Haemophilus Meningitis in an African Neonate
advertisement
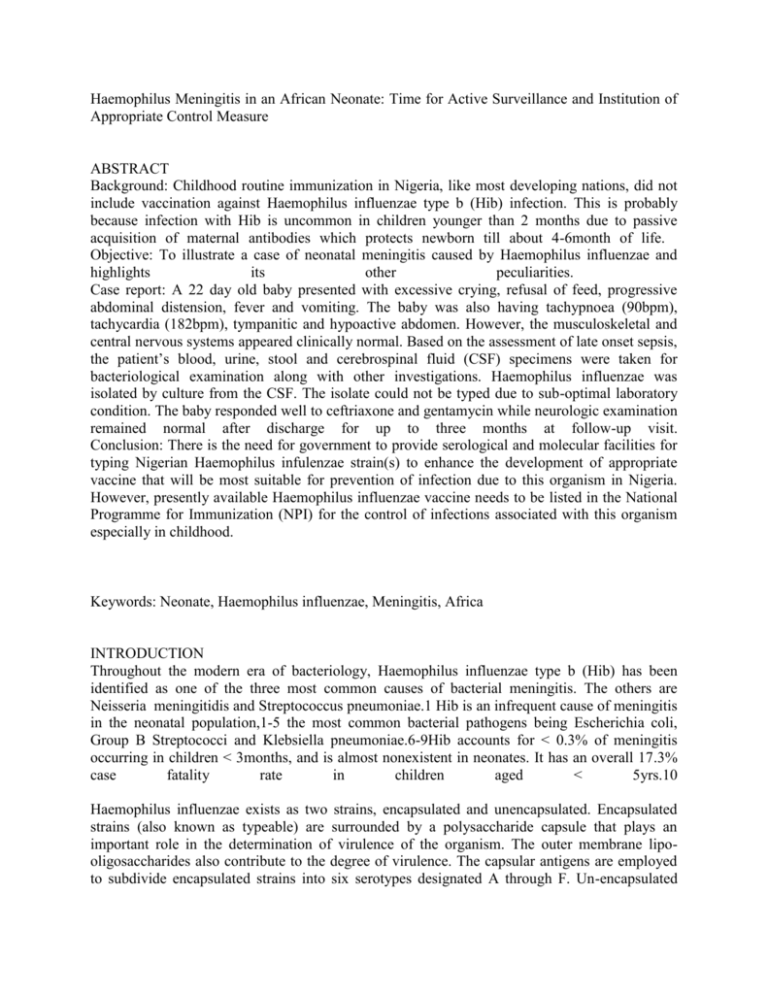
Haemophilus Meningitis in an African Neonate: Time for Active Surveillance and Institution of Appropriate Control Measure ABSTRACT Background: Childhood routine immunization in Nigeria, like most developing nations, did not include vaccination against Haemophilus influenzae type b (Hib) infection. This is probably because infection with Hib is uncommon in children younger than 2 months due to passive acquisition of maternal antibodies which protects newborn till about 4-6month of life. Objective: To illustrate a case of neonatal meningitis caused by Haemophilus influenzae and highlights its other peculiarities. Case report: A 22 day old baby presented with excessive crying, refusal of feed, progressive abdominal distension, fever and vomiting. The baby was also having tachypnoea (90bpm), tachycardia (182bpm), tympanitic and hypoactive abdomen. However, the musculoskeletal and central nervous systems appeared clinically normal. Based on the assessment of late onset sepsis, the patient’s blood, urine, stool and cerebrospinal fluid (CSF) specimens were taken for bacteriological examination along with other investigations. Haemophilus influenzae was isolated by culture from the CSF. The isolate could not be typed due to sub-optimal laboratory condition. The baby responded well to ceftriaxone and gentamycin while neurologic examination remained normal after discharge for up to three months at follow-up visit. Conclusion: There is the need for government to provide serological and molecular facilities for typing Nigerian Haemophilus infulenzae strain(s) to enhance the development of appropriate vaccine that will be most suitable for prevention of infection due to this organism in Nigeria. However, presently available Haemophilus influenzae vaccine needs to be listed in the National Programme for Immunization (NPI) for the control of infections associated with this organism especially in childhood. Keywords: Neonate, Haemophilus influenzae, Meningitis, Africa INTRODUCTION Throughout the modern era of bacteriology, Haemophilus influenzae type b (Hib) has been identified as one of the three most common causes of bacterial meningitis. The others are Neisseria meningitidis and Streptococcus pneumoniae.1 Hib is an infrequent cause of meningitis in the neonatal population,1-5 the most common bacterial pathogens being Escherichia coli, Group B Streptococci and Klebsiella pneumoniae.6-9Hib accounts for < 0.3% of meningitis occurring in children < 3months, and is almost nonexistent in neonates. It has an overall 17.3% case fatality rate in children aged < 5yrs.10 Haemophilus influenzae exists as two strains, encapsulated and unencapsulated. Encapsulated strains (also known as typeable) are surrounded by a polysaccharide capsule that plays an important role in the determination of virulence of the organism. The outer membrane lipooligosaccharides also contribute to the degree of virulence. The capsular antigens are employed to subdivide encapsulated strains into six serotypes designated A through F. Un-encapsulated strains lack the polysaccharide capsule and are designated untypeable strains.6-7 Most invasive infections are caused by encapsulated strains of Haemophilus influenza and in particular the B serotype. The polysaccharide capsule of these organisms not only confers virulence and invasiveness, but it also provides resistance to opsonization and complement-mediated bactericidal activities and inhibits neutrophil phagocytosis. It is also the source of the antigen used in vaccine formulation. Neonates are generally at greater risk of sepsis and meningitis than other age groups largely due to deficiency in humoral and cellular immunity. This may be in form of defective phagocytic function, reduced maternal antibody transfer in babies less 32 weeks gestation, defective alternative complement pathway which compromises their defence against encapsulated bacteria. T-cell defence and mediation of B-cell activity also are compromised along with deficient migration and phagocytosis by neutrophils in the neonatal period. 