Scrotum and Testes
advertisement
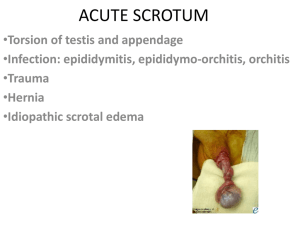
Sonography of Scrotum and Testes . Anatomy The scrotum is divided by the midline raphe. Each half of the scrotum contains a spermatic cord, testis, and epididymis. The testes descend into the scrotum at approximately the 28th gestational week via the inguinal canal through the peritoneal recess, which is called the processus vaginalis. The processus vaginalis gradually closes through infancy and childhood. The testis is covered by a visceral layer of tunica vaginalis, except where in contact with epididymis, and by the tunica albuginea. The posterior surface of the tunica albuginea extends into the testis to form the mediastinum testis. This is seen as a middle echogenic line on longitudinal US of the testis The testis has lobules containing the seminiferous tubules. Testicular lobules are occasionally identified as lines radiating from the mediastinum testis •The size and shape of the testes change with age. Testicular size is influenced by gonadal hormones. In boys, from birth to 5 months of age, the testicular volume rises to a maximum of 0.44 (±0.03) cm3. The rise in testicular volume coincides with a peak in gonadotropic hormones, so-called minipuberty, at approximately 3 to 4 months of age. After age 5 months, the testicular volume steadily declines and reaches its minimum volume at approximately 9 months of age and remains approximately the same size until puberty. The testis is rounded in newborns and gradually becomes ovoid with growth. •The epididymis has three parts: head, body, and tail. In the normal epididymis, only the head is routinely identified. The epididymal head is located in the upper pole of the scrotum, is triangular in shape, and has the same echogenicity as the testis. •Testicular appendixes are remnants of the mesonephric and paramesonephric ducts. They can be identified by US in cases of hydrocele •The spermatic cord appears as an echogenic band on longitudinal images and ovoid on transverse images as it passes in the inguinal canal. Color Doppler shows the testicular artery and pampiniform venous plexus .In the inguinal canal, the normal thickness of the spermatic cord is up to 4 mm. The normal inguinal canal does not contain fluid. Ultrasound (US) is a readily available and relatively inexpensive imaging modality that can be performed on patients at any age without the need for sedation or any other pretest preparation. US examinations are safe and there is no significant biologic risk from radiation exposure. Different pathologies of the scrotum may have similar clinical presentation, such as acute scrotal pain or scrotal mass. US of the scrotum can better guide treatment by improving the definition of the scrotal pathology. For these reasons, US became the imaging modality of choice for evaluation of scrotal pathology, and, in most cases, US is the first and only imaging needed for evaluation of scrotal pathology. •Color Doppler demonstrates capsular and intratesticular vessels. In prepubertal testes, it can be difficult to detect intratesticular flow, but the capsular arteries are easier to identify. It is, however. •The resistive index of the intratesticular arteries changes with age from high to low resistive index Indications for Scrotal Ultrasound • • • • • • • • • • Pain: trauma, inflammation, torsion Mass: testicular, extratesticular Evaluation of a possible hernia and its contents Search for occult neoplasm in cases of retroperitoneal or mediastinal lymphadenopathy Follow-up of previous infections, tumors, lymphoma, leukemia Small testes, atrophy Location of undescended testes Infertility Precocious puberty or feminization •The acute scrotum Acute scrotal pain is a medical urgency as 12% to 26% of boys who have it have testicular torsion. The main differential diagnosis includes testicular torsion, torsion of appendix testis, and epididymitis. It is crucial to rapidly diagnose testicular torsion because prognosis of the testis depends on the duration of torsion.[Ischemia of the testis can be reversible in the first 6 hours.