Testis, epididymis, vas deferens and spermatic cord
advertisement

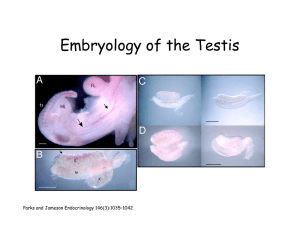
Dr Rania Gabr Dr. Safaa Ahmed OBJECTIVES Define the testis. Describe its normal site, size, shape & relation. Discuss its covering. Discuss its blood and nerve supply. Mention its lymphatic drainage. Define the epididymis. Describe its site, position & parts. Discuss its blood and nerve supply. OBJECTIVES Mention its lymphatic drainage. Define the vas deferens. Describe its beginning and termination. Discuss its course, relation, blood and nerve supply. Mention its lymphatic drainage. Enumerate the contents (structures) of the spermatic cord. Components of Male Reproductive System I- Primary Sex Organ: Testis. II- Reproductive Tract: Epididymis. Vas Deferens. Spermatic cord. III- Accessory Sex Glands: Seminal vesicles. Prostate gland. Bulbourethral glands. IV- External genitalia: Penis Testis Paired almond-shape gonads that are suspended in the scrotum by the spermatic cord 4 - 5 cm long Weigh (10.5 – 14) g sc Functions:: Spermatogenesis. Hormone production (Androgens- testosterone). T -It develops in the abdomen; descends into the scrotum before birth; -It is made up of tightly coiled tubes (SEMINIFEROUS TUBULES) where sperm are formed; -scattered between tubules are the LEYDIG CELLS (produce testosterone and other androgens). (Leydig cells) TESTIS Coverings of the Testis Tunica Vaginalis: - It surrounds testis & epididymis. - Derived from the abdominal peritoneum - It allows free movement of testis inside scrotum. Tunica albugenia: It is a whitish fibrous capsule T.Vag. Parietal & visceral Internal Structure of Testis Fibrous septae extend from the capsule, divide the testis into a (200-300) lobules. Each lobule contains, (1-3) seminiferous tubules. Seminiferous Tubules: - They are the site of the spermatogenesis. - They form the bulk of testicular tissue. Rete testis: - (a network of tubules) - It is the Site of merging of the Seminiferous tubules. RT Blood Supply of Testis Testicular artery: It is a direct branch from the abdominal aorta. Testicular Artery Venous drainage : (Pampiniform plexus of veins.) - Approximately a dozen veins which forms a network in the spermatic cord. - They become larger, converge as it approaches the inguinal canal and form the Testicular vein. Right Testicular vein Vein drains into IVC. Left Testicular vein Vein drains into Left Renal Vein. Testicular Lymphatics: Follow arteries, veins end in Lumbar (par aortic) nodes From scrotum, penis, prepuce: Terminate in Superficial Inguinal nodes Epididymis A Single coiled tubule 6 M long Located on the posterior & superior margins of the testis. It is divided into: Head, Body and Tail. The Head receives efferent ductules from testis. The Tail is continuous with Vas Deferens H V D B Functions: 1. Secretes/absorbs the nourishing fluid. 2. Recycles damaged spermatozoa. 3. Stores spermatozoa Up to 2 weeks to allow for maturation It is the site where sperms become motile and gain the ability to fertilize. Vas Deferens A Muscular tube 45 cm long. Carries sperms from the Epididymis to pelvic cavity. Passes through the inguinal canal It crosses the ureter Its terminal part is dilated to form the Ampulla of the vas It joins the urethra in the prostate Vas deferens Spermatic Cord - The spermatic cord is a collection of structures that pass from each testis through the inguinal canal to the abdominal cavity. Coverings 1- External spermatic fascia 2- Cremasteric fascia 3- Internal spermatic fascia Structures (Contents) of the Spermatic Cord 1- Vas deferens 2- Testicular artery 3-Testicular veins (pampiniform plexus) 4- Testicular lymph vessels 5- Autonomic nerves 6-Remains of the processus vaginalis 7- Genital branch of the genitofemoral nerve, which supplies the cremaster muscle Processus Vaginalis Is a pouch of peritoneum that is carried into the scrotum by the descent of the testicle and which in the scrotum forms the tunica vaginalis Thank you