7-8 Diagnosis of meningitis in neonates could be difficult due to its non-specificity of signs and symptoms.8 However, diagnosis of meningitis is established when at least two out of four laboratory criteria are fulfilled. 9 The criteria include: isolation of the cause by CSF culture, elevation of CSF leukocyte count more than 20cell/ mm3 with predominance of polymorphonuclear leukocytes in the CSF, hypoglycorrhachia and identification of bacteria by the Gram stain of CSF. Other important parameters useful in diagnosis and monitoring of response to treatment in meningitis include CSF/ blood sugar and CSF protein. The purpose of this communication is to sensitize medical practitioners about the occurrence of Haemophilus influenzae meningitis in the neonatal period and alert policy markers on the need to institute preventive measures. Case Report Baby OD, a 22 day old term female who presented at the neonatal intensive care unit of the University of Ilorin Teaching Hospital, Ilorin with history of excessive crying, irritability and refusal of feeds for 3 days, progressive abdominal distension for 2 days and fever for one day with an episode of vomiting just before presentation. Stools were of normal consistency but frequency had reduced from the usual three to four times to once daily. Her feeds had consisted of breast milk and water since birth. There were no adverse perinatal events. Her parents belonged to the high socioeconomic class. The family of four lived in a well-ventilated three bedroom apartment. On examination, she was acutely ill-looking but not irritable, pale, anicteric, febrile with an axillary temperature of 39.80C. She was appropriately sized with a weight of 3.4kg, occipitofrontal (OFC) of 38cm, and length of 51 cm. Gaseous abdominal distension without palpable organomegaly was observed. She was tachypnoeic with a respiratory rate of 90cycles per minute but there was no chest wall retraction and breath sounds were vesicular bilaterally. There was a tachycardia of 182 beats per minute but the heart sounds were normal. The anterior fontanelle was patent and normotensive. There was mild head lag but muscle tone and primitive reflexes were normal. The working diagnosis was late onset neonatal sepsis with the possibility of meningitis and partial intestinal obstruction. Lumbar puncture yielded turbid cerebrospinal fluid with relative hypoglycorrhacchia (1.0mmol/L compared to blood sugar of 4.4mmol/L), modestly elevated protein content (91mg/dl) and pleocytosis (280cells/mm3 mostly polymorphonuclear cells). Gram negative coccobacilli were seen and the culture yielded Haemophilus influenzae. The isolate was sensitive to Ciprofloxacin, Cefuroxime, Ceftriaxone, Ceftazidime and Augmentin. Other investigations revealed anaemia (PCV = 26%), normal peripheral blood leucocyte count (4.0 X 109/L) but with mostly neutrophils (84%), normal platelet count (463 X 109/L). Serum electrolytes and creatinine were within reference range. Abdominal ultrasound scan and plain abdominal radiography revealed normal findings. The blood culture was sterile. She was placed on supplemental oxygen by face