[US is typically required when the clinical assessment is equivocal for testicular torsion. Testicular torsion typically presents as an acute, excruciating scrotal pain of short duration before a patient arrives in the emergency room. Physical examination typically reveals diffuse tenderness, abnormal high and horizontal position of the testis, and absence of the cremasteric reflex. Gray-scale findings of testicular torsion may be normal. Testicular gray-scale abnormalities include testicular swelling or heterogeneous or decreased testicular echotexture. Heterogeneous parenchymal echotexture usually indicates testicular nonviability. Other findings include swelling of the epididymis, hydrocele, and scrotal skin edema .Epididymal swelling is common in testicular torsion and, in a few cases, associated with increased epididymal flow. A gray-scale study should include evaluation of the spermatic cord. A coiled spermatic cord could be the only sign for testicular torsion as perfusion of the testis can be normal in partial torsion (<360°) or even increased in a case of torsion-detorsion. Evaluation of the spermatic cord increases the sensitivity for detection of testicular torsion. •Decreased testicular blood flow on a color Doppler study is the most sensitive finding that indicates testicular torsion. Testicular capsular blood flow may increase and erroneously suggest, in young boys, the presence of testicular perfusion. Therefore, prudent examination of intratesticular blood flow is necessary. • Spectral evaluation of the blood flow and documentation of venous and arterial wave flow are important. Initially, only venous flow may be absent. Comparing the intratesticular flow to the contralateral testis is important, as any decrease in perfusion or change in the waveform may be the first indication of testicular torsion Acute torsion of the testis Rates of testicular salvage by time from start of symptoms. Davenport, M. BMJ 1996;312:435-437 Copyright ©1996 BMJ Publishing Group Ltd. Torsion of Testicular Appendix The appendix testis, a müllerian duct remnant located at the superior pole of the testicle, is the most common appendix to twist. The epididymal appendix, located at the head of the epididymis, is a wolffian duct remnant. Torsion of testicular appendix can occur at any age but is most common between the ages of 7 and 12 years. The pain is typically indolent and not as severe as the pain from testicular torsion. Duration of scrotal pain is significantly longer than that of testicular torsion. A palpable tender nodule in the upper pole of the scrotum and the blue dot sign, which represents the bluish discoloration of the torsed appendix, are specific signs for torsion of testicular appendix. US typically demonstrates an extratesticular nodule with no vascularity in the upper pole of the scrotum. The maximal diameter of the torsed appendix varies from 4 to 16 mm. There may be an overlap between the size of torsed and normal appendixes when the nodule is smaller than 6 mm. The torsed appendix leads to secondary inflammation in the surrounding structures. The epididymis is almost always swollen with increased perfusion, and occasionally there is swelling and increased perfusion of the testis. Other findings include scrotal wall edema and hydrocele. In some cases, when the torsed appendix is not identified by US, the findings cannot be distinguished from acute epididymitis. Treatment includes analgesic and anti-inflammatory medications. Surgery is reserved for patients in excruciating pain who are not responding to medication or when it is not possible to clinically distinguish from testicular torsion. Scrotal appendages. (A) Appendix testis. (B) Appendix epididymis originating from the surface of an epididymal cyst. Both appendages are seen because of thepresence of peritesticularfluid. Arrow, appendages. EC, epididymal cyst Torsed appendix testis.enlarged avascular appendix testis surrounded by increased blood flow •Acute Epididymitis Epididymitis is an inflammation of the epididymis. Epididymitis is described in response to infection, trauma, vasculitis, or urine refluxing into the ejaculatory ducts but in most cases is idiopathic.The diagnosis is often based on clinical presentation of a few days of acute scrotal pain, swelling, and tenderness of the epididymis. Presentation in young boys and those with recurrent epididymitis should lead to further evaluation with renal US and cystourethrography for associated anomalies. Anomalies that are described in association with epididymitis include ectopic ureter to the seminal vesicles and lower urinary tract anomalies, such as recto-ureteral fistula and strictures of the urethra. Recurrent epididymitis can also occur in boys with neurogenic bladder or functional bladder abnormalities. Gray-scale US findings of epididymo-orchitis include an