Severe Sepsis - UNM Hospitalist Group / FrontPage
advertisement

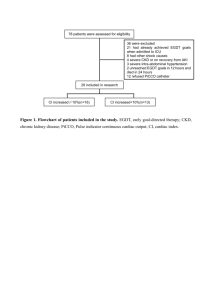
Reducing Sepsis Mortality Richard Crowell, MD Senior Vice Chair Department of Internal Medicine Professor and Chief Pulmonary, Critical Care, and Sleep Medicine UNM School of Medicine Objectives • Discuss pathophysiology and treatment of sepsis and septic shock, and advent of Early Goal-Directed Therapy • Describe approach to Early Goal-Directed Therapy at UNM Hospital: SMITe Severe Sepsis vs. Other Critical Illnesses In the US, more than 500 patients die of severe sepsis daily (Angus, Crit Care Med 2001) Condition Prevalence Deaths Mortality AMI (1) 900,000 225,000 25% Stroke (2) Trauma (3) 700,000 163,500 23% 2.9 million 42,643 1.5% 751,000 215,000 29% (Motor Vehicle) Severe Sepsis (4) Source: (1) Ryan TJ, et al. ACC/AHA Guidelines for management of patients with AMI. JACC. 1996; 28: 1328-1428. (2) American Heart Association. Heart Disease and Stroke Statistics – 2005 Update. Available at: www.americanheart.org. (3) National Highway Traffic Safety Administration. Traffic Safety Facts 2003: A Compilation of Motor Vehicle Crash Data from the Fatality Analysis Reporting System and the General Estimates System. Available at http://www.nhtsa.dot.gov/. (4) Angus DC et al. Crit Care Med 2001;29(7): 1303-1310. Age Related Incidence of Severe Sepsis 25 20 60,000 15 40,000 10 20,000 5 0 0 85 80,000 <1 1-4 510 9 -1 15 4 -1 20 9 -2 25 4 -2 30 9 -3 35 4 -3 40 9 -4 45 4 -49 50 -5 55 4 -5 60 9 -6 65 4 -69 70 -7 75 4 -7 80 > 9 -84 No. of Cases 100,000 Cases Incidence Incidence (per 1000 pop) 30 120,000 Age (y) Angus DC, et al. Crit Care Med. 2001. Sepsis: A Complex Disease Other Sepsis Pancreatitis Infection Severe Sepsis SIRS Trauma Burns Adapted from: Bone RC et al. Chest. 1992;101:1644-55. Used with permission, S.Simpson, MD, KU, 2008 Sepsis: A Deadly Continuum SIRS • A clinical response arising from a nonspecific insult, with 2 of the following: • T >38oC or <36oC • HR >90 beats/min • RR >20/min • WBC >12,000/mm3 or <4,000/mm3 or >10% bands Sepsis SIRS with a presumed or confirmed infectious process Severe Sepsis Sepsis with organ dysfunction Shock Septic Refractory Hypotension Related to Sepsis Chest 1992;101:1644. Natural History of SIRS • Prospectively enrolled 2527 patients who met SIRS criteria • Followed for 28 days or discharge for development of any stage of the sepsis continuum Incidence (No. pts, (%)) Mortality (%) No progression 1301 (52%) 7% Sepsis 649 (26%) 16% Severe Sepsis 467 (18%) 25% Septic Shock 110 (4%) 46% •Note: median interval from SIRS to sepsis was inversely related to number of SIRS criteria Rangel-Frausto MS, et.al. JAMA 273:117-23, 1995 Prognosis based sepsis severity Mortality Severe Sepsis: 20-35% Septic shock: 35-60% Figure B, page 948, reproduced with permission from Dellinger RP. Cardiovascular management of septic shock. Crit Care Med 2003;31:946-955. Clinical Alterations in Severe Sepsis • Vasculopathy • Loss of regional autoregulation • Vasodilation • Relative intravascular hypovolemia • Cardiopathy • ↓ contractility, ↑ compliance • ↑ CO, but ↓ EF • Acute organ dysfunction • Toxin and cytokine actions on vascular / tissue barriers Inflammatory Mediators Cardiovascular Insufficiency Global Tissue Hypoxia Increased Metabolic Demands O2 Demand Hypovolemia Vasodilation Myocardial Depression Microvascular Alterations Used with permission, S.Simpson, MD, KU, 2008 O2 Delivery After Fink. Crit Care Clin 2002. Acute Organ Dysfunction as the Hallmark of Severe Sepsis Altered Consciousness Confusion Psychosis Tachycardia Hypotension Tachypnea PaO2 <70 mm Hg SaO2 <90% PaO2/FiO2 300 Oliguria Anuria Creatinine Jaundice Enzymes Albumin PT Platelets PT/APTT Protein C D-dimer Lactic acidosis Used with permission, S.Simpson, MD, KU, 2008 Treatment of Sepsis • Address cause: Treat infection • Intravascular volume resuscitation • Cardiovascular support • Support of dysfunctional organ systems Figure 2 Has the mortality of septic shock changed with time? Friedman, Gilberto; Silva, Eliezer; Vincent, Jean-Louis; MD, PhD Critical Care Medicine. 