THE LIVER - Orange Coast College
advertisement
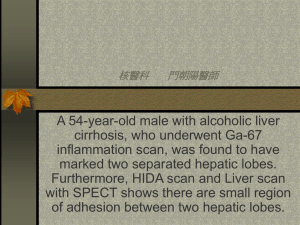
THE LIVER I. Introduction/General Information A. Largest of viscera 1. ~ 2.5% body weight 2. Completely covered by Glisson’s Capsule 3. Incomplete covering by peritoneum General Information, continued … 4. Measurements are ~ a. 21 – 23 cm transverse b. 15 – 18 cm superior to inferior c. 10 – 13 cm anterior to posterior General Information, continued … B. Location: 1. right hypochondrium 2. epigastrium C. Mostly covered by ribs D. Contains numerous vascular structures II. Detailed Anatomy A. Four lobes 1. Divisions based on blood supply, bile drainage 2. Anatomical lobes divided by falciform ligament Inferior View of the Liver A P Detailed Anatomy, con’t… 3. Functional Lobes a. right and left lobes separated by imaginary line b. from fossa for GB IVC Right and Left Functional Lobes of the Liver Left Lobe Right Lobe Detailed Anatomy, continued … B. Functional Divisions 1. Right lobe with caudate process 2. Left lobe: a. Caudate lobe b. Quadrate lobe Caudate Process Detailed Anatomy, continued … C. Fissures: 1. Right sagittal (main) 2. Left sagittal (accessory) 3. Portal 4. Right oblique intersegmental 5. Lateral intersegmental Fissures of the Liver Main lobar fissure Boundary between R and L lobes L.S. on U/S: seen as hyperechoic line from PV to neck of GB Used to ID GB when it is packed with stones Fissures of the Liver Portal fissure T.S. on U/S Created by portal veins (triads) R. main PV is // to anterior body wall Segments of the Liver Hepatic segments I = caudate lobe II & III = superior and inferior lateral segments, L. lobe IV = medial segment, L. lobe V & VI = caudal to transverse plane VII & VIII = cephalad to transverse plane I Functional divisions, continued … 4. Fossae (Superficial) a. IVC – posterior b. Portal Vein – inferior c. Gallbladder – inferior Fossae, Inferior Surface of the Liver Fossa for IVC Fossa for Portal Vein Fossa for Gall Bladder Functional Divisions, continued … 5. Impressions (visceral surface): produced by abdominal viscera a. b. c. d. e. f. Gastric (fundus of stomach) Renal (right kidney) Adrenal (right adrenal gland) Duodenal (bulb of duodenum) Esophageal (esophagus) Right and left colic (flexures of the colon) Visceral Impressions, continued … P •Esophageal •Renal •Gastric •Adrenal •Duodenal •Right colic •Left colic L R A Detailed Anatomy, continued … D. Ligaments 1. Falciform (most superficial anteriorly) a. Divides left lobe in two sections 1. anatomical left lobe 2. caudate & quadrate lobes b. Two layers of peritoneum c. Extends to umbilicus Ligaments, continued … 2. Ligamentum teres hepatis (fetal source??) 3. Ligamentum venosum (fetal source??) 4. Right/Left Coronary Ligaments Hepatic Ligaments Falciform ligament L. coronary ligament L. triangular ligament Ligamentum teres hepatis Ligamentum venosum Ligaments, continued … 5. Hepatophrenic & Hepatorenal ligaments: a. Subdivisions of right coronary ligament b. hepatophrenic (superior) & hepatorenal (inferior) c. Surround BARE AREA Hepatic Ligaments, con’t… Hepatophrenic ligament Hepatorenal ligament Bare Area Detailed Anatomy, continued … E. Lesser Omentum 1. Sleeve-like structure 2. Connects lesser curvature of stomach & bulb of duodenum to inferior surface of liver 3. AKA: Gastrohepatic or Hepatoduodenal ligament Lesser Omentum, continued … 3. Attachment surrounds Porta Hepatis 4. Continues on each side of ligamentum venosum 5. Extends to caudate & left lobes on posterior surface of liver Lesser Omentum Lesser Omentum: (R) Anterior view, (L) Inferior view Detailed Anatomy, con’t… E. Subphrenic Spaces 1. clinically important 2. common sites for abscesses 3. Between liver and diaphragm Subphrenic Spaces, con’t… 4. Right superior posterior subphrenic space a. Boundaries: - superior: right coronary ligament - anterior: liver - posterior: parietal peritoneum covering diaphragm b. Extends inferiorly to…. Subphrenic Spaces, continued … 5. Right posterior inferior subphrenic space a. Boundaries - above: inferior surface of liver - below: transverse colon & mesocolon b. Extends over right adrenal & kidney Subphrenic Spaces, continued … c. AKA: Hepatorenal Pouch/Recess, Morrison’s Pouch d. Patient lying supine: 1. Lowest part of peritoneal cavity is behind liver 2. Fluid, pus, etc. collects here 3. Can cause abscess formation Subphrenic spaces, continued … 6. Right superior anterior subphrenic space a. Boundaries: - right side of falciform ligament - upper layer of right coronary ligament - underside of diaphragm - superior surface of liver b. Found when patient lying prone Subphrenic spaces, continued … 7. Most sources of peritoneal contamination are on the right 8. Right posterior & right inferior spaces are most significant sites 9. Infection may spread via diaphragmatic lymphatics Detailed Anatomy, continued … F. Porta Hepatis: contains the following structures 1. Hepatic arteries a. Usually two, sometimes one b. Originate from common/proper hepatic artery c. Course is variable Porta Hepatis, continued … 2. Portal vein (supplies 1100 ml/blood per minute) a. Largest structure in porta b. Formed by confluence of mesenteric veins & splenic vein Porta Hepatis Hepatic Artery Portal Vein Common Bile Duct Porta Hepatis, continued … 3. Hepatic & cystic ducts 4. Nerves: a. Vagus X (parasympathetic) b. Fibers from celiac ganglion Porta Hepatis, continued … 4. Lymph nodes: a. most hepatic lymph vessels end in nodes around porta hepatis b. From here, drain into celiac nodes Porta Hepatis, continued … c. Some vessels pass through falciform ligament 1. through diaphragm 2. into mediastinal nodes d. enlarged nodes may compress portal vein or hepatic duct Detailed Anatomy, continued … G. Vascular Structures in Liver 1. Largest vessels are portal vein and IVC a. Portal Vein: 1. appears on T.S. as tubular, echolucent structure 2. courses horizontally from porta hepatis Detailed Anatomy, continued … 3. walls echogenic due to structures in portal triad b. Left Portal Vein: 1. has more variable course 2. May be difficult to trace on transverse scans Hepatic Vessels IVC Right Portal Vein Left Portal Vein Main Portal Vein Vascular Structures, continued … c. Right Portal Vein: 1. anatomical landmark 2. extends into right lobe 3. branches after porta hepatis 4. L.S. shows “dumbbell” or circular structure with echogenic “collar” Computer-enhanced image of RPV, L.S. Computer-enhanced 3-D image of RPV, L.S. Vascular Structures, continued … d. IVC: 1. To right of aorta 2. Appears to pass through liver 3. Diameter enlarges after renal veins join (~L-1) Computer-enhanced 3-D image of Hepatic Vessels Vascular structures, continued … 2. Hepatic Veins: a. Tubular structures b. Enlarge cephalad c. In superior half of liver d. Angles of hepatic vein branches oriented toward IVC e. Walls not echogenic Hepatic Veins R. Hepatic Vein Middle Hepatic Vein L. Hepatic Vein Detailed Anatomy, continued … A. Bile Ducts 1. No “normal” anatomy 2. If dilated: a. Echogenic collar b. Lobulated shape c. Highly branched over short distances d. Converge toward porta hepatis Anatomy of the Biliary System (yeah, right…) P L R A III. Hepatic Masses A. May be cystic, solid, or complex B. Simple Cysts 1. solitary or multiple 2. sonolucent 3. well-defined margins 4. exhibit posterior acoustic enhancement 5. Congenital cysts may contain cellular debris Simple Cysts, Hepatic Masses, continued … 6. Polycysts: usually accompany cysts of kidney, spleen, and/or pancreas 7. Appearance: a. Wall is distinct, sharp border, crisp edges b. Shape: spherical Hepatic Masses, continued … C. Complex Masses 1. With central necrosis: irregular walls a. Associated with metastases from rapidly-growing neoplasms b. Blood supply can’t supply tumor growth c. Central part of mass becomes necrotic Complex Masses,Hepatic Masses, continued … 2. With cellular or inflammatory debris: a. walls are irregular b. Associated with hepatic abscess c. Internal bacterial infection 3. Due to echinococcal disease: a. Show irregular wall thickness b. Parasitic bacteria in sheep feces Complex Masses, continued … 4.Hematoma: