Scrotal Ultrasound
Tanya Nolan
Scrotal Anatomy
or Globus Major
Fused tubules that form efferent ducts
Thickened portion of tunica albuginea
(multiple septa)
Or Globus Minor
Covers testes
Tunica Vaginalis
Lines inner walls of
scrotum
2
Dartos Muscle and Raphe
3
Prostate
Seminal Vesicles:
Produce fluid rich in fructose
(energy source for sperm
motility after ejaculation)
Prostate Gland:
secretes a thick alkaline
substance that constitutes the
largest part of seminal fluid.
Alkalinity protects sperm from
acid present in the male urethra
4
and female vagina.
Vascular Supply
• ARTERIES
o Testicular Arteries
• Capsular Arteries
o Centripedal arteries
o Transmediastinal / Transtesticular
Artery
o Cremasteric and Deferential Arteries
o Pudendal Artery
• VEINS
o Pampiniform plexus
o Right Testicular Vein: drains into IVC
o Left Testicular Vein: joins the left renal
vein
o Deferential Vein
o Cremasteric Vein
5
Epididymis
• Head
o Superior to the upper pole of the
testis
o Contains 10-15 efferent ductules
from the rete testes
• Body, Tail
o Efferent ductules converge to
form Ductus Epididymis and
becomes the Vas Deferens which
joins the duct of the seminal
vesicles and forms the Ejaculatory
duct that empties into the Urethra
• Postvasectomy Changes
o 40% enlargement, inhomogeneity,
spermatoceles, dilation of rete testis, and
sperm granulomas
6
Spermatic Cord
• Extends from the scrotum, through the inguinal
canal and internal inguinal rings, to the pelvis
o
o
o
o
o
o
Vas Deferens
Testicular Arteries
Venous Pampiniform Plexus
Lymphatics
Autonomic Nerves
Fiber of the Cremaster
7
Function and Physiology
• Spermatogenesis
o Testicles
• Produce sperm in seminiferous tubules
o Epididymis
• Serves as a duct through which sperm pass
• Stores small quantities of sperm
• Secretes a small part of the seminal fluid (Semen)
• Secretion of Hormones
o Testosterone
• Secreted by Leydig cells
• Androgen or masculinizing hormone
8
Sperm Pathway
• Seminiferous Tubules
o Produce Sperm
• Tubuli Recti
• Rete Testes
• Efferent Ducts
o Connect testis to epididymis
• Vas Deferens
o Connect epididymis to the ejaculatory duct
• Ejaculatory Duct
o Seminal Vesicle ducts join Vas Deferens on each side to
form the Ejaculatory Duct
• Urethra
o Path by which spermatozoa and urine pass.
9
Songraphic Technique
• Transducer
o High frequency (10-14 MHz) Linear
o Lower frequency may be
considered when wall edema
and skin thickening is present.
o Trapezoid, virtual convex, and
panoramic views may be used in
cases of hydroceles, hematomas,
or swelling.
• Patient Position
o Supine with legs slightly apart and
support placed underneath
scrotum.
o Penis and upper thighs are
draped and positioned away
from scrotum.
10
Sonographic Technique
• Right and left testis and epididymis
are examined separately in both
sagittal and transverse planes
• Transverse plane images include
superior, middle, and inferior
scrotum.
o Measurement is obtained at widest diameter (24 cm in width)
o Compare echogenicity and scrotal skin
thickness
o Color Flow Doppler
• Sagittal images include medial and
lateral borders of scrotum.
• Length and AP measurements are obtained
at longest axis. (Length 3-5 cm & 3 cm in
AP)
• If patient has a lump/nodule. Have
patient trap it between fingers and
then scan the nodule.
Rete
Testis
11
Normal Testes & Raphe
• An image should be taken demonstrating
the raphe and comparing size,
echogenicity, and texture of each testicle.
12
Color Doppler
• Upper frequency range
improves sensitivity to slow
flow.
• Enhance visibility of perfusion
o
o
o
o
o
o
o
Gain
Scale / Pulse Repetition Frequency (PRF)
Wall Filter
Line Density
Threshold
Packet Size
Color box / Region of Interest
• Normal Spectral Doppler
o Low resistance waveform in intratesticular arteries. (A lowresistance waveform
demonstrates forward flow
during both systole and diastole.)