26(12):2078-2086, December 1998. . Time Sensitive Interventions • Patients enrolled on entry into ED • Evidence of Infection • Met SIRS criteria • Hypotensive OR • Lactic acidosis (>4 mmol/L) • Rapid recognition • Protocol of treatment w/in 6 hours: • Cultures and appropriate antibiotics • Fluid resuscitation to CVP 8-12 • Cardiovascular support with pressors, augmented O2 delivery The Importance of Early Goal-Directed Therapy for Sepsis Induced Hypoperfusion NNT to prevent 1 event (death) = 6-8 Mortality (%) 60 50 Standard therapy EGDT 40 30 20 10 0 In-hospital mortality (all patients) 28-day mortality 60-day mortality Adapted from Table 3, page 1374, from Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 2001; 345:1368-1377 Surviving Sepsis Campaign www.survivingsepsis.org Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock 2012 Crit Care Med 2013; 41:580-637 Institute for Healthcare Improvement www.IHI.org Early Goal-Direct Therapy (EGDT) EGDT is designed to: Recognize patients with severe sepsis as early as possible and begin treatment quickly Assess laboratory and clinical variables for acute organ dysfunction, hemodynamic instability Delineate time targets for delivery of treatment of patients with sepsis Develop hospital-specific bundled protocols Earlier treatment leads to better outcomes Surviving Sepsis Campaign Recommendations for EGDT Bundle Bundles should be developed based on the systems and expertise available to providers Goal: perform all indicated tasks 100% of the time within the first 6 hours of identification Good Evidence-based Data for EGDT • Mortality improvement • Use of lactate as severity and prognostic indicator • Bundled protocols improve outcomes • But not all individual bundle elements have been shown to specifically improve mortality • Early and appropriate antibiotics • Aggressive fluid resuscitation improve outcomes • But how much fluid? • Enough to improve end organ dysfunction • But not too much… Best current, generally available measure of Global Tissue Hypoxia is Lactate • What is role of lactate ? • Patient assessment • Assigning prognosis • Guiding treatment decisions Serum Lactate as a predictor of mortality in patients with infection •Retrospective analysis of patients with dx of infection and lactate measured •Did not evaluate +/- shock Trzeciak S, et.al. Intensive Care Medicine 33:970-77, 2007 Lactate is associated with mortality in Severe Sepsis Independent of organ failure and shock Prospective cohort study Critical Care Medicine. 37(5):1670-1677, May 2009. © 2009 Lippincott Williams & Wilkins, Inc. Published by Lippincott Williams & Wilkins, Inc. 4 Figure 3. Lactate is associated with mortality in Severe Sepsis Independent of organ failure and shock Critical Care Medicine. 37(5):1670-1677, May 2009. © 2009 Lippincott Williams & Wilkins, Inc. Published by Lippincott Williams & Wilkins, Inc. 7 Lactate is associated with mortality in Severe Sepsis Independent of organ failure and shock 2. Critical Care Medicine. 