord dysfunction “Croup” • Group of conditions – Acute and infectious causes of upper airway inflammation • Upper airway of children Laryngotracheitis • = most common “Croup” illness – Laryngotracheitis vs. Laryngotracheobronchitis/pneumonitis • Predisposing Factors – – – – Between age 3 months and 5 yrs Peak in 2nd year of life M>F Can occur anytime of year but peaks in late fall and winter – Preceding URI illness Laryngotracheitis • Pathophysiology – Inflammation involving the vocal cords and structures inferior to the cords Laryngotracheitis • Pathophysiology – Viral etiology is most common • Parainfluenza viruses (type 1, 2, and 3) ~ 75% of cases • Influenza A – Associated with SEVERE disease • • • • Influenza B Adenovirus RSV Measles – Mycoplama pneumoniae rarely isolated Laryngotracheitis • Clinical Presentation** – URI symptoms for 1-3 days prior to signs of upper airway obstruction • Rhinorrhea, pharyngitis, mild cough, low-grade fever – Characteristic “barking” cough, “seal-like” – Hoarseness – Inspiratory stridor – +/- fever Laryngotracheitis • Clinical Presentation** – Symptoms characteristically worse at night – Agitation and crying aggravate symptoms – Varying degrees of respiratory distress on exam – Should not be hypoxic – this is a sign that complete airway obstruction is imminent Laryngotracheitis • Diagnosis – Clinical – Xrays • “Steeple sign” in AP view • Do not correlate with disease severity • Can help distinguish from other causes Laryngotracheitis • Treatment** – Most patients managed as outpatients – Cool mist?? • Not proven in literature, but used since the 1900’s • If bronchospasm present, can worsen with cool mist – Antibiotics not indicated in viral croup Laryngotracheitis • Treatment** – Corticosteroids • Action: decrease laryngeal mucosal edema • Effective in reducing hospitalization rates, shorter hospital stays, reduced need for subsequent interventions • Dose: 0.6mg/kg single dose DEXAMETHASONE (max 16mg) – PO/IM Decadron both effective – Clincal improvement 6 hours after dose – Prednisolone less effective than Dexamethasone Laryngotracheitis • Treatment** – Nebulized racemic epinephrine (Vaponeb) • For moderate to severe croup • Action: decrease laryngeal mucosal edema • Dose: 0.25ml-0.5ml of 2.25% racemic epi in 3ml of NS nebulized – – – – Onset of relief 10-30min Duration of activity <2-3 hours Can repeat q20 min Monitor for symptoms once the Vaponeb activity duration is over (rebound?), generally 3-4 hrs after a treatment • Use caustiously in patients with tachycardia, and heart conditions such as TOF or ventricular outlet obstruction Laryngotracheitis • Indications for hospitalization with croup – Progressive stridor – Severe stridor at rest – Respiratory distress – Hypoxia/cyanosis – Depressed mental status – Poor oral intake – Need for reliable observation Laryngotracheobronchitis/pneumonitis • More severe form of croup • Considered an extension of laryngotracheitis associated with bacterial superinfection – Occurs 5-7 days into the clinical course – New onset fever – Worsening clinical symptoms, toxic – Increased work of breathing • Signs of both upper and lower airway obstruction • Requires empiric antibiotics Feature Acute Spasmodic Laryngotracheitis Croup Prodrome URI Mean Age 3 mo - 5 yr Onset gradual Fever variable Hoarseness, barking cough Inspiratory stridor Yes Yes: minimal to severe Dysphagia No Toxic appearance No Etiology Viral X-ray findings Steeple sign Treatment cool mist, racemic epi neb, dexamethasone Epiglottitis Bacterial Tracheitis Noninfectious Croup • “Spasmodic” croup** – Most often children 1 to 3 yrs – Pathogenesis unknown – possible allergic etiology – Clinically similar to croup but without the viral prodrome or fever – Most common in the evening – Sudden onset, preceded by mild cough or hoarseness – Episode of characteristic coughing, stridor and respiratory distress, anxious – Severity improves over hours and can have repeat episodes x1-2 more nights Feature Acute Spasmodic Laryngotracheitis Croup Prodrome URI none or minimal coryza Mean Age 3 mo - 5 yr 1 to 3 yr Onset gradual sudden Fever variable no Inspiratory stridor Yes Yes: minimal to severe Yes Yes: usually moderate Dysphagia No No Toxic appearance No No Etiology Viral Noninfectious X-ray findings Steeple sign --- Treatment cool mist, racemic epi neb, dexamethasone cool mist Hoarseness, barking cough Epiglottitis Bacterial Tracheitis Epiglottitis • Predisposing Factors – Typical age of patients 2 to 4 yrs – Unimmunized Epiglottitis • Pathophysiology – Prevaccine, most common cause: • Haemophilus influenzae type B – Now, larger number of cases in vaccinated patients due to: • Streptococcus pyogenes • Streptococcus pneumoniae • Staphylococcus aureus Epiglottitis • Pathophysiology – Inflammation of epiglottis – Degree of inflammation leads to degree of obstruction of airway Epiglottitis • Clinical Presentation – Acute – High fever – Sore throat – Dyspnea – Rapidly progressing respiratory obstruction • Can be within hours – become toxic, difficulty swallowing, labored breathing Epiglottitis • Clinical Presentation – Drooling – Holding neck in hyperextended position – Tripod position – Stridor is a late finding! – Not usually associated with a cough Epiglottitis • Diagnosis – Visualization via laryngoscopy • In controlled environment Epiglottitis • Diagnosis – Xrays • “Thumb sign” in lateral view Epiglottitis • Treatment** – Careful on exam** • Avoid anxiety-provoking procedures (labs/IV), avoid placing patient supine or direct inspection of oral cavity • To prevent acute airway obstruction – Medical emergency – Placement of artificial airway in controlled setting • Mortality ~6% without airway vs. <1% with airway – Oxygen via mask until artificial airway • As long as mask doesn’t cause agitation Epiglottitis • Treatment** – Antibiotics** • • • • Ceftriaxone Cefotaxime Meropenem Obtain cultures from blood, epiglottic surface, and if needed from CSF (after obtain airway) • Treat with at least 7-10 antibiotics, but usually patient improves after 2-3 days Epiglottitis • Rifampin prophylaxis indicated for: – Any household contacts <48 months old and incompletely immunized – Any household contacts <12 months old and has not received primary vaccination series – Any immunocompromised child in the household Feature Acute Spasmodic Laryngotracheitis Croup Epiglottitis Prodrome URI none or minimal coryza Mean Age 3 mo - 5 yr 1 to 3 yr 2 to 4 yr (range 1 to 8 yr) Onset gradual sudden rapid Fever variable no High Inspiratory stridor Yes Yes: minimal to severe Yes Yes: usually moderate No Yes: moderate to severe Dysphagia No No Yes Toxic appearance No No Yes Hoarseness, barking cough none or mild URI Etiology Viral Noninfectious Bacterial: Hib, Strep, S. aureus X-ray findings Steeple sign --- Thumb sign Treatment cool mist, racemic epi neb, dexamethasone cool mist Intubation, Ceftriaxone, or Cefotaxime, or Meropenem Bacterial Tracheitis Bacterial Tracheitis • Predisposing Factors – Mean age 5 to 7 yrs – M=F – Preceding viral respiratory infection • Bacterial complication of croup – More common than epiglottitis in vaccinated patients Bacterial Tracheitis • Pathophysiology – Mucosal swelling at the level of the of the cricoid cartilage – Complicated by copius, thick, purulent secretions, sometimes pseudomembranes – Most common pathogen: S. aureus • Other organisms: Moraxella catarrhalis, nontype H. influenzae, and anaerobic organisms Bacterial Tracheitis • Clinical Presentation** – Preceding croup illness with cough – Then develops high fever and toxic-appearance – Differs from epiglottitis • Patient can lie down, does not drool, no dysphagia – Differs from croup • More toxic, does not respond to racemic epi Bacterial Tracheitis • Diagnosis – Clinical picture • Toxic + absence of classic epiglottitis – Xrays • Not necessary • Findings of irregular lining of the trachea due to pseudomembranes • Can have “steeple sign” Bacterial Tracheitis • Treatment** – Artificial airway required in ~50-60% of patients – More likely to require intubation if younger – Antibiotics • Including appropriate Staph coverage • Vanc + 3rd gen Cephalosporin = empiric coverage Feature Acute Spasmodic Laryngotracheitis Croup Epiglottitis Bacterial Tracheitis none or mild URI URI/croup Prodrome URI none or minimal coryza Mean Age 3 mo - 5 yr 1 to 3 yr 2 to 4 yr (range 1 to 8 yr) 5 yr to 7 yr Onset gradual sudden rapid acute after prodrome Fever variable no High High Hoarseness, barking cough Inspiratory stridor Yes Yes: minimal to severe Yes Yes: usually moderate No Yes: moderate to severe Variable, with prodrome Yes: Variable Dysphagia No No Yes No Toxic appearance No No Yes Yes Bacterial: S. aureus Etiology Viral Noninfectious Bacterial: Hib, Strep, S. aureus X-ray findings Steeple sign --- Thumb sign Irregular tracheal lining Intubation, Ceftriaxone, or Cefotaxime, or Meropenem Often intubation required, Vancomycin and 3rd gen Cephalosporin Treatment cool mist, racemic epi neb, dexamethasone cool mist Noon Conference!