mask, intravenous 10% dextrose in 0.18saline, intramuscular Ceftriaxone 100mg/kg/day, Gentamycin 5mg/kg 12 hourly, and Dexamethasone 0.5mg/kg stat, then 0.2mg/kg/dose 8 hourly for 48hours. A repeat CSF examination at about 48 hours of initiating treatment gave almost similar CSF biochemistry and cell count results but no organism was cultured though few gram negative coccobacili were seen on gram stain. The baby had first episode of subtle seizure at 24hours on admission, then had several episodes characterised by lip smacking and staring gaze. Intramuscular Phenobarbitone was prescribed at a dose of 15mg/kg stat and 2.5 mg/kg/dose 12 hourly. Phenobarbitone was discontinued and feeding commenced on fourth day of admission after baby had been seizure free for >48hrs. The fever abated on the sixth day. Gentamycin was discontinued on day 7 and baby had become stable enough to be discharged home. Her occipitofrontal circumference (OFC) remained constant and within normal range throughout admission. She continued to receive Ceftriaxone on out-patient basis for the next 7 days, totalling 14 days on medication. Transfontanelle ultrasound scan was normal on completion of antibiotics. She remained clinically normal on neurologic examination at the outpatient clinic during the first three months after discharge. Unfortunately, her parents defaulted on subsequent follow up visits. DISCUSSION Haemophilus influenzae was first identified in culture by Pfeiffer in 1892.1 The designation influenza bacillus was applied because he mistakenly thought that it was the cause of the influenza pandemic of 1890. The genus designation Haemophilus, indicating the hemophilic or blood-loving characteristic of Haemophilus influenzae was applied because growth of the organism in culture requires the presence of whole blood factors V and X.1,11- 12 Transmissibility of Haemophilus influenzae infection and the capacity of this organism to cause purulent meningitis were first demonstrated by Wollstein in 1911. 1 She first drew attention to the marked tendency for Haemophilus influenzae meningitis to occur in infants and young children. The child in focus presented with non-specific symptoms and signs as well as paucity of central nervous system symptoms and sign such as tense and bulging anterior fontanelle. This underlines the need for a high index of suspicion for the possible occurrence of meningitis in sick neonates. Indeed, the appearance of neurologic signs is often an indication of late presentation and has grave consequences for long term prognosis. Meningitis remains one of the leading causes of cerebral palsy and mental retardation in this environment. Though we did not have the privilege to follow the child up till the end of the first year of life, the short duration during which follow up occurred showed the possibility of a normal neurologic outcome. An unusual organism was responsible for the meningitis in this child with particular reference to age. Infection with Hib is uncommon in children younger than 2 months, probably because of passive acquisition of maternal antibodies which protects newborn till about 4-6month of life. 1, 12 Children that develop Hib disease most likely acquired the organism from other children (contacts) in day care centres, schools, as less than one percent of adults have nasopharyngeal colonization with Haemophilus influenzae.1 In the index case, the disease was probably contracted from an adult contact since the baby was not yet mixing with other children. The infrequency of Hib infection in young infants is related to the degree of protection conferred by transplacentally acquired maternal