37(5):1670-1677, May 2009. © 2009 Lippincott Williams & Wilkins, Inc. Published by Lippincott Williams & Wilkins, Inc. 6 Good Evidence-based Data for EGDT • Mortality improvement • Use of lactate as severity and prognostic indicator • Bundled protocols improve outcomes • Even though not all individual bundle elements have been shown to specifically improve mortality • Early and appropriate antibiotics • Aggressive fluid resuscitation improve outcomes • But how much fluid? • Enough to improve end organ dysfunction • But not too much… EGDT: Bundled approaches to protocols • Use is evidence-based: • Combine multiple effective elements • Outcome is additive or synergistic • Framework that leverages change • Avoids a piecemeal approach Do Bundles Work? Gao, et al. Critical Care 2005, 9:R764-R770. With Permission from S. Simpson, MD,, Kansas University, 2008 A. All subjects with Severe Sepsis/Septic Shock B. Only subjects with Septic Shock Multicenter implementation of a severe sepsis and septic shock treatment bundle. Miller RR, et.al. Am Journal Respir Crit Care Med, 2013; 188, 77-82 Good Evidence-based Data for EGDT • Mortality improvement • Use of lactate as severity and prognostic indicator • Bundled protocols improve outcomes • Even though all individual bundle elements have not been shown to specifically improve mortality • Early and appropriate antibiotics • Aggressive fluid resuscitation improve outcomes • But how much fluid? • Enough to improve end organ dysfunction • But not too much… Good Evidence-based Data for EGDT • Mortality improvement • Use of lactate as severity and prognostic indicator • Bundled protocols improve outcomes • But not all individual bundle elements have been shown to specifically improve mortality • Early and appropriate antibiotics • Aggressive fluid resuscitation improve outcomes • But how much fluid? • Enough to improve end organ dysfunction • But not too much… Timeliness of Antibiotics in Septic Shock • Kumar, et.al. reviewed medical records of 2731 adults with septic shock over 25 years in Manitoba, Canada • Focused on 2,154 patients who received Ab ONLY after onset of hypotension • Clinical site infections • 37.2% lung • 29.3% intraabdominal • 10.7% genitourinary • Documented infection (by cx) in 78% of cases • Others by definitive xray, surgical, biopsy, or autopsy evidence • Microbiology: Gram (-) 47.9%, Gram (+) 38.3% Kumar A, et.al. Crit Care Med 34:1589, 2006 Kumar et al, CCM. 2006:34:1589-96 Septic Shock: Timing of Antibiotics Percent of total pts 1.00 % Survival % Total receiving antibiotics 14 ICUs; n = 2,731 .80 .60 50% of patients in Septic Shock Only received antibiotics w/in 6 hrs. .40 .20 0.0 Time (hrs) from hypotension onset Timeliness of Antibiotics in Septic Shock • Antibiotics w/in first hour: 79.9% survival • Every hour delay decreased survival by 7.6% • OR of in-hospital mortality increased by 12% for each hour delay in administration • In Multivariate analysis: • Time to antimicrobial therapy most strongly associated with survival • Others: APACHE score, volume of fluid in first hour of resuscitation •Kumar A, et.al. Crit Care Med 34:1589, 2006 Antibiotic administration, UNMH ED → MICU May 1, 2011 thru May 31, 2012; 296 total cases Mortality (%) * Percent of Bundle patients who received Ab in this time frame % patients Ab <3hrs Antibiotics in < 3 hrs 100 Percent 80 60 40 20 0 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Month With Permission of Jon Femling, MD A n tib io tic s < 6 0 m in u te s 100 The challenge Antibiotics within 60 minutes is the goal. As this data reveals we meet this goal less than 50% of the time. P e rc e n t 80 60 40 20 0 6 7 8 9 10 11 12 13 14 15 M o n th With Permission of Jon Femling, MD Time to Antibiotics Percent of patients who receive Antibiotics in less than 1 Hour (monthly) 80 Percent 60 40 20 6/11 9/11 12/11 3/12 6/12 9/12 12/12 Month Intervention begins 3/13 Time to Antibiotics (individual