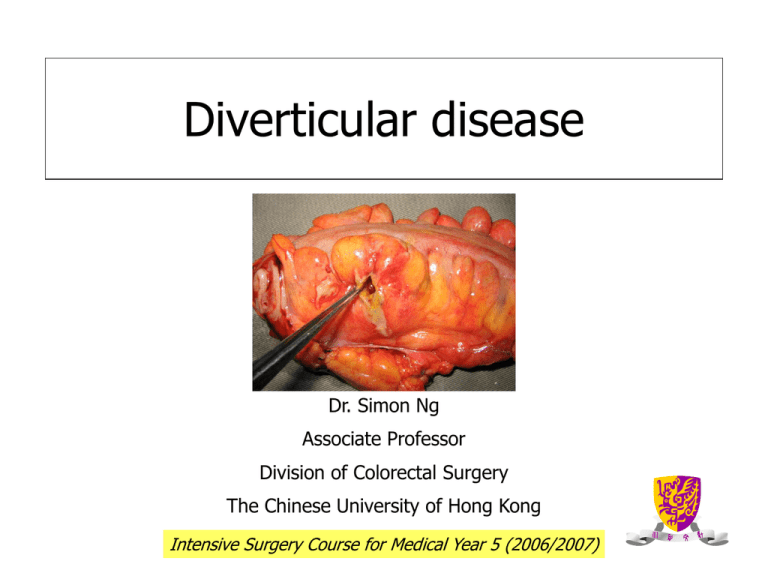
Diverticular disease
Dr. Simon Ng
Associate Professor
Division of Colorectal Surgery
The Chinese University of Hong Kong
Intensive Surgery Course for Medical Year 5 (2006/2007)
Diverticulum
• A sac-like protrusion of
mucosa through the
muscular colonic wall
• Protrusion occurs in weak
areas of the bowel wall
where blood vessels
(vasa recta) penetrate
False diverticulum
Contains only mucosa and submucosa covered by serosa
Diverticular disease spectrum
Diverticulosis
Diverticulitis
Diverticular bleeding
Diverticulosis
• Presence of diverticula without
inflammation
Diverticulitis
• Presence of diverticula with inflammation
and subsequent perforation
• Uncomplicated diverticulitis:
• Peridiverticulitis or phlegmon
• Complicated diverticulitis:
• Abscess, fistula, perforation, obstruction
Hinchey classification
• Stage I: pericolic abscess
• Stage II: distant abscess (retroperitoneal/pelvic)
• Stage III: generalized suppurative peritonitis
(abscess ruptured)
• Stage IV: faecal peritonitis (free rupture of a
diverticulum)
Hinchey EJ et al. Adv Surg 1978; 12: 85-109.
Diverticular bleeding
Clinical Approach to LGIB
Covered
already in
previous
lecture!
Prevalence: age
Prevalence increases with age
80%
65%
60%
40%
30%
20%
5%
0%
40
60
80
Age in years
Young-Fadok TM et al. Curr Prob Surg 2000; 37: 459-514.
Prevalence: gender
No apparent sex predilection
Prevalence: geographical variation
‘A disease of western civilization’
High
High
Low
Low
High
High: up to
45%
Low: ~ 0%
Painter NS and Burkitt DP. BMJ 1971; 2: 450-454.
Diverticular disease location
In Asian
populations, >70%
of patients have
diverticula in the
right colon
In European and US
populations, 90%
of patients have
diverticula in the
sigmoid colon and
only 15% have
diverticula in the
right colon
Stollman N and Raskin JB. Lancet 2004; 363: 631-639.
Colonic diverticulosis in HK:
distribution pattern and clinical significance
• 858 DCBE; prevalence 25.1%
Left-sided
only
12.1%
Both
32.6%
Right-sided
only
55.3%
87.9% have right-sided colonic involvement
Chan CC et al. Clin Radiol 1998; 53: 842-844.
Cause and pathogenesis
Colonic wall
weakening
Age-related changes
P
Intraluminal
pressure
Segmentation
Dietary fibre deficiency
Simpson J et al. Br J Surg 2002; 89: 546-554.
Structural changes in colonic wall of
patients with diverticulosis
• Mychosis
• Thickening (neither hypertrophy nor hyperplasia) of the circular
muscle layer
• Shortening of the taeniae coli
• Luminal narrowing
• elastin deposition in taeniae coli
• type III collagen synthesis
• collagen crosslinking
Age-related changes
All these changes lead to an
irreversible state of
contracture and result in
resistance of the colonic wall
Segmentation
Diverticulum
Laplace’s law
Contraction
Contraction
P = k T/R
Painter NS et al. Gastroenterology 1965; 49: 169-77.
