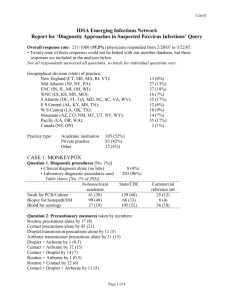
Infection control basics and introduction to the WHO policy
advertisement

Unit 3. Infection control (IC) basics and the WHO set of measures for TB IC TB Infection Control Training for Managers at National and Subnational Level Objectives After this unit, the participant will • understand the mechanisms of TB transmission • be able to describe the factors affecting the risk of TB transmission (patient, recipient, bacterial and institutional factors) • be able to list the WHO set of measures for TB infection control 2 Standard precautions • Use with every patient, at every health care visit Main elements include: • – – – – – Hand hygiene Respiratory hygiene, cough etiquette Use of personal protective equipment to avoid direct contact with patient’s blood, body fluids, secretions, and non intact skin Prevention of needle stick/sharp injury Cleaning and disinfection of the environment and equipment 3 Additional precautions Added to standard precautions depending on transmission mode of the patient’s suspected pathogen: • Airborne (measles, chickenpox) • Droplet (SARS, avian influenza) • Contact (staphylococcus aureus) 4 Airborne vs. droplet transmission Airborne • Small droplet nuclei <5 microns diameter • Stay suspended in air • When inhaled, can reach the alveoli and cause infection Droplet • Large droplets > 5 microns in diameter. • Do not remain suspended in the air, so no special air handling or ventilation is required • If inhaled, do not reach alveoli 5 Fate of droplet nuclei vs. droplets Droplet nuclei (airborne transmission) • A 1.0 μm droplet nucleus will settle at a rate of 0.0035 cm/sec (or 3 m in 24 hours) Large droplets (droplet transmission) • Fall to ground or other horizontal surface relatively fast 6 A sneeze 7 Number and size of organisms Number of organisms released Talking 0-200 Coughing 0-3,500 Sneezing 4,500- 1,000,000 Size of the droplets (function of air velocity) Sneeze ~3-10 m/s 75% are ~10 μm in diameter < 25% are droplet nuclei (1-5 μm in diameter). Wells 1955, Duguid 1945, Wells/Riley 1961, et al. 8 Airborne precautions • Place patient in airborne precaution room which has: – 12 or more air changes per hour – Control of airflow direction • Limit the movement of the patient – Ensure patients wear a surgical mask if outside their rooms • Use a particulate respirator whenever entering and providing care 9 What is the risk for TB transmission? 10 Who can infect whom? Patient to Worker to Visitor to Patient Worker Visitor 11 Factors affecting the risk of transmission • • • • Patient Recipient Bacterial Institutional 12 Patient factors • Infectiousness: sputum smear, cavitation, force and frequency of cough* • Cough-inducing procedures • Treatment (time since start of correct treatment and adherence)* • Understanding of TB, cough etiquette*, and adherence to IC practices • General health status (immune status,* nutrition, co-morbidities, e.g. diabetes) *Influence the number of infectious bacilli released 13 When is TB most infectious • When it occurs in the lungs or larynx • Until the person has – Completed at least 2 weeks of appropriate therapy, preferably with direct observation – Has become smear negative – Has improvement in symptoms 14 Recipient factors • Closeness, duration and frequency of contact* • Risk of TB infection (prior treatment, age, homelessness, contact of known case, etc.) • Adherence to IC practices* • Susceptibility either intrinsic or acquired (i.e. immune status, general health, other diseases, nutrition, age) *Influence dose of inhaled bacilli 15 Recipient factors 16 Bacterial factors • Intrinsic virulence of MDR-TB bacilli may not be greater than drug susceptible bacilli • However, patients with MDR-TB may infect more people due to their prolonged period of infectiousness • Previously treated cases (treatment failure, default, relapse) have increased levels of MDR-TB 17 Institutional factors (1) • Exposure in small, enclosed spaces • Lack of adequate ventilation • Re-circulation of contaminated air 18 Institutional factors (2) • Fixed characteristics (type, location, structure) • Variable characteristics (temperature, humidity, rain) • Type and number of people served by institution (crowding) • Resources available • Policies and practices governing patient movement and housing • Time lag between detection of disease or drug resistance (reporting and proper treatment) 