Croup
advertisement

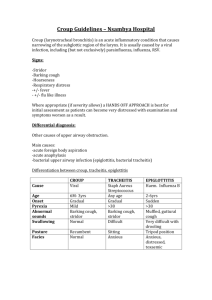
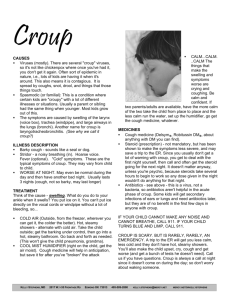
CROUP Dr.S. Alyasin Associated professor Pediatric Department Shiraz University of Medical Science Croup • Airway resistance is inversely proportional to 4th power of radius : minor reduction: increase in air flow resistance. • Larynx: 4 major cartilage: epiglottic – arytenoid – thyroid – cricoid & the soft tissue souround it • Cricoid is just below vocal cord & narrowest in children < 10 yr -0 Supraglottic • Epiglotitis – peritonsilar abcess- retropharyngeal abcess Drooling - hot potato voice – positional preference Infraglottic Laryngitis – lanyngotracheitis, laryngotracheobronchitis • Croup: Heterogenous group of acute and infectious process Bark like cough , may hoarsness, stridor ,distress - (affect larynx,trachea ,bronchus) - Stridor:Harsh ,high pitched usually inspiratory or biphasic ,turbulant flow Croup • Croup typically affects larynx, tarcheabronchi (acute infection • - bark cough • - hoarsness • - stridor) Croup :Etiolology Viral :Para -influenza 1,2,3 75% Influenza A-B, Adenovirus, RSV, measlse, Inf A: Severe LTB Bacterial: diphtheria- bacterial thracheitisepiglotitis – mycoplasma (mild) Croup ;Epidemiology • Age: 3 mo – 5yr, peak: 2nd yr of life • Boy • Late fall & winter (but can throughout the year) • Recurrents : 3-6 yr of age, decrease with growth • Family hx of croup in 15% Croup (Laryngotracheobronchitis) • Some clinicians use the term laryngotracheitis for the most common & most typical form of croup and laryngotrachobronchitis for more sever form with bacterial super-infection (in 5-7 days course) • URI in family • URI rhinorrhea- pharyngitis- cough- low grade fever 1-3 days then barking cough • Low grade to 39- 40 0c or afebrile Croup : Clinical manifestation • • • • • Worse at night Improve in a week Agitation aggravate symptom Prefer sit up Older children are not ill. Croup : Clinical manifestation • PE - hoarse voice - Coryza - mild to mod infla. Pharynx - RR↑ - variable respiratory distress (RR- nasal flaring – retraction) - Stridor Croup :Dx • Alveolar gas exchange is nl so hypoxia only in complete airway obstruction (occasionally difficult to differentiate from epiglottitis) • X-ray may be helpful in distinguishing between sever LTB & epiglottitis but after airway stabilization. Diagnosis Croup is a clinical diagnosis and not require X ray. X Ray AP: steeple sign (false +ve & -ve & not correlate with severity) distinghish between epiglotitis & LTB after stabilization of airway “steeple sign” of subglottic narrowing. (b) Laternal neck radiograph showing subglottic narrowing consistent with acute laryngotracheitis Spasmodic croup • • • • • 1-3 yr No URI hx in family member & patient No fever Cause?: viral- allergic – psychologic An allergic reaction to viral antigen. Acute infectious laryngitis • Virus – Diphteria • URI -sore throat – cough- hoarseness- loss of voice: mild • In infant : RD • Subglottic inflammation Croup: Treatment • Admission: -progressive stridor - severe stridor at rest - - RD - - hypoxia - - cyanosis - - depressed mental status - – poor oral intake - – need for observation. Croup: Treatment • L epinephrinin (5 ml: 1/1000) is as potent as racemic epinephrin (tachycardia – HTN) , every 20 minutes. • Indication: -stridor at rest - need for intubation - - RD - - hypoxia (caution: tachycardia- TOF- venticular outlet obstruction) Croup: treatment: corticosteroid • • • anti inflammatory action: laryngeal edema Oral CS even in mild croup: ↓ admission ↓ duration of admission - ↓need for E – Oral dexametason 0.6 to 0.15 mg/kg single dose = im dexametson or budesonide • Single dose of prednisolon is less potent • 1 week CS: candidal infection *No during varicella infection Croup: treatment • No Antibiotic – • No cough medication in children <4y-0 • Heliox Croup • Discharge: after 2-3 hr observation: - no stridor at rest - normal air entry - nl pulse oximetry – nl level of consciousness - received steroid Treatment: acute laryngeal swelling on an allergic basis • Epinephrine 1/1000 – 0.01 ml/kg im or Racemic E Q .5 ml / with 3 ml nl/s • CS 2-4 mg/kg/24 : prednison Post-extubation croup - Racemic E - - dexametason 0.5 mg/kg/dose every 6 hrs Croup: complication • 15% Om • bronchial , lung parenchyma • Bacterial tracheitis (with toxic shock syndrome) Prognosis • Is related to Length of admission and extension o f infection( except in epiglotitis) • Death in croup: - laryngeal obstruction – complication of tracheotomy • Px is excellent • Admitted patient: increased bronchial reactivity Croup : Df Dx • • • • • • • • • • • • • Foreign body 6mo-3 yrs, sudden , No prodrom Retropharngeal abscess (CT) Peritonsilar abscess Extrinsic compression (web- vascular ring) Intraluminal (papiloma- hemangioma) Angioedema Post extubation Hypocalcaemia tetani I.Mono Trauma Tumor Malformation Very hot liquid : epiglottis like drooling – dysphagia – stridor • Foreign Body • Lateral neck radiograph demonstrating widening of the retropharyngeal space and reversal of the normal cervical spine curvature. The epiglottis and subglottic area are normal. Epiglotitis: Etiology • Hl type B ↓80-90% in vaccinated area for epiglottis: st. pyogen- st. pneumonia- st. aureus • Age 2-4 (although range of 1 to 7 y-0) Epiglotitis • • • • • • • • • Potentially lethal High fever- sore throat- dyspnearesp obstruction within few hours: toxic difficult swallowing Drooling- neck extention Tripod position Air hunger, restless: cyanosis & coma Stridor after complete airway obstruction No barking cough – No illness in family Epiglotitis Dx lanygoscopy: cherry red epiglottis when dx is certain or probable, lanyngoscopy should be done in OR or in ICU Phlebotomy, IV line, supine or direct inspection of oral cavity after airway is secure If dx is not certain : lat X ray neck “ thumb sign” direct visualization. Epiglotittis • Anxiety provoked intervention (phlebotomy- supine –IV-direct inspection of oral cavity) should be avoided. - Most patients have bacteremia: occasionally pneumonia- cervical LAP- OM, rarely: meningitis – arthritis • - Occasionally aryepiglottic fold is more involved than epiglottis Treatment: Epiglotitis • Epiglotitis is medical emergency: Artificial airway in OR or ICU : improved immediately • culture (B- epi_ sometimes CSF) after airway stabilized • All should recieve O2 • Ceftriaxone – Cefotoxime- meropenem 7-10 days • CS or E are not effective Treatment: Epiglotitis • Indication for rifampin for household members if: - any centact < 48 mo of age incomplete vaccinated - Any contact < 12 mo of age not received the 10 vaccine series - Immuno-compromised child Bacterial tracheitis • Stap au.* - morexella cat.- Non typable HI- anerobic • Age: 5-7 y-o • 2nd to LT & viral infection is more common than 10 infection - Brassy cough- high fever- toxic – RD- not drool- can lie- no dysphagea • Need intubation in 50-60 % (younger children) - Major pathology: mucosal swelling in cricoid cartilage purulent secretion pseudomembrane Bacterial tracheitis • : diognosiS : Fever- purulent discharge- absence of epiglottitis finding • X-Ray is not needed but show classic finding • During ET intubation : pus below cord • Tx: Artificial airway is strongly suspected • Vancomycin + nafcillin • O2 suction Lateral neck radiograph showing intraluminal membranes and tracheal wall irregularity (arrows) consistent with bacterial tracheitis. Tracheotomy; Endotracheal Intubation • Epiglotitis mortality rate of 6% dropped to zero -In OR or in ICU -Tube 0.5-1 mm smaller than estimation - T, ET for most patient of bacterial tracheitis (5060%) - T, ET in LTB in outbreak of influenza A & measlse - Extubation :few days - T. complication: Mediastinal emphysema / pneumothorax - DL in epiglottitis: after 42 hr inflammation ↓, (2-3 days after antibiotic)