Dietary fibre deficiency
• Diverticulosis is a
‘deficiency disease’:
dietary fibre deficiency
Smaller stool volume
Longer transit time
Increases intraluminal
pressure
Painter NS and Burkitt DP. BMJ 1971; 2: 450-454.
Natural history of diverticulosis
Asymptomatic
70
%
Clinical features of diverticulosis
• 70% remains asymptomatic
• Some patients have symptoms of mild abdominal
cramping, bloating, flatulence, irregular bowel habit
• These nonspecific symptoms overlap considerably with
those of irritable bowel syndrome
• Diagnosis: DCBE or colonoscopy
• Treatment: dietary fibre, anticholinergic or antispasmodic
agents
Natural history of diverticulitis
Clinical features of diverticulitis
LLQ pain (93-100%)
Fever (57-100%)
Clinical triad
Leukocytosis (69-83%)
• Generalized peritonitis
• Fistulae to bladder, vagina, or skin
• Intestinal obstruction due to edema, bowel spasm,
compression from an abscess, or stricture after recurrent
attacks
Diagnosis of diverticulitis
• Initial evaluation by Hx, P/E, CBP, urinalysis, and
X-rays (CXR and AXR)
• It has been recommended that when the clinical
picture is clear additional tests are not necessary
to make a diagnosis
• If the diagnosis is uncertain, other tests may be
performed
Other diagnostic tests for diverticulitis
Water-soluble contrast enema
CT scan
DCBE and colonoscopy are contraindicated
during the acute attack
• However, full LB Ix with DCBE or colonoscopy
should be performed when the acute attack has
resolved: to r/o cancer
CT scans of diverticulitis
CT scans of diverticular abscesses
Contained abscess in
sigmoid diverticulitis
Large air-containing
divertciular abscess
Large divertciular
abscess with penetration
into retroperitoneal
structures
Hinchey stage I
Hinchey stage II
Perforated right-sided diverticulitis
Contrast
extravasation
Hinchey stage III
Colovesical fistula
Bladder
Sigmoid
Colovaginal fistula
Sigmoid
Vagina
Coloenteric fistula
Terminal
ileum
Sigmoid
Sigmoid diverticulitis with stricture
Treatment of diverticulitis
• Medical therapy
• Successful in 70-80% of patients
• Percutaneous therapy
• For drainage of pericolic abscess (Hinchey stage I and II)
• Surgical therapy
• Emergency (Hinchey stage III and IV) or elective operation
Medical therapy
• In the absence of systemic symptoms and signs, patients
may be treated on an outpatient basis with low residue
diet and oral antibiotics (7-10 days)
• Hospitalization is required for increasing abdominal pain,
fever, or inability to tolerate oral intake
• Need bowel rest, observation and IV antibiotics
• 70-80% of patients respond to medical therapy –
improvement should be apparent within 48-72 hours
CT-guided drainage of
pericolic abscess
Emergency surgery
• Indications for emergency surgery:
• Failed medical treatment
• Abscess could not be drained by percutaneous
methods
• Generalized peritonitis
• Intestinal obstruction
Natural history of diverticulitis and
elective surgery
Elective surgery
• Indications for elective surgery:
Patients who have had one episode of complicated
diverticulitis (abscess, obstruction, fistula)
Patients who have had two episodes of acute
diverticulitis severe enough to require hospitalization
? Young and immunocompromised patients after one
attack of acute diverticulitis (controversial)
Surgical principles
• Control of sepsis
• Resection of all diseased tissues
• Restoration of intestinal continuity if
possible (with or without protective stoma)
• Minimizing morbidity and mortality
Surgical options
Outdated 3-stage colostomy and drainage
• Hartmann’s procedure
• Primary resection, anastomosis and diversion
• Primary resection and anastomosis (on-table
lavage)
3-stage operation
2-stage operation
First stage
Second stage
Hartmann’s procedure
Resection, end colostomy,
and mucus fistula
Resection, anastomosis, and
proximal diversion
Closure of stoma
1-stage operation
Anastomosis or stoma
• 2 good ends anastomosis
• 2 good ends/poor condition anastomosis +
diversion
• 1 good end/poor condition anastomosis +
diversion
• 2 bad ends Hartmann’s operation
Laparoscopic colectomy for diverticulitis
• Considered to be the procedure of choice for
uncomplicated diverticulitis
• Also feasible for complicated diverticulitis (Hinchey Stage
I and II)