antibodies. These antibodies decay with time, thus exposing the older infant to the risk of infection. It is likely therefore that there was low level of maternal antibody transfer or rapid decay of maternally transmitted antibodies in the index case. The occurrence of this infection in a neonate may acquire greater significance if it does represent a new trend. Policy changes may be needed to cope with the situation. It may for example be necessary to incorporate routine typing of the organism into our laboratory techniques so as to identify which strain is responsible for infection in these young infants. Secondly, routine vaccination against Hib may have to be included in the national programme so as to prevent the devastating consequences of infection due to this organism. In Nigeria like most African countries, vaccine for the control of Haemophilus influenzae infections is not included in the national programme on immunization as against the practice in the USA and other developed nations. This probably may be related to the unknown national and continental prevalence, morbidity and mortality rates for infections due to Haemophilus influenzae. Furthermore, Haemophilus influenzae isolates are not routinely typed in our environment and the Haemophilus influenzae recovered from the baby in question was not typed. There is therefore the need for active surveillance system for Haemophilus influenzae related infections in Nigeria. In conclusion, there is need for continuous high index of suspicion for meningitis in the newborn. The reported case seems to be a relatively benign course of a highly invasive organism. Are there environmental issues that have resulted in this reported case? Findings call for diligent survey, provision of necessary laboratory needs and probably, inclusion of appropriate vaccine among childhood immunization in Nigeria. REFERENCES 1. Rust RS. Haemophilus influenzae meningitis. www.emedicine.com assessed on 6th October, 2006. 2. Kimberlin DW. Meningitis in the Neonate. Curr Treat Options Neurol. 2002; 4 : 239-248. 3. Anh DD, Kilgore PE, Kennedy WA, Batmunkh N, Long HT, Jodar L et al. Haemophilus influenzae type B meningitis among children in Hanoi, Vietnam: Epidemiologic patterns and estimates of H. influenzea type B disease burden. Am. J. Trop. Med. Hyg.2006;74(3):509-515. 4. Commey JO, Rodrigues OP, Akita FA, Newman M. Bacterial meningitis in children in southern Ghana. East Afr Med J. 1994;71(2):113-7. 5. Metha N, Pollard AJ. Meningitis-Bacterial meningitis. Hosp Pharm. 1999;6:258-63. 6. Department of Vaccines and biologicals. Estimating the local burden of Haemophilus influenzae type b (Hib) disease preventable by vaccination. A rapid assessment tool. WHO 2001. 7. Bachiller LP, Eiros BJM, Blanco QA. Clinical manifestations, diagnosis and treatment of Haemophilus influenzae infection.Ann Med Interna. 2000; 17(4):204-12. 8. Laving AM, Musoke RN, Wasunna AO, Revathi G. Neonatal bacterial meningitis at the newborn unit of Kenyatta National Hospital. East Afr Med J. 2003 ; 80(9):456-62. 9. Igniatovic M. Bacterial causes of meningitis in newborns. Srp Arh Celok Lek. 2001; 129 Suppl 1:36-41 10. Vaccines and Biologicals. Haemophilus influenzae type b (Hib) meningitis in the prevaccine era: a global review of incidence, age distributions, and case-fatality rates. WHO 2002. 11. Cheesbrough M. District Laboratory Practise in Tropical Countries. Part 2. Cambridge University Press. United Kingdom. 2000: 201-203. 12. Crawford SE, Daum RS. Haemophilus influenzae In: Behrman RE, Klimegman RM, Jenson HB, Stanton BF eds Nelson Textbook of Paediatrics. Saunders, Philadelphia: 2007; 904-7.