ill-defined borders, sonolucent-to-complex masses a. Early: appears sonolucent b. After clot forms, echogenic c. Due to liver trauma Hepatic Masses, continued … D. Solid Masses often represent carcinomas 1. Hepatoma: primary liver cancer a. Central necrosis may be present b. Tumor thrombus may be detected impinging on major veins Solid Masses, Hepatic Masses, continued … 2. Metastatic Liver Disease a. “Bull’s Eye” or “Target” pattern [adenocarcinoma of GI Tract] b. Adenocarcinomas from other sources more echogenic c. Sonolucent metastases from lymphomas, sarcomas more complex IV. Parenchymal Disorders A. Sonographic appearance: non-specific 1. Stroma = supportive connective tissue 2. Parenychma = functional tissue 3. Most liver tissue is parenchyma Parenchymal disorders, continued … B. Cirrhosis: Most common 1. Due to hepatitis or alcoholism 2. Sonographic appearance: a. Moderately echogenic b. Liver denser than normal c. Due to formation of scar tissue Cirrhosis, Sonographic appearance, continued … c. Peripheral intrahepatic vessels indistinct 1. reduced blood supply 2. peripheral vessels obscured by scar tissue Cirrhosis, Sonographic appearance, continued … d. Lobes may show reduced size: 1. right lobe is more affected 2. left lobe enlargement a. compensation b. decreased function of right lobe Cirrhosis, Sonographic appearance, continued … e. As scar tissue develops, blood flow is affected 1. Blood backs up 2. Spleen and splenic vein enlarge e. Portal Hypertension Cirrhosis, Sonographic appearance, continued … f. Liver margin: 1. indentations 2. changes in contour 3. blunted edges 4. may be observed on U/S Cirrhosis, Sonographic appearance, continued … g. Increased incidence of hepatoma in advanced cirrhosis h. detection of ascites aids in differential diagnosis 1. Ascites: fluid in peritoneal cavity 2. Due to portal HTN Parenchymal Disorders, continued … C. Fatty Replacement (prior to cirrhosis) 1. Appearance similar to cirrhosis 2. May be initial stage of cirrhosis 3. Difference: a. Intrahepatic vessels remain clearly defined b. No portal HTN V. Other Diseases and Conditions A. Congestive Hepatomegaly: 1. Enlargement of liver secondary to congestive heart failure 2. Homogeneous: liver rarely shows echo changes 3. Tissue attenuation may decrease as liver fills with blood Other Disease Conditions, continued … 4. Marked dilation of IVC without respiratory influence is proof of right heart failure 5. Hepatic vein branches may show enlargement Other disease conditions, continued … 6. Thrombosis of IVC may show similarities -thrombus can be detected 7. Other signs: a. Ascites b. dilation of right atrium Other diseases and conditions, continued … B. Liver Abscesses: 1. Commonly found in hepatorenal pouch 2. Appear cystic with irregular borders and fine precipitates Other Disease Conditions, continued … C. Obstructive Jaundice: 1. Result of obstruction of bile flow 2. Dilation of intrahepatic bile ducts 3. Ultrasound can differentiate between obstructive and hepatocellular jaundice Dilated CBD: seen in Obstructive Jaundice Other Disease Conditions, continued … D. Hepatic Artery Aneurysm: 1. May stimulate hepatic abscess 2. Usually appears as sonolucency with surrounding echogenic area (thrombus) 3. Flow of blood changes as blood swirls and clots Other Disease Conditions, continued … E. Klatskin Tumor: 1. Ducts are blocked or fused a. Tumor at junction of Right and Left Hepatic Ducts b. Causes obstructive jaundice Other Disease Conditions, continued … F. Courvasier’s Sign: 1. Refers to gallbladder “rate of fill” with tumor vs. stone 2. Hydrops (edema) of gallbladder due to tumor in head of pancreas Other Disease Conditions, continued … G. Reidel’s Lobe: 1. Anomalous, tongue-like extension 2. From right lobe of liver to the gallbladder Reidel’s Lobe R. Lobe L. Lobe GB Reidel’s Lobe Reidel’s Lobe VI. Miscellaneous Data A. Portal Vein: Measurements 1. Length = 5.5 – 8.0 cm (average = 6.5) 2. Diameter = ~ 1 cm Misc. Data, continued … B. Ampulla of Vater 1. Length = 1 – 14 mm 2. Width = 1.5 – 4.5 mm