enlarged epididymis. The echotexture of the epididymis varies, depending on time of evolution, from decreased to increased echogenicity. Inflammation of the testis, orchitis, is confirmed by enlarged testis with heterogeneous echotexture. Indirect signs of inflammation, such as reactive scrotal wall edema and hydrocele, are present in most cases. Duplex US demonstrates hyperemia of the epididymis and, when orchitis is present, increased testicular perfusion. Acute epididymitis Epididymo-orchitis Trauma: The scrotum and its contents may be injured by penetrating or blunt trauma. Surgical exploration is performed after penetrating trauma, whereas ultrasound examination is indicated after blunt trauma .Under these circumstances,the main role of ultrasound is in the diagnosis of testicular rupture. Early surgical exploration and repair of a ruptured testis improve testicular survival because the salvage rate is over 80% when the testis is repaired within 72 hours,but it drops to 30% thereafter .Reported accuracy in the diagnosis of rupture of the testis is in the range of 94% to 100%. Missed or untreated rupture of the testis may result in an ischemic atrophic testis or secondary infection. In addition, in cases of unilateral testis trauma, which might or might not include orchiectomy as treatment, it has been shown that patients might develop subfertility in association with apoptosis (cell self-destruction by fragmentation of the nuclear DNA) and abnormal sperm. Rupture of the testis Scrotal hematoma with testis rupture . scrotal wall infiltration (arrows) and heterogeneous testis on the right side. The left side is normal. •Germ cell tumors: Tumors showing a single cell type: Seminoma Typical Anaplastic Spermatocytic Embryonal carcinoma Adult type Infantile type Polyembryoma Choriocarcinoma Teratoma Mature and immature Tumors showing more than one histologic pattern: Embryonal carcinoma plus teratoma (teratocarcinoma) Embryonal carcinoma plus seminoma Seminoma and teratoma Other combinations •Tumors of gonadal stroma: Leydig cell tumors Sertoli cell, granulosa cell, theca cell tumors Tumors of primitive gonadal stroma Mixtures of these three Adult Unilateral (Occasionally Bilateral) Tumors of the Testis Classic seminoma in a 46-year-old patient Testicular teratoma in an infant Embryonal cell carcinoma predominant in a mixed-cell tumor Abdominal Burkitt's lymphoma with metastasis to the testes Non-Hodgkin large B-cell lymphoma in a 66-year-old patient Large paratesticular rhabdomyosarcoma in a 14-year-old boy Chronic epididymitis mimicking a paratesticular mass in a 2year-old boy •Cryptorchydism Cryptorchydism occurs in approximately 3% of term male infants with spontaneous descent in two-thirds of the cases. The incidence of cryptorchydism rises with prematurity because testicular descent usually occurs in the seventh month of gestation. Orchiopexy prevents torsion of the cryptorchid testis and reduces the risk of trauma to the testis. The exact relationship of fertility to cryptorchydism and subsequent orchiopexy is controversial. Boys with cryptorchydism have increased risk of testicular cancer. Orchiopexy may allow earlier detection of testicular tumors, but it is controversial as to whether or not orchiopexy reduces the risk of testicular cancer.[ Approximately 20% of undescended testes are nonpalpable and most of them are located in the inguinal canal .US is highly sensitive for identifying the inguinal undescended testis. Using US to guide the surgical approach saves most boys from the need for laparoscopy. •Inguinal hernia and hydrocele: Obliteration of the processus vaginalis occurs after the seventh month of gestation. Failure of the processus vaginalis to obliterate can result in passage of peritoneal fluid, leading to hydrocele or intestinal loops, or omentum, leading to inguinal hernia. The incidence of congenital inguinal hernia is between 0.8% and 4% of live births. The risk of incarceration is up to 60% in the first 6 months of life. Right inguinal hernias are more common as the right processus vaginalis closes later. US can be helpful for inconclusive physical examination or to evaluate for contralateral involvement. US can show bowel loops in the inguinal canal or scrotum, and during real-time imaging it can demonstrate peristaltic activity or movement of fluid and air bubbles. Omental hernia is seen as a continuous echogenic structure from the pelvis to the inguinal canal or scrotum. A clinically