13
Indication for
Sonographic Examination
Painful scrotum
Scrotal trauma
Enlargement
Palpable Mass
Search for undescended testicle(s)
Follow-up for patients with a previous
orchiectomy or recent tumor
• Trauma
• Male infertility
•
•
•
•
•
•
14
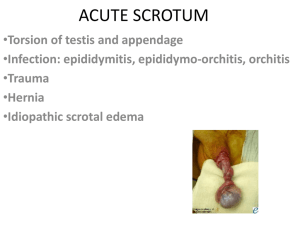
Pathology
Benign Conditions
15
Scrotal Trauma
•
•
•
Rupture of the testis is a surgical emergency.
If surgery is performed within 72 hours after injury, 90% of testes can be
saved. After 72 hours, only 45% can be saved.
Clinical Findings
o Pain
o Swelling
•
Sonographic Findings
o
o
o
o
o
Focal alteration of testicular parenchymal pattern; irregular contour
Interruption of the tunica albuginea
Scrotal wall thickening
Hematocele
Blood flow disruption across the surface of the testis
16
Hydrocele
• Abnormal accumulation of
fluid in the tunica vaginalis
o Clinical Findings
• Congenital or idiopathic
• Usually due to epididymitis
• Associated with orchitis,
spermatic cord torsion, and
trauma
o Sonographic Findings
• Located around the
anterolateral aspect of the testis
• Anechoic or low-level echoes.
17
Hydrocele and Testicular Appendix
The appendix testis is attached to the upper pole
of the testis between the epididymis and testis.
18
Hematocele
• Blood in scrotal sac
• Sonographic Indications
o Acute hematocele is
echogenic with many
visible echoes that can
float or move in real time.
o Aged hematoceles
become more complex
and show low level
echoes. They may also
develop a fluid-fluid level
or septations.
o Absent of blood flow
19
• Pus in scrotal sac
Pyocele
o Contains internal septations, loculations, & debris
o Increased vascular perfussion
20
Epididymitis
• Inflammation of epididymis
• Most common cause of acute scrotal
pain
• Clinical Findings
o Fever
o Dysuria with possible urethral
discharge
• Sonographic Findings
o Enlarged epididymis
o Thickened scrotal skin
o Decreased echogenicity with
course echo pattern
o Associated with hydrocele
o Increased Doppler flow
21
Orchitis
• Inflammation of the testis;
Infection may be focal or
diffuse
• Enlarged testis
o Severely swollen testis may
lead to testicular infarction.
• Decreased high resistance,
absent blood flow, or
Doppler waveforms
demonstrating reverse
diastolic flow is indicative of
testicular infarction.
• Sonographic Findings
o Affected areas appear
hypoechoic
22
Orchitis
6 months after diagnosis
o testicular atrophy
o skin thickness
• Normal skin wall thickness is 2-8
mm thick
Epidiymoorchitis
• A. Swelling
and Edema
• B. Hyperemic
Perfusion
• C. High
Resistance
Blood Flow
Abscess
• Most commonly caused
by untreated epidiymoorchitis
• Clinical Findings
o Fever
o Scrotal Pain
o Swelling
• Sonographic Findings
o Anechoic or complex mass
o Increased blood flow
around mass periphery
o No blood flow in mass
o Air within the space
indicated abscess
• Spermatic Cord becomes twisted and
cuts off blood supply
• Medical Emergency
o Surgery within 5-6 hours onset of pain (80100% testes salvaged); 6-12 hours onset of
pain (70% testes salvaged); after 12 hours
onset of pain (20% testes salvaged)
• The degree or number of twists also affects
testicular salvage
• Acute Symptoms
o Scrotal pain and swelling
o Nausea and vomiting
o Sonographic Findings
• Enlarged testicle
• Enlarged epididymal head
• Decreased echogenicity
• Chronic
o Sonographic Findings
•
•
•
•
Small heterogeneous testicle
Scrotal wall thickening
Possible hydrocele
No arterial flow
• Partial Torsion
o Sonographic Findings
• Reduced flow with possilbe increased flow
in the peritesticular soft tissue
• Must make comparison to contralateral
side.