patients) March - present, 2013 Minutes July 2012 – Feb 2013 88 min 66 min Individual patients Intervention begins Good Evidence-based Data for EGDT • Mortality improvement • Use of lactate as severity and prognostic indicator • Bundled protocols improve outcomes • But not all individual bundle elements have been shown to specifically improve mortality • Early and appropriate antibiotics • Aggressive fluid resuscitation improve outcomes • But how much fluid? • Enough to improve end organ dysfunction • But not too much… Cardiovascular Resuscitation-Based EGDT Lin, et.al. 2006 • 241 consecutive patients enrolled, randomized to protocol vs no protocol • Protocol focused on rapid fluids to: • 1) attain CVP ≥ 8-12 then 2) MAP ≥ 65 (pressors, steroids as needed) then • 2) urine output ≥ 0.5 ml/kg/hr • All patients got antibiotics per clinician; no differences in groups Lin SM, et.al. Shock 6:551-7, 2006 Cardiovascular Resuscitation-Based EGDT Outcome Protocol (n=108) No Protocol (n=116) p 53.7 % 71.6% 0.006 Shock reversal (hrs) 47 ± 22.8 65.4 ± 32.1 0.006 Resuscitation fluids 136.2 ± 119 88.6 ± 57.7 0.034 78 22.2 104.4 29 0.001 Length of ICU stay 14.3 ± 11.7 20.3 ± 16.6 0.003 Renal failure 42 (38.9%) 64 (55.2%) 0.015 CNS failure 20 (18.5%) 42 (36.2%) 0.003 Hosp Mortality Time to pressors Lin SM, et.al. Shock 6:551-7, 2006 Good Evidence-based Data for EGDT • Mortality improvement • Use of lactate as severity and prognostic indicator • Bundled protocols improve outcomes • But not all individual bundle elements have been shown to specifically improve mortality • Early and appropriate antibiotics • Aggressive fluid resuscitation improve outcomes • But how much fluid? • Enough to improve end organ dysfunction • But not too much… Successful fluid resuscitation in EGDT • What are appropriate endpoints for “successful” volume resuscitation? • Depends on “volume responsiveness” • where is the patient on the Starling curve? • CVP: may not be best measure for volume responsiveness • Pulse pressure variation: accurate only in nonspontaneously breathing patients • IVC diameter before/after fluid challenges: limited by body habitus Is optimization of oxygen delivery/utilization necessary for successful EGDT? • Is ScVO2 the appropriate surrogate measure for optimizing oxygen delivery/utilization in septic shock? • Role of transfusion, inotropic support • Can lactate clearance be used as a measure of successful EGDT ? Surviving Sepsis Campaign: Early Recognition is Crucial!!! • Use of screening tools improves overall awareness, educates, and increases recognition • UNM: • Wards/MICU: qshift screening by nursing staff • ED: Triage nurses, EMS do initial evaluation Figure 1 Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock: 2012 Dellinger, R. Phillip; Levy, Mitchell M.; Rhodes, Andrew; Annane, Djillali; Gerlach, Herwig; Opal, Steven M.; Sevransky, Jonathan E.; Sprung, Charles L.; Douglas, Ivor S.; Jaeschke, Roman; Osborn, Tiffany M.; Nunnally, Mark E.; Townsend, Sean R.; Reinhart, Konrad; Kleinpell, Ruth M.; Angus, Derek C.; Deutschman, Clifford S.; Machado, Flavia R.; Rubenfeld, Gordon D.; Webb, Steven A.; Beale, Richard J.; Vincent, Jean-Louis; Moreno, Rui; and the Surviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup Figure 1. Surviving Sepsis Campaign Care Critical Care Medicine. 41(2):580-637, February 2013. Bundles. doi: 10.1097/CCM.0b013e31827e83af Copyright © 2013 Critical Care Medicine. Published by Lippincott Williams & Wilkins. 