Sepsis and Septic Shock 2011 - st. james healthcare education
advertisement

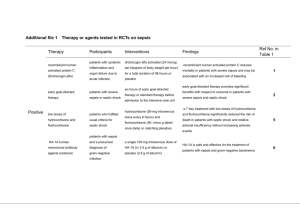
Sepsis and Septic Shock Dr. John Pullman St. James Healthcare Butte, Montana 2011 Microbiology of Sepsis Common gram-positive cocci are Strep pneumonia, Staph aureus (MSSA & MRSA), gp A & B strep, gp G strep; strep anginosis. Aerobic gram-negatives are E. coli, Klebsiella, and other Enterobacteriacae (Lipid A) Gram-positive anerobes are Clostridia (toxinproducing) & rarely Fusobacterium CAP and Sepsis 37 yr old woman presents with 5 day h/o fever, cough, dysnea and pleuritic chest pain. No hx of prior lung disease or pneumonia. No major medical illnesses or surgeries. Temp 104.6 BP 70/45, HR 130, RR 40, O2 sat 76% RA. Exam and CXR reveal RLL, RML, LLL consolidation & large R pleural effusion. pH 7.12, pCO2 56, pO2 56. What most likely would a gram stain of sputum show? What are the most likely organisms to cause CAP? What guides antibiotic choices initially? Purpura Fulminans 26 yr old woman with a history of ‘congenital splenic dysplasia’ presents with temp 104 F, BP 88/50, HR 124, RR 36. Recent URI and cough. She develops purpuric lesions on the acral points of her body. WBC is 4200, Hgb 11, platelet count is 15,000. CXR shows lobar pneumonia. What is her most likely condition? Fever, Rash, and Hypotension 30 yr old woman referred for evaluation of a perineal cellulitis culture + for MRSA. Rash developed on oral TMP/SMX and pt transferred to your hospital. Steroids started. Temp is 104 F, BP 92/56, HR 128, RR 32; there is a diffuse macular rash on trunk and extremities; perineum is red and ulcerated. Is this shock? What kind? What else is wrong? Fever, Limb Pain, and Hypotension 18 yr old man with hep C cirrhosis from infancy presents with temp 103 F, BP 92/54, HR 120, RR28. He has chronic lymphedema of both legs but has severe pain in his right calf. WBC is 20,000, Hgb 11, platelet count is 52000. CPK is 4200. BUN is 65 and creatinine is 3.2. Last creatinine 3 months ago was 1.0. What type(s) of septic shock is this likely to be ? Is this a surgical disease? What antibiotics should be ordered? What principles guide your selection? Fever & Hypotension NOS 65 yr old man presents with fever, BP 84/52, HR 116, RR 30. There are no focal symptoms or signs. After 24 hours, temp is still 104 F on vancomycin and ceftriaxone. What next? 32 yr old woman brought to ER by ambulance confused, febrile, and hypotensive. Minimal findings on exam; has a dorsal laceration of her hand with minimal redness. What history is pertinent? What requests do you make of micro? 80 yr old woman brought to ER from SNF for acute confusion, temp 101 F, and BP 96/60, HR 110. No hx available and CXR is ‘clear’. After blood work is drawn, what next? 56 yr old man with rheumatoid arthritis presents with fever and hypotension. He is on TNF antagonist. Why does that matter? Vasopressors and Septic Shock Recent prospective MC/DB randomized trial found no difference in 28 day mortality between dopamine (DA) and norepinephrine (NE) in treatment of shock. Dysrhythmias were more common with DA. DA-induced tachycardia was associated with increased ischemic events; cardiogenic shock had higher mortality rate with DA. Norepinephrine should be first line in septic shock After adequate volume resuscitation, if NE-treated patients have MAP<65-70, add fixed dose vasopressin (0.03 units/min) and IV hydrocortisone (50 mg q6hrs). Sepsis and Respiratory Failure 72 yr old man presents with abdominal pain, temp 102 F, BP 70/44, HR 120, RR 40. Abd/Pelvic CT confirms peri-diverticular abscesses with air-fluid levels and percutaneous catheter drainage is performed. Arterial lactate level is high, creatinine is 3.0 after volume resuscitation. On AM of his third day, he develops increasing confusion and dysnea despite CPAP mask. ABGs: pH 7.20, pCO2 38, pO2 84 on high flow O2. CXR shows new ‘bibasilar and perihilar’ lung infiltrates. Is this hospital-acquired pneumonia? What else could it be? Serum Cortisol and Sepsis Surviving Sepsis Campaign Goal-Directed Rx in the First 6 Hours Blood cultures before antibiotic therapy Volume resuscitation Imaging studies promptly to confirm source of infection Administration of broad-spectrum antibiotics within 1 hour of diagnosis of septic shock and for 7-10 days Source control after R/B analysis of methods needed Surviving Sepsis Campaign Goal-Directed Rx in the First 6 Hours Vasopressor followed by stress dose corticosteroids Low TV/ low peak pressure ventilation with PEEP if ALI/ARDS Targeting blood glucose 140-180 after stabilization VAP prevention bundle Don’t Let It Sneak Up On You! 17 yr old girl goes to walk-in clinic with 5-7 day h/o sore throat, fever, swollen cervical LN and myalgias. Rapid strep test + and amoxacillin prescribed. A diffuse macular rash develops on her trunk. What lab test would you order now? She is re-assured, given analgesics, and sent home. 3 days later she presents with Temp 104, BP 80/40, HR140, RR 36. WBC 4000, plt count 45,000 SEPSIS True or False True or False Sepsis and septic shock are synonymous. Bacteremia is always followed by sepsis. Gram positive sepsis has replaced gram negative sepsis in frequency Septic emboli to the lungs should be treated with antibiotics and full anti-coagulation Pneumonia, soft tissue infx, UTIs, and intra-abdominal infx are common causes of sepsis True or False MRSA sepsis is more common than Strep pneumonia sepsis. E. coli sepsis is often from an intra-abdominal or urinary tract source. Klebsiella more often than E coli can cause pneumonia –associated sepsis. Vasopressor preferences in sepsis are absolutely defined by practice guidelines. Norepinephrine is generally preferred over dopamine for septic shock refractory to fluid resuscitation. Vasopressin can play a role as an adjunctive Rx in shock. True or False Source control of infection can often wait until Monday if a patient in septic shock is admitted on a preceding Friday. Bactericidal antibiotics are preferred over bacterostatic antibiotics for patients with sepsis or septic shock. Vancomycin is often the antibiotic of choice in the ICU for suspected gram positive infections. Azithromycin in combination with ceftriaxone is recommended in CAP over ceftriaxone alone on the basis of prospective randomized controlled multi-center trials. CAP patients admitted to ICU should get the same antibiotics recommended for medical floor CAP patients if on telemetry. True or False Group A streptococcal toxic shock and necrotizing fasciitis is a purely medically managed condition. Staphylococcal toxic shock syndrome is always associated with staphylococcal bacteremia or necrotizing fasciitis. Positive blood cultures for Staph aureus (MSSA or MRSA) after 48-72 hours of high-dose vancomycin are a poor prognostic sign. E coli has been cultured from the urinary tract after 3 days of high dose levofloxacin in cases of septic shock from E coli pyelonephritis. Surviving sepsis guidelines work best when a team approach is respected by everyone involved in the care of a septic pt.