Spermatic
Cord
Torsion
Spermatic Cord
Torsion
B
B
A. L testicle enlarged and
heterogenous
B. Mixed echopattern
caused by
hemorrhage, necrosis,
& vascular congestion
(torsion > 24 hours)
C. Absence of detectable
Color signal
Spermatoceles & Epididymal Cysts
Spermatocele
•
Cyst containing nonviable sperm and
proteinaceous fluid.
o Always Located in Epididymal Head
o More common following vasectomy
Epididymal Cyst
•
Cyst containing serous fluid
o Found anywhere within the epididymis
Sonographic Findings
o
o
o
o
Palpable
Clear, Simple, or Multilocular
Thin Walled
Posterior Acoustic Enhancement
Varicocele
• Enlargement of Veins
of Spermatic Cord
o Most common cause of
infertility
o Majority occur on the left
side due to venous
drainage (L renal vein)
o Large, right-sided
varicoceles may be
associated with renal
tumor
Varicocele
• Sonographic Findings
o Dilated Veins: More than 2mm in diameter
• Valsalva maneuver or having patient stand will increase
venous pressure and increase vessel diameter.
• Reversal Flow occurs when intra-abdominal pressure
increases
Intratesticular Cysts and Tubular
Ectasia of the Rete Testis
• Intratesticular Cysts
o More common in men over 40
o Associated with
spermatoceles
o Single, multiple, variable size
• Tubular Ectasia of the Rete
Testis
o Dilated tubules of Rete Testis
o Associated with
spermatoceles, epididymal or
testicular cysts, or other
epididymal obstruction
o Has the appearance of
intratesticular varicocele but
has NO FLOW
Epidermoid Cyst
• Rare benign lesion of
testis
o
o
o
o
Well Circumscribed
Hypoechoic
Lamellated
Little Flow
Scrotal Hernia
• Bowel, omentum, or
other structures
herniated into the
scrotum
• Sonographic Findings
o Peristalsis during real-time
o Fluid filled bowel loops
easily recognizable
Sperm Granuloma
• Chronic inflammatory
reaction to
extravasation of
spermatazoa
o Frequently seen in
patients with vasectomy
o Located anywhere
within epididymis or vas
deferens
o Sonographic Findings
• Well defined solid mass
• Hypoechoic or isoechoic
• Increased flow with color
Doppler when
inflammation is present
Microlithiasis
• Tiny calcifications < 3mm
within testis
o Bilateral
o Associated with testicular
malignancy and cryptorchidism,
Klinefelter’s syndrome, infertility,
varicoceles, testicular atrophy,
and male
pseudohermaphroditism
• Sonographic Finding
o Multiple bright nonshadowing foci scattered
through testis
Adenomatoid Tumor
• Most common extratesticular tumor
• Clinical Findings
o
o
o
o
Generally asymptomatic
Painless
Small, slow growing
Commonly in 5th decade
• Sonographic Findings
o
o
o
o
Well circumscribed, solid
Unilateral (usually left)
Variable echogenicity
Associated with hydrocele
Pathology
Malignant Conditions
Approximately 95% of all testicular neoplasms are
malignant!
Testicular Cancer
• Clinical Findings
o Painless; vague discomfort
o Unilateral enlargement
• Types
o Germ Cell Tumors
• Associated with elevated human chorionic gonadotropin and
alphafetoprotien
o
o
o
o
Seminoma
Embyonal carcinoma
Teratoma
Choriocarcinoma
o Stromal Cell Tumors
o
o
o
o
Leydig cell
Sertoli
Granulose
Theca cell
o Metastasis
o Lymphoma and Leukemia
Seminoma
• Most common germ cell
tumor
• Sonographic Findings
o Hypoechoic lesion
o Smooth border
o Cystic components or
calcification not common
Embryonal Carcinoma
o
o
o
o
o
Invasive; aggressive
Ill defined hypoechoic lesion
Possible capsular distorion
Associated hemorrhage, calcification,
and fibrosis
Teratoma
o Well defined
o Complex Mass
o Possible calcification with
acoustic shadowing
o Usually benign in children
Choriocarcinoma
o Mixed appearance depending on dominant cell type
o Typically irregular borders
Congenital Anomalies
• Cryptochidism
• Testicular Ectopia
• Anorchia
o Scrotum is empty
• Polyorchidism
o Increased risk of malignancy, cryptorchidism,
inguinal hernia, and torsion
o Duplicated testis are commonly small & efferent
spermatic system is completely absent
Cryptochidism
• The testicles do not
descend to their normal
position
o 80% are palpable and located
in the inguinal canal region
o 2.5-8 more times more likely to
develop cancer
o 10 times more likely for
spermatic cord torsion
• Surgical Treatment
needed because higher
temperature may prohibit
spermatogenesis and
result in infertility.
• http://www.medicalvideos.us/play.php?vid=2783