49 Table 2 Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock: 2012 Dellinger, R. Phillip; Levy, Mitchell M.; Rhodes, Andrew; Annane, Djillali; Gerlach, Herwig; Opal, Steven M.; Sevransky, Jonathan E.; Sprung, Charles L.; Douglas, Ivor S.; Jaeschke, Roman; Osborn, Tiffany M.; Nunnally, Mark E.; Townsend, Sean R.; Reinhart, Konrad; Kleinpell, Ruth M.; Angus, Derek C.; Deutschman, Clifford S.; Machado, Flavia R.; Rubenfeld, Gordon D.; Webb, Steven A.; Beale, Richard J.; Vincent, Jean-Louis; Moreno, Rui; and the Surviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup Critical Care Medicine. 41(2):580-637, February 2013. doi: 10.1097/CCM.0b013e31827e83af TABLE 2. Severe Sepsis Copyright © 2013 Critical Care Medicine. Published by Lippincott Williams & Wilkins. 50 UNM 6 Hour Sepsis Resuscitation Bundle Completed ASAP (w/in 6 hrs) after (+) SIRS/Sepsis screen 1. Organ function labs, Serum lactate measured 2. Blood Cultures obtained 3. Appropriate antibiotics administered (within 1 hr) UNM 6 Hour Sepsis Resuscitation Bundle Completed ASAP (w/in 6 hrs) after (+) SIRS/Sepsis screen 4. If Lactate >4, SBP<90, MAP <65, or SBP >30mm decrease from baseline: a. Give 30 ml/kg IVF bolus b. Transfer to MICU UNM 6 Hour Sepsis Resuscitation Bundle Completed ASAP (w/in 6 hrs) after (+) SIRS/Sepsis screen 5. Place central venous catheter 6. Apply vasopressors for hypotension not responding to initial fluid resuscitation to maintain mean arterial pressure > 65 mmHg • Norepi, then vasopressin • Avoid dopamine 7. Consider SvO2 measurement, improve oxygen delivery if <65-70% Identification of sepsis severity !! 3 pathways Green (sepsis) Yellow (lactate 2-4) Red (severe sepsis or septic shock) • Protocol was based on literature and input from all areas involved • Several revisions before consensus Electronic Order Set IHI Severe Sepsis Collaborative Expanded SMITe to ED • Fall 2009 Joined IHI collaborative • Aims: • Improve ED recognition of severe sepsis • Facilitate transfers to the MICU • Improve communication between both units • ED-specific screening tool for triage • Concurrent patient tracking • Still have twice-monthly group meeting “If you’re not keeping score, you’re just practicing” EGDT: Outcomes Measures • Establish institutional data baselines “where are we starting from?” • UNM: In 2007 ~38% of all deaths on Medicine service were coded for sepsis or infection as primary cause of death • Severe sepsis/septic shock mortality: 46% Our ED->MICU EGDT Performance (2/12 -5/13) ~24 patients / month 30% Mortality With Permission of Jon Femling, MD Lactate Cultures Fluids Antibiotics Pressors CVP 100% 94% 97% 88% 79% 68% Observed Severe Sepsis Mortality % Mortality Adult Severe Sepsis Observed Severe Sepsis: UNMH Mortality Index (O/E Ratio) Documentation of Disease Severity: Severe Sepsis/Septic Shock • Severe sepsis w/o MV 96+ hours with MCC • DRG 871 RW: 1.9090 Est. Payment: $17,654 • Severe sepsis w/o MV 96+ hours without MCC • DRG 872 RW 1.1339 Est. Payment: $10,486 61 Severity of Illness and Risk of Mortality Comorbidity and/or Complication (CC) • Comorbitidy: A pre-existing condition/illness that will cause an increase in length of stay because of its presence with the condition that caused the admission. • Complication: A condition that arises during the hospital stay that may prolong the length of stay. • Major comordibity/complication (MCC) 62 MCCs for Sepsis Example of MCCs for Sepsis •Respiratory Failure due to Sepsis • • • • Acute Respiratory Failure Lung Abcess Empyema Ventilator Dependent (can’t use unable to wean) 63 Summary of recent data on EGDT • EGDT bundle completion improves mortality • Antibiotics within 1 hour saves lives • Hospital-derived Sepsis much higher mortality than if present on admission • UH Sepsis mortality NOT POA 2x that if Present On Admission (PAO) Brought to you by SMITe Sepsis Mortality Improvement Team at UNM