occult contralateral hernia can be found in 88% of cases. Congenital hydrocele appears as fluid collection surrounding the anterolateral aspects of the testis, sometimes extending to the inguinal canal. When the processus vaginalis is completely patent, the hydrocele is communicating. This leads to elective repair. The processus vaginalis may obliterate at any point leading to various types of hydroceles. Closure of the processus vaginalis below the internal inguinal ring leads to noncommunicating hydrocele, which usually resolves by the age of 1 year. Closure of the processus vaginalis below the internal inguinal ring and above the testis leads to spermatic cord hydrocele. A rare type of hydrocele is referred to as abdominoscrotal hydrocele. This is a large communicating hydrocele that protrudes through the internal inguinal ring into the abdominal cavity and appears as a pelvic cystic mass. Normal anatomy of the inguinal canal Omental hernia in a 16-year-old boy Inguinal hernia containing bowel •Testicular Calcifications: Testicular calcifications are of different types. Isolated calcifications with no associated findings are common and may represent benign phleboliths, fibrosed-calcified spermatic granulomas, the end result of previous epididymoorchitis, or trauma. They are of no clinical significance. A different situation arises when the calcifications are multiple, minute, and grouped. They should be considered highly suggestive of malignancy. Necrotic or hemorrhagic areas in germ cell tumors may calcify. Embryonal carcinoma is the most common tumor to present with necrosis and hemorrhage, whereas seminomas rarely necrose and calcify. Calcifications may also be seen with teratoma, but in this case they represent calcified cartilage or bone fragments. Testicular microlithiasis is an uncommon, usually incidental, finding. It is caused by the formation of microliths from degenerating cells in the seminiferous tubules. Microlithiasis may occur in healthy patients, but it has also been found in nonneoplastic conditions such as Klinefelter’s syndrome, Peutz-Jeghers syndrome, cryptorchidism, postorchiopexy testis, testicular infarcts, granulomas, subfertility, infertility, male pseudohermaphroditism, Down’s syndrome, and pulmonary alveolar microlithiasis. Testicular microlithiasis has been associated with germ cell tumors: seminomas, seminoteratoma , and intratubular germ cell neoplasia . In cases of seminoma with pathologic correlation, the area of microlithiasis was confined to the nontumoral portion of the testis. Because of the described association of microlithiasis with neoplasia, the ultrasound diagnosis of microlithiasis should warrant more aggressive follow-up. Bilateral microlithiasis of the testes Seminoma (calipers) in a patient with testicular microlithiasis •Varicoceles are a dilation and tortuosity of the pampiniform plexus veins in the spermatic cord or the epididymis .Most varicoceles are primary and affect adolescents and young adults. They usually involve the left side, a finding attributed to the drainage pattern of the more tortuous left internal spermatic vein into the left renal vein. Bilateral varicoceles have been reported with an incidence varying from 10% to 70%. Secondary varicoceles result from increased intra-abdominal pressure such as from hepatosplenomegaly and abdominal masses. They are less frequent. An acute onset on either side, a right varicocele, or a varicocele in a mature man raises the possibility of an abdominal or pelvic mass. Varicocele is the most common single, correctable cause of male infertility, and it is found in 37% of patients with this problem. Two or more tortuous, sonolucent tubular structures with a caliber of 2 mm or more are seen as the hallmark findings in varicoceles. On the basis of the Doppler tracing during a Valsalva maneuver, varicoceles have been classified in two types. The stop type shows only retrograde blood in the internal spermatic vein. An explanation for this situation is the presence of competent valves in the pampiniform plexus. Small and subclinical varicoceles are usually of this type. The shunt type shows both retrograde and antegrade (physiologic) blood flow in the same vein. This phenomenon is explained by the presence of incompetent valves in the pampiniform plexus that allow communication and collateral circulation by way of the deferential and cremasteric veins. Moderate-to-large varicoceles display this pattern. Ali shahbazi