19 Institutional factors 20 Institutional factors (3): path of the patient • • • • • • In-patients versus out-patients Diagnosed TB cases vs. undetected Intake, triage, registration Waiting area Laboratory, radiology, pharmacy High risk procedures 21 Areas visited by TB patients Reception General wards Home/referral clinics OPD TB Department VCT Maternity ward Unsuspected TB patients Radiology TB wards Laboratory Pharmacy Other departs 22 Institutional factors (4) path of the specimen • • • • • • • • Collection location and procedures Registration and identification number Storage Transportation Lab log entry Processing procedures Smear, culture, drug susceptibility testing Disposal procedures 23 Reorganization for optimal services (functionality) • • • • Maximise infection control Minimize risk of TB transmission Maximise quality of patient services Minimize cost (capital and recurring) 24 Set of measures for TB infection control, WHO, 2009 1. National and subnational levels • Managerial activities 2. Facility level • • • • Managerial activities Administrative controls Environmental controls Personal protection 25 What are managerial activities? Activities used by programme managers to support and facilitate the • implementation • operation • maintenance • evaluation of TB infection control at the national, subnational and facility levels 26 Managerial activities —national level (1) • Identify and strengthen a coordinating body • Develop a comprehensive plan for IC to include – Budget – Human resource requirements • Ensure that health facility design, construction, renovation and use are appropriate 27 Managerial activities —national level (2) • Conduct surveillance of TB disease among health care workers • Assess TB transmission risk at all levels of the health system and congregate settings • Address advocacy communication and social mobilization (ACSM), engagement of civil society • Monitor and evaluate TB IC measures • Enable and conduct operational research 28 Set of measures--facility level • • • • Managerial activities Administrative controls Environmental controls Personal protective equipment 29 Managerial activities at the facility level • • • • • • Identify and strengthen coordinating body, develop facility plan Rethink use of available spaces Assess facility, conduct surveillance of TB disease among health workers Address ACSM for health workers, patients and visitors Monitor and evaluate set of TB IC measures Participate in research efforts 30 Administrative controls— facility level • Promptly identify people with TB symptoms (triage), • Separate them • Cough etiquette • Minimize time in health care settings. • Provide a package of prevention and care for health workers, including HIV prevention –For HIV-positive health workers, antiretroviral therapy and isoniazid preventive therapy 31 Environmental controls— facility level Reduce the concentration of infectious particles in the air via: • Ventilation – Natural, mechanical, or mixed mode – Can direct the flow of infectious air away from health care workers and other patients • Ultraviolet germicidal irradiation (UVGI) 32 Personal protective equipment Use particulate respirators • Along with administrative and environmental controls • In situations where there is an increased risk of TB transmission • With comprehensive training program • With fit testing 33 Controls work at different points of the chain of transmission Patient coughs droplet nuclei into air (administrative controls) Droplet nuclei are suspended in the air (environmental controls) Exposed person breathes in M. tuberculosis (particulate respirators) 34 Priority measures for IC Control Why? 1 Administrative Prevent the generation of droplet nuclei. First line defence. 2 Environmental 2nd line defence, since cannot eliminate all TB exposure. 3 Particulate respirators Use only with the other 2 controls, in situations with a high risk of TB transmission. Protect only the health care worker, not other patients or visitors Managerial IC activities are required for all facilities 35 Summary • TB is spread through droplet nuclei that stay airborne for prolonged periods, and can be inhaled • Patient, recipient, bacterial and institutional factors influence the risk of TB transmission • WHO recommends a set of TB infection control measures including managerial, administrative, environmental, and personal protective equipment 36